Abstract
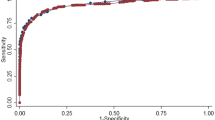
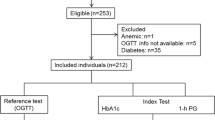
The aim of this analysis is to compare screening strategies with haemoglobin A1c (HbA1c), fasting plasma glucose (FPG) or combined measures in the identification of individuals at high risk for diabetes. Applying American Diabetes Association thresholds for FPG and HbA1c screening, 6,803 subjects free of diabetes were classified as non-diabetic, pre-diabetic and possibly diabetic by FPG (<100, 100–125 and >125 mg/dl) and HbA1c (<5.7, 5.7–6.4 and >6.4%). Hazard ratios, sensitivity and specificity were estimated for individuals with pre-diabetes with respect to incident diabetes in the following 5 years. Areas under the receiver operating characteristic curves (AUC) were estimated for levels of FPG ≤ 125 mg/dl and HbA1c ≤ 6.4% in diabetes prediction. Although FPG and HbA1c screenings poorly agreed in classifying individuals as pre-diabetic, hazard ratios [95% confidence interval] for incident diabetes were similarly increased in univariate models in the two pre-diabetic groups: FPG 100–125 mg/dl, 4.72 [3.69; 6.05]; HbA1c 5.7–6.4%, 3.97 [3.05; 5.23]. HbA1c and FPG had comparable AUCs (FPG, 0.732; HbA1c, 0.725) and consequently similar 5-year sensitivities and specificities for their pre-diabetes definitions (when the lower cut-off for HbA1c-defined pre-diabetes was increased to a level between 5.8 and 5.9%). Combining HbA1c and FPG increased the AUC to 0.778, and a further increase to 0.817 was seen with additional inclusion of conventional risk factors. FPG and HbA1c have comparable (yet insufficient) abilities in identifying individuals at high risk for diabetes. Effectiveness of a diabetes screening program could be improved by a risk score including FPG and HbA1c.


Similar content being viewed by others
Abbreviations
- ADA:
-
American Diabetes Association
- AUC:
-
Area under the receiver operating characteristic curve
- FPG:
-
Fasting plasma glucose
- FOS-SCM:
-
Framingham Offspring Study—Simple Clinical Model
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- I-HbA1c :
-
Isolated HbA1c-defined pre-diabetes
- I-IFG:
-
Isolated impaired fasting glucose
- IQR:
-
Interquartile range
References
Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al. Screening for type 2 diabetes: literature review and economic modelling. Health Technol Assess. 2007;11(17):iii–xi, 1.
American Diabetes Association. Standards of medical care in diabetes-2010. Diabetes Care. 2010;33(1):S11–61.
Mann DM, Carson AP, Shimbo D, Fonseca V, Fox CS, Muntner P. Impact of HbA1c screening criterion on the diagnosis of pre-diabetes among US adults. Diabetes Care. 2010;33:2190–95; published online ahead of print, doi:10.2337/dc10-0752.
American Diabetes Association, European Association for the Study of Diabetes, International Federation of Clinical Chemistry and Laboratory Medicine, and the International Diabetes Federation. Consensus statement on the worldwide standardization of the hemoglobin A1C measurement. Diabetes Care. 2007;30(9):2399–400.
American Diabetes Association. Standards of medical care in diabetes-2011. Diabetes Care. 2011;34(1):S11–61.
Gambino R. Glucose: a simple molecule that is not simple to quantify. Clin Chem. 2007;53(12):2040–1.
Davidson MB, Schriger DL, Peters AL, Lorber B. Relationship between fasting plasma glucose and glycosylated hemoglobin: potential for false-positive diagnoses of type 2 diabetes using new diagnostic criteria. JAMA. 1999;281(13):1203–10.
