Abstract
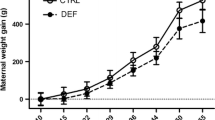
Data from our previous work indicate that Lamotrigine (LTG) is teratogenic in the mouse. In the present study, we attempted to determine the possible protective effects of exogenous folate on LTG-induced fetal anomalies in TO mouse. Experiment I entailed administering 4 mg/kg of folinic acid (FA) and (25 mg/kg) of LTG intraperitoneally three times on gestation day (GD) 8 to a group of mice; other groups were a group that received similar volumes of saline, a group that received LTG and Saline, a group that received FA and saline. Experiment 2 involved administering groups of mice with daily 3 doses FA (or proportionate volume of saline) on GD 5 through 10 and either 3 doses of saline on GD8, or 3 doses of LTG on GD8. Maternal plasma concentrations of FA, vitamin B12 and homocysteine were determined an hour after the last injection from one-half of all animals. The other half were allowed to go to term (GD18) when they were euthanized and their fetuses were examined for visceral and skeletal malformations. A high incidence of resorption, abortion, embryolethality, congenital malformations, and intrauterine growth restriction (IUGR), was observed in the LTG-treated group. Folic acid and B12 levels were decreased and homocysteine concentration increased significantly in LTG groups. Mice receiving LTG with FA had normal levels of folate, Vitamin B12 and homocysteine levels, and the fetuses had fewer birth defects similar to the controls which were given saline only. Supplemental FA ameliorated to a great extent the LTG-induced embryonic resorption and malformations and restored the FA status.





Similar content being viewed by others
References
Holmes LB, Hernandez-Diaz S (2012) Newer anticonvulsants: LTG, topiramate and gabapentin. Birth Defects Res A 94(8):599–606
Tomson T, Battino D, Bonizzoni E, Craig J, Lindhout D, Sabers A, Perucca E, Vajda F (2011) Dose-dependent risk of malformations with anti-epileptic drugs: an analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol 10(7):609–617
Morrell MJ (2002) Folic acid and epilepsy. Epilepsy Curr 2(2):31–34
Linnebank M, Moskau S, Semmier A, Widman G, Stoffel-Wagner B, Weller M, Elger CE (2011) Antiepileptic drugs interact with folate and vitamin B12 serum levels. Ann Neurol 69(2):352–359
Pittschieler S, Brezinka C, Jahn B, Trinka E, Unterberger I, Dobesberger J, Walser G, Auckenthaler A, Embacher N, Bauer G, Luef G (2008) Spontaneous abortion and the prophylactic effect of folic acid supplementation in epileptic women undergoing antiepileptic therapy. J Neurol 255(12):1926–1931
Meador KJ, Baker GA, Browning N, Cohen MJ, Clayton-Smith J, Kalayjian LA, Kanner A, Liporace JD, Pennell PB, Privitera M, Loring DW, NEAD Study Group (2011) Foetal antiepileptic drug exposure and verbal versus non-verbal abilities at three years of age. Brain 134(Pt 2): 396–404
Lindhout D, Omtzigt JGC (1994) Teratogenic effects of antiepileptic drugs: Implications for the management of epilepsy in women of childbearing age. Epilepsia 35(Suppl 4):S19-S28
Kaaja E, Kaaja R, Hiilesmaa V (2003) Major malformations in offspring of women with epilepsy. Neurology 60(4):575–579
Cunnington M, Tennis P (2005) LTG and the risk of malformations in pregnancy. Neurology 64:955–960
Ornoy A (2009) Valproic acid in pregnancy: how much are we endangering the embryo and fetus? Reprod Toxicol 28(1):1–10
Vajda FJ, Graham J, Roten A, Lander CM, O’Brien TJ, Eadie M (2012) Teratogenicity of the newer antiepileptic drugs-the Australian experience. J Clin Sci 19(1):57–59
Nguyen HT, Sharma V, McIntyre RS (2009) Teratogenesis associated with antibipolar agents. Adv Ther 26(3):281–294
Hill DS, Wlodarczyk BJ, Palacios AM, Finnell RH (2010) Teratogenic effects of antiepileptic drugs. Expert Rev Neurother 10(6):943–959
Wild C, Lehner P, Reiselhuber S, Schiller-Frühwirth I (2010) Prevention of neural tube defects: regional policies in folic acid enrichment and supplementation. Gesundheitswesen 72(12):875–879
