Abstract
Objective
To assess the combination of a non-invasive blood oxygen content (CaO2) monitor and a non-invasive cardiac output (CO) monitor to continuously measure oxygen delivery (DO2; DO2 = CaO2 × CO).
Methods
DO2 was assessed during blood transfusions in an infant with acute hemolytic anemia following admission (~48 h). CaO2 was measured by Pulse Co-Oximetry, which also provides estimates of hemoglobin (Hgb) concentration and percent oxygen saturation. CO was measured by Electrical Velocimetry, which also provides an estimate of stroke volume (SV). Lactate levels, an indirect measure of adequate DO2, were assessed during the initial 8 h following admission.
Results
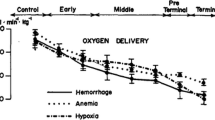
Incremental blood transfusions during the first 36 h increased Hgb from 2.7 to 9.5 g/dL during which time heart rate (HR) normalized from 156 to 115 beats/min. Lactate levels decreased from 20 to 0.8 mmol/L in the first 7 h. Non-invasive Hgb and CaO2 measurements were well correlated with invasive Hgb and CaO2 measures (r 2 = 0.88; P = 0.019; r 2 = 0.86; P = 0.0074, respectively). CO decreased from 2.47 ± 0.06 to 1.28 ± 0.02 L/min and SV decreased from 15.9 ± 0.4 to 11.1 ± 0.2 mL/beat. Mean arterial blood pressure was stable throughout the admission with systemic vascular resistance increasing from 407.6 ± 15.2 to 887.7 ± 30.1 dynes-s/cm5. DO2 was estimated to increase from 120.2 ± 18.9 to 182.4 ± 5.6 mL O2/min.
Conclusions
Non-invasive contin- uous CO and CaO2 monitors are shown in this single case to provide continuous DO2 measurement. The ability to assess DO2 may improve hemodynamic monitoring during goal directed therapies.
Similar content being viewed by others
References
Ralston M, Hazinski MF, Zaritsky AL, Schexnayder SM, Kleinman ME. PALS provider manual. Dallas: American Heart Association; 2006.
Rampal T, Jhanji S, Pearse RM. Using oxygen delivery targets to optimize resuscitation in critically ill patients. Curr Opin Crit Care. 2010;16:244–249.
Lucking SE, Williams TM, Chaten FC, Metz RI, Mickell JJ. Dependence of oxygen consumption on oxygen delivery in children with hyperdynamic septic shock and low oxygen extraction. Crit Care Med. 1990;18:1316–1319.
Huang YC. Monitoring oxygen delivery in the critically ill. Chest. 2005;128:554S–60S.
Yu M, Levy MM, Smith P, Takiguchi SA, Miyasaki A, Myers SA. Effect of maximizing oxygen delivery on morbidity and mortality rates in critically ill patients: a prospective, randomized, controlled study. Crit Care Med. 1993;21:830–838.
Hata JS, Stotts C, Shelsky C, Bayman EO, Frazier A, Wang J, Nickel EJ. Reduced mortality with noninvasive hemodynamic monitoring of shock. J Crit Care. 2011;26:224.e1–224.e8.
Castellanos-Ortega A, Suberviola B, Garcia-Astudillo LA, Holanda MS, Ortiz F, Llorca J, Delgado-Rodriguez M. Impact of the Surviving Sepsis Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a three-year follow-up quasi-experimental study. Crit Care Med. 2010;38:1036–1043.
Collins CL, Andersen CC. Deceptive simplicity: systemic oxygen delivery and pulse oximetry. J Paediatr Child Health. 2007;43:510–512.
Calbet JAL, Joyner MJ. Disparity in regional and systemic circulatory capacities: do they affect the regulation of the circulation? Acta Physiol. 2010;199:393–406.
Miyoshi H, Sumikawa K. Evaluation of circulatory state using pulse oximeter: 2. Measurement of total hemoglobin employing pulse CO-oximetry (Masimo Radical-7). Masui. 2009;58:854–859.
