Abstract
Background and Aims
Retained gastric food (RGF) identified during esophagogastroduodenoscopy (EGD) is often attributed to gastroparesis. This retrospective study evaluated the prevalence of RGF, risk factors for RGF, and the association between RGF and delayed gastric emptying (GE).
Methods
The prevalence and odds ratios for RGF in patients with structural foregut abnormalities or medical risk factors for delayed GE were determined from 85,116 EGDs performed between 2012 and 2018. The associations between RGF, delayed GE, and medical comorbidities were evaluated in 2991 patients without structural abnormalities who had undergone EGD and gastric emptying scintigraphy. The relationship between medication use and RGF was evaluated in 249 patients without structural or medical risk factors for RGF.
Results
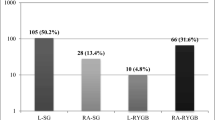
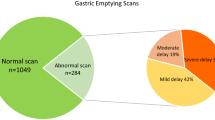
RGF was identified during 3% of EGDs. The odds of RGF were increased in patients with type 1 diabetes (12%, OR 1.7, P ≤ 0.001), type 2 diabetes (6%, OR 1.4, P ≤ 0.001), gastroparesis (14%, OR 4.8, P ≤ 0.001), amyloidosis (5%, OR 1.7, P ≤ 0.001), and structural foregut abnormalities (6%, OR 2.6, P ≤ 0.001). Overall, the PPV of RGF for delayed GE was 55%. However, the PPV varied from 32% in patients without risk factors to 79% in patients with type 1 diabetes. Opioids, cardiovascular medications, and acid suppressants were associated with RGF.
Conclusions
RGF is common during EGD. The PPV of RGF for delayed GE varies depending on underlying risk factors (type 1 diabetes, type 2 diabetes, gastroparesis, and amyloidosis). Acid suppressants or antacids, cardiovascular medications, and opioids are associated with RGF independent of delayed GE.


Similar content being viewed by others
Abbreviations
- EGD:
-
Esophagogastroduodenoscopy
- GE:
-
Gastric emptying
- GES:
-
Gastric emptying scintigraphy
- OR:
-
Odds ratio
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RGF:
-
Retained gastric food
References
Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156:254-272.e11.
Watanabe H, Adachi W, Koide N, et al. Food residue at endoscopy in patients who have previously undergone distal gastrectomy: risk factors and patient preparation. Endoscopy. 2003;35:397–401.
Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999;83:453–460.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–671.
Schwartz DJ, Wynne JW, Gibbs CP, et al. The pulmonary consequences of aspiration of gastric contents at pH values greater than 2.5. Am Rev Respir Dis. 1980;121:119–126.
Coleski R, Baker JR, Hasler WL. Endoscopic gastric food retention in relation to scintigraphic gastric emptying delays and clinical factors. Dig Dis Sci. 2016;61:2593–2601. https://doi.org/10.1007/s10620-016-4173-7.
Jung HK, Choung RS, Locke GR 3rd, et al. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;136:1225–1233.
Brady PG. Gastric phytobezoars consequent to delayed gastric emptying. Gastrointest Endosc. 1978;24:159–161.
Calabuig R, Navarro S, Carrio I, et al. Gastric emptying and bezoars. Am J Surg. 1989;157:287–290.
Hewitt AN, Levine MS, Rubesin SE, et al. Gastric bezoars: reassessment of clinical and radiographic findings in 19 patients. Br J Radiol. 2009;82:901–907.
Tohdo H, Haruma K, Kitadai Y, et al. Gastric emptying and bezoars in Japanese. Report of five cases. Dig Dis Sci. 1993;38:1422–1425. https://doi.org/10.1007/BF01308598.
Camilleri M, Iturrino J, Bharucha AE, et al. Performance characteristics of scintigraphic measurement of gastric emptying of solids in healthy participants. Neurogastroenterol Motil. 2012;24:1076-e562.
Fukami N, Anderson MA, Khan K, et al. The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc. 2011;74:13–21.
Kalf JG, de Swart BJ, Bloem BR, et al. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: a meta-analysis. Parkinsonism Relat Disord. 2012;18:311–315.
Galligan JJ, Sternini C. Insights into the role of opioid receptors in the GI tract: experimental evidence and therapeutic relevance. Handb Exp Pharmacol. 2017;239:363–378.