Meijer WM, de Walle HE (2005) Differences in folic-acid policy and the prevalence of neural-tube defects in Europe; recommendations for food fortification in a EUROCAT report. Ned Tijdschr Geneeskd 149(46):2561–2564
Wilson RD, Davies G, Désilets V, Reid GJ, Summers A, Wyatt P, Young D (2003) The use of folic acid for the prevention of neural tube defects and other congenital anomalies. J Obstet Gynaecol Can 25(11):959–965
Padmanabhan R, Abdulrazzaq YM, Bastaki SM, Shafiullah M, Chandranath SI (2003) Experimental studies on reproductive toxicologic effects of LTG in mice. Birth Defects Res B 68:428–438
Padmanabhan R, Shafiullah MM (2003) Amelioration of sodium valproate-induced neural tube defects in mouse fetuses by maternal folic acid supplementation during gestation. Congenit Anom 43(1):29–40
Quattrini A, Ortenzi A, Paggi A et al (1996) LTG and pregnancy [Letter]. Ital J Neurosci 17:441
Rambeck B, Kurlemann G, Stodieck SRG et al (1997) Concentrations of LTG in a mother on LTG treatment and her newborn child. Eur J Clin Pharmacol 51:481–484
Tomson T, Öhman I, Vitols S (1997) LTG in pregnancy and lactation: a case report. Epilepsia 38:1039–1041
Abdulrazzaq YM, Bastaki SMA, Padmanabhan R (1997) Teratogenic effects of vigabatrin in the TO mouse fetuses. Teratology 55:165–176
Abdulrazzaq YM, Padmanabhan R, Bastaki SMA, Ibrahim A, Bener A (2001) Placental transfer of vigabatrin (γ-vinyl GABA) and its effect on concentrations of amino acids in the embryo of TO mice. Teratology 63:127–133
İspir E, Serdar MA, Ozgurtas T, Gulbahar O, Akın KO, Yesildal F, Kurt İ (2015) Comparison of four automated serum vitamin B12 assays. Clin Chem Lab Med 53(8):1205–1213
Padmanabhan R, Abdulrazzaq YM, Bastaki SM, Nurulain M, Shafiullah M (2010) Vigabatrin (VGB) administered during late gestation lowers maternal folate concentration and causes pregnancy loss, fetal growth restriction and skeletal hypoplasia in the mouse. Reprod Toxicol 29(3):366–377
Padmanabhan R, Shafiullah M, Benedict S, Nagelkerke N (2006) Effect of maternal exposure to homocysteine on sodium valproate-induced neural tube defects in the mouse embryos. Eur J Nutr 45(6):311–319
Sterz H, Lehmann H (1985) A critical comparison of the free hand razor blade dissection method according to Wilson with an in situ sectioning method for rat fetuses. Terat Carcin Mutagen 5:347–354
Inouye M (1976) Differential staining of cartilage and bone in fetal mouse skeleton by alcian blue and alizarin red S. Congenit Anom 16:71–173
Marchi NS, Azoubel R, Tognola WA (2001) Teratogenic effects of LTG on rat fetal brain: a morphometric study. Arq Neuropsiquiatr 59:362–364
Ohman I, Vitols S, Tomson T (2000) LTG in pregnancy: pharmacokinetics during delivery, in the neonate, and during lactation. Epilepsia 41(6):709–713
Koren G, Pastuszak A, Ito S (1998) Drugs in pregnancy. N Engl J Med 338:1128–1137
van Gelder MM, van Rooij IA, Miller RK, Zielhuis GA, de Jong-van den Berg LT, Roeleveld N (2010) Teratogenic mechanisms of medical drugs. Hum Reprod Update 16:378–394
Lindhout D (1992) Pharmacogenetics and drug interactions: Role in antiepileptic-drug-induced teratogenesis. Neurology 42:43–47
Petrenaite V, Sabers A, Hansen-Schwartz J (2005) Individual changes in LTG plasma concentrations during pregnancy. Epilepsy Res 65(3):185–188
Reimers A, Helde G, Bråthen G, Brodtkorb E (2011) LTG and its N2-glucuronide during pregnancy: the significance of renal clearance and estradiol. Epilepsy Res 94(3):198–205
Tureski RJ, Bessette EE, Dunbar D, Liberman RG, Skipper PL (2012) Cytochrome P450-mediated metabolism and DNA binding of 2-Amino-1,7-dimethylimidazo[4,5-g]quinoxaline and its carcinogenic isomer2-Amino-3,8-dimethylimidazo[4,5-f]quinoxaline in mice. Chem Res Toxicol 25(2):410–421
Cunnington M, Ferber S, Quartey G; International Lamotrigine Pregnancy Registry Scientific Advisory Committee (2007) Effect of dose on the frequency of major birth defects following fetal exposure to lamotrigine monotherapy in an international observational study. Epilepsia 48(6):1207–1210