Macknet MR, Allard M, Applegate RL, Rook J. The Accuracy of noninvasive and continuous total hemoglobin measure- ment by pulse CO-oximetry in human subjects undergoing hemodilution. Anesth Analg. 2010;111:1424–1426.
Tomaske M, Knirsch W, Kretschmar O, Woitzek K, Balmer C, Schmitz A, Bauersfeld U, Weiss M, Working Group on Non-Invasive Haemodynamic Monitoring in P. Cardiac output measurement in children: comparison of Aesculon cardiac output monitor and thermodilution. Br J Anaesth. 2008;100:517–520.
Norozi K, Beck C, Osthaus WA, Wille I, Wessel A, Bertram H. Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth. 2008;100:88–94.
Heulitt E, Fajardo E. Normal values and PRISM and TISS scores. In: Toro-Figueroa L, Levin D, Morriss F, editors. Essentials of pediatric intensive care manual. St. Louis: Quality Medical Publishing, Inc.; 1992. p. 447.
Fuhrman BP, Zimmerman J. Pediatric critical care. 3rd ed. Philadelphia: Mosby; 2006.
Al-Azzam SI, Al-Ajlony MJ, Al-Khateeb T, Alzoubi KH, Mhaidat N, Ayoub A. An audit of the precipitating factors for haemolytic crisis among glucose-6-phosphate dehydrogenase-deficient paediatric patients. J Med Screen. 2009;16:167–169.
Osypka MJ, Bernstein DP. Electrophysiologic principles and theory of stroke volume determination by thoracic electrical bioimpedance. AACN Clin Issues. 1999;10:385–399.
Osthaus WA, Huber D, Beck C, Winterhalter M, Boethig D, Wessel A, Sumpelmann R. Comparison of electrical velocimetry and transpulmonary thermodilution for measuring cardiac output in piglets. Paediatr Anaesth. 2007;17:749–755.
Tomaske M, Knirsch W, Kretschmar O, Balmer C, Woitzek K, Schmitz A, Bauersfeld U, Weiss M, Working Group on Noninvasive Haemodynamic Monitoring in P. Evaluation of the Aesculon cardiac output monitor by subxiphoidal Doppler flow measurement in children with congenital heart defects. Eur J Anaesthesiol. 2009;26:412–415.
Schubert S, Schmitz T, Weiss M, Nagdyman N, Huebler M, Alexi-Meskishvili V, Berger F, Stiller B. Continuous, non-invasive techniques to determine cardiac output in children after cardiac surgery: evaluation of transesophageal Doppler and electric velocimetry. J Clin Monit Comput. 2008;22:299–307.
Weisel RD, Berger RL, Hechtman HB. Measurement of cardiac output by thermodilution. N Engl J Med. 1975;292:682–684.
Wippermann CF, Huth RG, Schmidt FX, Thul J, Betancor M, Schranz D. Continuous measurement of cardiac output by the Fick principle in infants and children: comparison with the thermodilution method. Intensive Care Med. 1996;22:467–471.
Custer JW, Rau RE. The harriet lane handbook. 18th ed. Philadelphia: Mosby Elsevier Inc.; 2008.
Cropp GJ. Cardiovascular function in children with severe anemia. Circulation. 1969;39:775–784.
Seear M, Wensley D, MacNab A. Oxygen consumption-oxygen delivery relationship in children. J Pediatr. 1993;123:208–214.
Proulx F, Lemson J, Choker G, Tibby SM. Hemodynamic monitoring by transpulmonary thermodilution and pulse contour analysis in critically ill children. Pediatr Crit Care Med. 2011;12(4):1–8.
Weiss IK, Fink S, Harrison R, Feldman JD, Brill JE. Clinical use of continuous arterial blood gas monitoring in the pediatric intensive care unit. Pediatrics. 1999;103:440–445.
