Abstract
Purpose
To describe and analyze short-term posterior vitreous abnormalities following intravitreal ocriplasmin in eyes with symptomatic vitreomacular traction syndrome (VMT).
Methods
In this institutional, prospective and interventional study enrolled patients with symptomatic focal VMT syndrome treated with intravitreal ocriplasmin. In all cases, spectral-domain optical coherence tomography scans were quantitatively and qualitatively analyzed preoperatively and at 1 and 4 weeks postoperatively.
Results
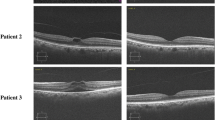
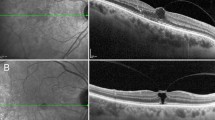
Twenty-three patients, of which 5 were males and 18 females, with a mean age of 69.5 ± 8.2 years were included in this study. Postoperatively, VMT resolved in 11 of 23 eyes (47.8%). In 9 out of 11 cases (81.8%), VMT resolved by postoperative week 1, whether in the remaining 2 (18.2%) anatomical restoration, was diagnosed at postoperative week 4. At postoperative week 1, a foveolar detachment was detected in 9 out of 23 eyes (39.1%). The foveolar detachment resolved all but one eye by the end of postoperative week 4. At the end of the follow-up period, the presence of subretinal fluid was detected in 7 out of 9 eyes (77.8%), and it was significantly associated with a shrinkage of the posterior vitreous cortex (p < 0.006). At the end of the follow-up period, visual acuity was significantly higher in those eyes with VMT resolution (p < 0.001).
Conclusion
Intravitreal ocriplasmin is effective for the treatment of patients with VMT. The postoperative presence of posterior hyaloid shrinkage may be associated with higher traction over the foveal area and the appearance of foveolar detachment.


Similar content being viewed by others
References
Cacciamani A, Gelso A, Simonett JM, Ripandelli G, Pileri M, Stirpe M, Scarinci F (2017) Longitudinal microperimetry evaluation after intravitreal Ocriplasmin injection for vitreomacular traction. Retina 37(10):1832–1838. https://doi.org/10.1097/iae.0000000000001432
Feng HL, Roth DB, Hasan A, Fine HF, Wheatley HM, Prenner JL, Shah SP, Modi KK, Feuer WJ (2018) Intravitreal Ocriplasmin in clinical practice: predictors of success, visual outcomes, and complications. Retina 38(1):128–136. https://doi.org/10.1097/iae.0000000000001505
Haller JA, Stalmans P, Benz MS, Gandorfer A, Pakola SJ, Girach A, Kampik A, Jaffe GJ, Toth CA (2015) Efficacy of intravitreal Ocriplasmin for treatment of vitreomacular adhesion: subgroup analyses from two randomized trials. Ophthalmology 122(1):117–122. https://doi.org/10.1016/j.ophtha.2014.07.045
Chatziralli I, Theodossiadis G, Xanthopoulou P, Miligkos M, Sivaprasad S, Theodossiadis P (2016) Ocriplasmin use for vitreomacular traction and macular hole: a meta-analysis and comprehensive review on predictive factors for vitreous release and potential complications. Graefe’s Arch Clin Exp Ophthal Albrecht von Graefes Arch klinische und Exp Ophthal 254(7):1247–1256. https://doi.org/10.1007/s00417-016-3363-5
Jackson TL, Regillo CD, Girach A, Dugel PU (2016) Baseline predictors of vitreomacular adhesion/traction resolution following an intravitreal injection of Ocriplasmin. Ophthalmic Surg Lasers Imaging Retina 47(8):716–723. https://doi.org/10.3928/23258160-20160808-04
John VJ, Flynn HW Jr, Smiddy WE, Carver A, Leonard R, Tabandeh H, Boyer DS (2014) Clinical course of vitreomacular adhesion managed by initial observation. Retina 34(3):442–446. https://doi.org/10.1097/IAE.0b013e3182a15f8b