Ban L, Fleming KM, Doyle P, Smeeth L, Hubbard RB, Fiaschi L, Tata LJ (2015) Congenital Anomalies in children of mothers taking antiepileptic drugs with and without periconceptional high dose folic acid use: a population-based cohort study. PLoS ONE 10(7): e0131130. https://doi.org/10.1371/journal.pone.0131130
Vajda FJE, Graham JE, Hitchcock AA, O’Brien TJ, Lander CM, Eadie MJ (2010) Is LTG a significant human teratogen? Observations from the Australian Pregnancy Register. Seizure 19:558–561
Weston J, Bromley R, Jackson CF, Adab N, Clayton-Smith J, Greenhalgh J, Hounsome J, McKay AJ, Tudur Smith C, Marson AG (2016) Monotherapy treatment of epilepsy in pregnancy: congenital malformation outcomes in the child. Cochrane Database Syst Rev 11:CD010224
Leppik IE (1990) How to get patients with epilepsy to take their medication. The problem of noncompliance. Postgrad Med 88:253–256
Hendel J, Dam M, Gram L, Winkel P, Jorgensen I (1984) The effect of carbamezapine and valproate on folate metabolism in man. Acta Neurol Scand 69:226–231
Kirke PN, Molloy AM, Daly LE, Burke H, Weir DG, Scott JM (1993) Maternal plasma folate and vitamin B12 are independent risk factors for neural tube defects. Q J Med 86:703–708
Gu Q, Li Y, Cui ZL, Luo XP (2012) Homocysteine, folate, vitamin B12 and B6 in mothers of children with neural tube defects in Xinjiang, China. Acta Paediatr 101(11):e486–e490
Mills JL, McPartlin JM, Kirke PN, Lee YJ, Conley MR, Weir DG, Scott JM (1995) Homocysteine metabolism in pregnancies complicated by neural tube defects. Lancet 345:149–151
Iqbal MM, Gundlapalli SP, Ryan WG, Ryals T, Passman TE (2001) Effect of antimanic mood-stabilizing drugs on fetuses, neonates, and nursing infants. South Med J 94:304
Jordan RL, Wilson JG, Schumacher HJ (1977) Embryotoxicity of the folate antagonist methotrexate in rats and rabbits. Teratology 15:73–80
Papakostas GI, Shelton RC, Zajecka JM et al (2012) L-methylfolate as adjunctive therapy for SSRI-resistant major depression: results of two randomized, double-blind, parallel-sequential trials. Am J Psychiatry 169:1267–1274
Brodie MJ (1992) LTG Lancet 339:1397–1400
Geddes JR, Gardiner A, Rendell J, Voysey M, Tunbridge E, Hinds C, Yu L-M, Hainsworth J, Attenburrow M-J, Somin J, Goodwin GM, Harrison PJ, CEQUEL Investigators and Collaborators (2016) Comparative evaluation of quetiapine plus LTG combination versus quetiapine monotherapy (and folic acid versus placebo) in bipolar depression (CEQUEL): a 2 × 2 factorial randomised trial. Lancet Psychiatry 3:31–39
Dolk H, Wang H, Loane M, Morris J, Garne E, Addor M-C et al (2016) LTG use in pregnancy and risk of orofacial cleft and other congenital anomalies. Neurology 86:1716–1725
Verrotti A, Pascarella R, Trotta D, Giuva T, Morgese G, Chiarelli F (2000) Hyperhomocysteinemia in children treated with sodium valproate and carbamazepine. Epilepsy Res 41:253–257
Alonso-Aperte E, Ubeda N, Achon M, Perez-Miguelsanz J, Varela-Moreiras G (1999) Impaired methionine synthesis and hypomethylation in rats exposed to valproate during gestation. Neurology 52:750–756
Yoo JH, Hong SB (1999) A common mutation in the methylenetetrahydrofolate reductase gene is a determinant of hyperhomocysteinemia in epileptic patients receiving anticonvulsants. Metabolism 48:1047–1051
Dias-Arrastia R (2000) Homocysteine and neurologic disease. Arch Neurol 57:1422–1427
Acknowledgements
We are indebted to Sheikh Hamdan Award for Medical Sciences for providing funds for this work (Grant No. MRG13/2005). We are also grateful to the College of Medicine and Health Sciences, UAE University for making available the laboratory facilities and animals, without which this work would not be possible.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
There are no conflicts of interest with any of the authors.
Rights and permissions
About this article
Cite this article
Abdulrazzaq, Y.M., Shafiullah, M., Kochyil, J. et al. Ameliorative effects of supplemental folinic acid on Lamotrigine-induced fetal malformations in the mouse. Mol Cell Biochem 446, 185–197 (2018). https://doi.org/10.1007/s11010-018-3285-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-018-3285-0