Lauritzen T, Sandbaek A, Skriver K, Borch-Johnson K. HbA1c and cardiovascular risk score identify people who may benefit from preventive interventions: a 7 year follow-up of a high-risk screening programme for diabetes in primary care (ADDITION), Denmark. Diabetologia. 2011 Feb; published online ahead of print doi:10.1007/s00125-011-2077-9.
Raum E, Lietzau S, Stegmaier C, Brenner H, Rothenbacher D. For the majority of patients with diabetes blood pressure and lipid management is not in line with recommendations. Results from a large population-based cohort in Germany. Pharmacoepidemiol Drug Saf. 2008;17(5):485–94.
Gao L, Weck MN, Stegmaier C, Rothenbacher D, Brenner H. Alcohol consumption, serum gamma-glutamyltransferase, and helicobacter pylori infection in a population-based study among 9733 older adults. Ann Epidemiol. 2010;20(2):122–8.
Richter M, Brand H, Rossler G. [Socio-economic differences in the utilisation of screening programmes and health promotion measures in North Rhine-Westphalia, Germany]. Gesundheitswesen. 2002;64(7):417–23.
John WG, Mosca A, Weykamp C, Goodall I. HbA(1c) standardisation: history, science and politics. Clin Biochem Rev. 2007;28(4):163–8.
Olafsdottir E, Aspelund T, Sigurdsson G, Thorsson B, Benediktsson R, Harris TB, et al. Unfavourable risk factors for type 2 diabetes mellitus are already apparent more than a decade before onset in a population-based study of older persons: from the Age, Gene/Environment Susceptibility-Reykjavik Study (AGES-Reykjavik). Eur J Epidemiol. 2009;24(6):307–14.
Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D’Agostino RB Sr. Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch Intern Med. 2007;167(10):1068–74.
Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613–9.
Kremers WK. Concordance for survival time data: fixed and Time-Dependent Covariates and Possible Ties in Predictor and Time. Technical report series #80. Available from http://mayoresearch.mayo.edu/mayo/research/biostat/techreports.cfm. Survstd SAS Macro available form http://mayoresearch.mayo.edu/mayo/research/biostat/sasmacros.cfm. Accessed 20 Dec 2010.
Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS. Screening for diabetes and prediabetes with proposed A1c-based diagnostic criteria. Diabetes Care. 2010;33(10):2184–9 published online ahead of print.
Lorenzo C, Wagenknecht LE, Hanley AJ, Rewers MJ, Karter AJ, Haffner SM. A1C between 5.7 and 6.4% as a marker for identifying pre-diabetes, insulin sensitivity and secretion, and cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care. 2010;33(9):2104–9.
Sato KK, Hayashi T, Harita N, Yoneda T, Nakamura Y, Endo G, et al. Combined measurement of fasting plasma glucose and A1C is effective for the prediction of type 2 diabetes: the Kansai Healthcare Study. Diabetes Care. 2009;32(4):644–6.
Matsushita K, Blecker S, Pazin-Filho A, Bertoni A, Chang PP, Coresh J, et al. The association of hemoglobin a1c with incident heart failure among people without diabetes: the Atherosclerosis Risk In Communities study. Diabetes. 2010;59(8):2020–6.
Rohlfing CL, Wiedmeyer HM, Little RR, England JD, Tennill A, Goldstein DE. Defining the relationship between plasma glucose and HbA(1c): analysis of glucose profiles and HbA(1c) in the Diabetes Control and Complications Trial. Diabetes Care. 2002;25(2):275–8.
Voulgari C, Tentolouris N. Accuracy and precision of glucose monitoring are relevant to treatment decision-making and clinical outcome in hospitalized patients with diabetes. Diabetes Technol Ther. 2011;13(7):723–30.
Goodall I, Colman PG, Schneider HG, McLean M, Barker G. Desirable performance standards for HbA(1c) analysis - precision, accuracy and standardisation: consensus statement of the Australasian Association of Clinical Biochemists (AACB), the Australian Diabetes Society (ADS), the Royal College of Pathologists of Australasia (RCPA), Endocrine Society of Australia (ESA), and the Australian Diabetes Educators Association (ADEA). Clin Chem Lab Med. 2007;45(8):1083–97.