Ganter M, Zollinger A. Continuous intravascular blood gas monitoring: development, current techniques, and clinical use of a commercial device. Br J Anaesth. 2003;91:397–407.
Colgan FJ, Stewart S. An assessment of cardiac output by thermodilution in infants and children following cardiac surgery. Crit Care Med. 1977;5:220–225.
Critchley LA, Lee A, Ho AM-H. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–1192.
Squara P, Cecconi M, Rhodes A, Singer M, Chiche J-D. Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensive Care Med. 2009;35:1801–1808.
Cecconi M, Dawson D, Casaretti R, Grounds RM, Rhodes A. A prospective study of the accuracy and precision of continuous cardiac output monitoring devices as compared to intermittent thermodilution. Minerva Anestesiol. 2010;76:1010–1017.
Lacroix J, Hebert PC, Hutchison JS, Hume HA, Tucci M, Ducruet T, Gauvin F, Collet JP, Toledano BJ, Robillard P, Joffe A, Biarent D, Meert K, Peters MJ, Investigators T, Canadian Critical Care Trials G, Pediatric Acute Lung I, Sepsis Investigators N. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007;356:1609–1619.
Motoyama EK, Davis P. Smith’s anesthesia for infants and children. 7th ed. Philadelphia: C.V. Mosby; 2005.
Cropp GJ. Hemodynamic responses to oxygen breathing in children with severe anemia. Circulation. 1969;40:493–500.
Rachoin J-S, Weisberg LS, McFadden CB. Treatment of lactic acidosis: appropriate confusion. J Hosp Med. 2010;5:E1–E7.
Ouellette DR. The impact of anemia in patients with respiratory failure. Chest. 2005;128:576S–582S.
Brierley J, Carcillo JA, Choong K, Cornell T, DeCaen A, Deymann A, Doctor A, Davis A, Duff J, Dugas M-A, Duncan A, Evans B, Feldman J, Felmet K, Fisher G, Frankel L, Jeffries H, Greenwald B, Gutierrez J, Hall M, Han YY, Hanson J, Hazelzet J, Hernan L, Kiff J, Kissoon N, Kon A, Irazusta J, Lin J, Lorts A, Mariscalco M, Mehta R, Nadel S, Nguyen T, Nicholson C, Peters M, Okhuysen-Cawley R, Poulton T, Relves M, Rodriguez A, Rozenfeld R, Schnitzler E, Shanley T, Skache S, Skippen P, Torres A, von Dessauer B, Weingarten J, Yeh T, Zaritsky A, Stojadinovic B, Zimmerman J, Zuckerberg A. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009;37:666–688.
de Oliveira C, de Oliveira D, Gottschald A, Moura J, Costa G, Ventura A, Fernandes J, Vaz F, Carcillo J, Rivers E, Troster E. ACCM/PALS haemodynamic support guidelines for paediatric septic shock: an outcomes comparison with and without monitoring central venous oxygen saturation. Intensive Care Med. 2008;34:1065–1075.
Levy RJ, Deutschman CS. Cytochrome c oxidase dysfunction in sepsis. Crit Care Med. 2007;35:S468–S475.
Sola A. Oxygen in neonatal anesthesia: friend or foe? Curr Opin Anesthesiol. 2008;21:332–339.
Cabello JB, Burls A, Emparanza JI, Bayliss S, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2010;16(6).
Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Weatherall M, Beasley R. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart. 2009;95:198–202.
Author information
Authors and Affiliations
Corresponding author
Additional information
Steil GM, Eckstein OS, Caplow J, Agus MSD, Walsh BK, Wong J. Non-invasive cardiac output and oxygen delivery measurement in an infant with critical anemia.
Rights and permissions
About this article
Cite this article
Steil, G.M., Eckstein, O.S., Caplow, J. et al. Non-invasive cardiac output and oxygen delivery measurement in an infant with critical anemia. J Clin Monit Comput 25, 113–119 (2011). https://doi.org/10.1007/s10877-011-9287-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-011-9287-z