De Schepper HU, Cremonini F, Park MI, et al. Opioids and the gut: pharmacology and current clinical experience. Neurogastroenterol Motil. 2004;16:383–394.
De Ponti F, Giaroni C, Cosentino M, et al. Calcium-channel blockers and gastrointestinal motility: basic and clinical aspects. Pharmacol Ther. 1993;60:121–148.
Santander R, Mena I, Gramisu M, et al. Effect of nifedipine on gastric emptying and gastrointestinal motility in man. Dig Dis Sci. 1988;33:535–539. https://doi.org/10.1007/BF01798353.
Stanghellini V, Malagelada J-R, Zinsmeister AR, et al. Effect of opiate and adrenergic blockers on the gut motor response to centrally acting stimuli. Gastroenterology. 1984;87:1104–1113.
Bech K, Hovendal CP, Gottrup F, et al. Dopaminergic and beta-adrenergic effects on gastric antral motility. Scand J Gastroenterol Suppl. 1984;89:65–70.
Tougas G, Earnest DL, Chen Y, et al. Omeprazole delays gastric emptying in healthy volunteers: an effect prevented by tegaserod. Aliment Pharmacol Ther. 2005;22:59–65.
Parkman HP, Urbain JL, Knight LC, et al. Effect of gastric acid suppressants on human gastric motility. Gut. 1998;42:243–250.
Glavin GB, Kiernan K, Hnatowich MR, et al. Effects of morphine and naloxone on stress ulcer formation and gastric acid secretion. Eur J Pharmacol. 1986;124:121–127.
Ho MM, Dai S, Ogle CW. Morphine reduces vagal-stimulated gastric acid secretion through a central action. Eur J Pharmacol. 1987;139:251–257.
Meeroff JC, Fernandez GG, Gaon D. Potent reduction of basal acid output produced by meperidine. Am J Dig Dis. 1978;23:696–698.
Caldara R, Cambielli M, Masci E, et al. Effect of loperamide and naloxone on gastric acid secretion in healthy man. Gut. 1981;22:720–723.
Feldman M, Walsh JH, Taylor IL. Effect of naloxone and morphine on gastric acid secretion and on serum gastrin and pancreatic polypeptide concentrations in humans. Gastroenterology. 1980;79:294–298.
Treuren BC, Galletly DC, Robinson BJ, et al. The influence of the H1 and H2 receptor antagonists, terfenadine and ranitidine on the hypotensive and gastric pH effects of the histamine releasing drugs, morphine and tubocurarine. Anaesthesia. 1993;48:758–762.
Fioramonti J, Fargeas MJ, Buéno L. Comparative effects of morphine and cyclazocine on gastrointestinal motility in conscious dogs. Arch Int Pharmacodyn Ther. 1984;270:141–150.
Camilleri M, Sanders KM. Opiates, the pylorus and gastroparesis. Gastroenterology. 2020;159:414–421.
Daly MJ. The classification of adrenoceptors and their effects on gastric acid secretion. Scand J Gastroenterol Suppl. 1984;89:3–9.
Jacob H, Brandt LJ, Farkas P, et al. Beta-adrenergic blockade and the gastrointestinal system. Am J Med. 1983;74:1042–1051.
American Society of Anesthesiologists. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017;126:376–393.
Smith I, Kranke P, Murat I, et al. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011;28:556–569.
Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003. https://doi.org/10.1002/14651858.CD004423.
Camilleri M. Integrated upper gastrointestinal response to food intake. Gastroenterology. 2006;131:640–658.
Prather CM, Camilleri M, Thomforde GM, et al. Gastric axial forces in experimentally delayed and accelerated gastric emptying. Am J Physiol. 1993;264:G928–G934.
Surrenti E, Camilleri M, Kammer PP, et al. Antral axial forces postprandially and after erythromycin in organic and functional dysmotilities. Dig Dis Sci. 1996;41:697–704. https://doi.org/10.1007/BF02213125.
Keshavarzian A, Isaac RM. Erythromycin accelerates gastric emptying of indigestible solids and transpyloric migration of the tip of an enteral feeding tube in fasting and fed states. Am J Gastroenterol. 1993;88:193–197.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bi, D., Choi, C., League, J. et al. Food Residue During Esophagogastroduodenoscopy Is Commonly Encountered and Is Not Pathognomonic of Delayed Gastric Emptying. Dig Dis Sci 66, 3951–3959 (2021). https://doi.org/10.1007/s10620-020-06718-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06718-0