Tzu JH, John VJ, Flynn HW Jr, Smiddy WE, Jackson JR, Isernhagen BA, Carver A, Leonard R, Tabandeh H, Boyer DS, Berrocal MH, Suzuki M, Freund KB, Gross JG (2015) Clinical course of vitreomacular traction managed initially by observation. Ophthalmic Surg Lasers Imaging Retina 46(5):571–576. https://doi.org/10.3928/23258160-20150521-09
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P (2013) The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120(12):2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
Kakehashi A, Takezawa M, Akiba J (2014) Classification of posterior vitreous detachment. Clin Ophthalmol 8:1–10. https://doi.org/10.2147/opth.s54021
Govetto A, Bhavsar KV, Virgili G, Gerber MJ, Freund KB, Curcio CA, Burgoyne CF, Hubschman JP, Sarraf D (2017) Tractional abnormalities of the Central Foveal bouquet in epiretinal membranes: clinical spectrum and pathophysiological perspectives. Am J Ophthalmol 184:167–180. https://doi.org/10.1016/j.ajo.2017.10.011
Reichenbach A, Wurm A, Pannicke T, Iandiev I, Wiedemann P, Bringmann A (2007) Muller cells as players in retinal degeneration and edema. Graefe’s Arch Clin Exp Ophthalmol Albrecht von Graefes Arch klinische und Exp Ophthalmol 245(5):627–636. https://doi.org/10.1007/s00417-006-0516-y
Yamada E (1969) Some structural features of the fovea centralis in the human retina. Arch Ophthalmol 82(2):151–159
Gass JD (1999) Muller cell cone, an overlooked part of the anatomy of the fovea centralis: hypotheses concerning its role in the pathogenesis of macular hole and foveomacular retinoschisis. Arch Ophthalmol 117(6):821–823
Govetto A, Lalane RA 3rd, Sarraf D, Figueroa MS, Hubschman JP (2017) Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol 175:99–113. https://doi.org/10.1016/j.ajo.2016.12.006
Stalmans P, Benz MS, Gandorfer A, Kampik A, Girach A, Pakola S, Haller JA (2012) Enzymatic vitreolysis with Ocriplasmin for vitreomacular traction and macular holes. N Engl J Med 367(7):606–615. https://doi.org/10.1056/NEJMoa1110823
Singh RP, Li A, Bedi R, Srivastava S, Sears JE, Ehlers JP, Schachat AP, Kaiser PK (2014) Anatomical and visual outcomes following Ocriplasmin treatment for symptomatic vitreomacular traction syndrome. Br J Ophthalmol 98(3):356–360. https://doi.org/10.1136/bjophthalmol-2013-304219
Chatziralli I, Theodossiadis G, Parikakis E, Datseris I, Theodossiadis P (2016) Real-life experience after intravitreal Ocriplasmin for vitreomacular traction and macular hole: a spectral-domain optical coherence tomography prospective study. Graefe’s Arch Clin Exp Ophthalmol Albrecht von Graefes Arch klinische und Exp Ophthalmol 254(2):223–233. https://doi.org/10.1007/s00417-015-3031-1
Cereda MG, Preziosa C, D’Agostino I, Cozzi M, Bottoni F, Pellegrini M, Giani A, Staurenghi G (2018) Ocriplasmin for vitreomacular traction: looking outside the macula: a wide-field optical coherence tomography study. Retina 38(8):1541–1548. https://doi.org/10.1097/iae.0000000000001785
Neffendorf JE, Kirthi V, Pringle E, Jackson TL (2017) Ocriplasmin for symptomatic vitreomacular adhesion. Cochrane Database Syst Rev 10:Cd011874. https://doi.org/10.1002/14651858.cd011874.pub2
Acknowledgements
The research for this paper was financially supported by Ministry of Health and Fondazione Roma.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cacciamani, A., Gattegna, R., Pileri, M. et al. Short-term changes in posterior vitreous cortex following intravitreal ocriplasmin for symptomatic vitreomacular traction syndrome: a prospective study. Int Ophthalmol 40, 185–193 (2020). https://doi.org/10.1007/s10792-019-01177-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01177-7