Ford ES, Cowie CC, Li C, Handelsman Y, Bloomgarden ZT. Iron-deficiency anemia, non-iron-deficiency anemia and HbA1c among adults in the US. J Diabetes. 2011;3(1):67–73.
Thomas MC, Tsalamandris C, MacIsaac RJ, Jerums G. The epidemiology of hemoglobin levels in patients with type 2 diabetes. Am J Kidney Dis. 2006;48(4):537–45.
Nathan DM. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–34.
Soranzo N, Senna S, Wheeler E, Gieger C, Radke D, Dupuis J, et al. Common variants at 10 genomic Loci influence hemoglobin A1c levels via Glycemic and Nonglycemic pathways. Diabetes. 2010;59:3229–39.
Santaguida PL, Balion C, Hunt D, Morrison K, Gerstein H, Raina P, et al. Diagnosis, prognosis, and treatment of impaired glucose tolerance and impaired fasting glucose. Evid Rep Technol Assess (Summ). 2005;128:1–11.
Droumaguet C, Balkau B, Simon D, Caces E, Tichet J, Charles MA, et al. Use of HbA1c in predicting progression to diabetes in French men and women: data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care. 2006;29(7):1619–25.
Nakagami T, Tajima N, Oizumi T, Karasawa S, Wada K, Kameda W, et al. Hemoglobin A1c in predicting progression to diabetes. Diabetes Res Clin Pract. 2010;87(1):126–31.
Wannamethee SG, Papacosta O, Whincup PH, Thomas MC, Carson C, Lawlor DA, et al. The potential for a two-stage diabetes risk algorithm combining non-laboratory-based scores with subsequent routine non-fasting blood tests: results from prospective studies in older men and women. Diabet Med. 2011;28(1):23–30.
Schulze MB, Hoffmann K, Boeing H, Linseisen J, Rohrmann S, Mohlig M, et al. An accurate risk score based on anthropometric, dietary, and lifestyle factors to predict the development of type 2 diabetes. Diabetes Care. 2007;30(3):510–5. Questionnaire available from www.dife.de/de/presse/dife-diabetes-risk-questionnaire-english.pdf. Accessed 17 Dec 2010.
Glumer C, Borch-Johnsen K, Colagiuri S. Can a screening programme for diabetes be applied to another population? Diabet Med. 2005;22(9):1234–8.
Raum E, Rothenbacher D, Low M, Stegmaier C, Ziegler H, Brenner H. Changes of cardiovascular risk factors and their implications in subsequent birth cohorts of older adults in Germany: a life course approach. Eur J Cardiovasc Prev Rehabil. 2007;14(6):809–14.
Löw M, Stegmaier C, Ziegler H, Rothenbacher D, Brenner H. [Epidemiological investigations of the chances of preventing, recognizing early and optimally treating chronic diseases in an elderly population (ESTHER study)]. Dtsch Med Wochenschr. 2004;129(49):2643–7.
Manley SE, Sikaris KA, Lu ZX, Nightingale PG, Stratton IM, Round RA, et al. Validation of an algorithm combining haemoglobin A(1c) and fasting plasma glucose for diagnosis of diabetes mellitus in UK and Australian populations. Diabet Med. 2009;26(2):115–21.
Acknowledgments
The ESTHER study was funded by the Baden-Württemberg state Ministry of Science, Research and Arts (Stuttgart, Germany), the Federal Ministry of Education and Research (Berlin, Germany) and the Federal Ministry of Family Affairs, Senior Citizens, Women and Youth (Berlin, Germany).
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schöttker, B., Raum, E., Rothenbacher, D. et al. Prognostic value of haemoglobin A1c and fasting plasma glucose for incident diabetes and implications for screening. Eur J Epidemiol 26, 779–787 (2011). https://doi.org/10.1007/s10654-011-9619-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9619-9