Abstract
Purpose
Diarrhea is recognized as a common adverse event associated with tyrosine kinase inhibitors (TKIs), with those targeting the ErbB family of receptors being associated with the highest rate of diarrhea.
Methods
This paper reviews data on the incidence, timing, and duration of diarrhea associated with US Food and Drug Administration-approved ErbB family-targeted TKIs from the published literature, and sets forth recommendations for management.
Results
In the absence of anti-diarrheal prophylaxis the incidence of any-grade diarrhea varies and typically occurs early during the course of treatment. Although it is difficult to determine if the incidence and severity of diarrhea is related to inhibition of a particular kinase target because of the multi-targeted and overlapping activity of many agents, evidence suggests that second-generation TKIs with broader target profiles (i.e., afatinib, lapatinib, neratinib) result in a higher incidence of diarrhea compared with highly specific first- (erlotinib, gefitinib) or third- (osimertinib) generation agents. The mechanisms responsible for TKI-associated diarrhea are not fully understood and are likely multi-factorial, involving dysregulated ion transport, inflammation, and mucosal injury. Management strategies have been developed—and continue to be refined—to prevent and reduce the severity and duration of TKI-associated diarrhea. For agents associated with more significant symptoms, anti-diarrheal prophylaxis reduces the incidence and severity of diarrhea, and ongoing studies are evaluating specific strategies to further reduce incidence and duration of TKI-associated diarrhea.
Conclusions
Continued investigations into risk factors and pharmacogenomic markers for diarrhea may further improve management of this common toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, 37 different tyrosine kinase inhibitors (TKIs) are approved by the US Food and Drug Administration (FDA) for the treatment of various cancers (Table 1) [1, 2]. These orally administered targeted agents improve patient outcomes in a variety of settings; however, TKIs have a unique adverse event profile including gastrointestinal and cutaneous side effects that must be recognized and managed appropriately [3, 4].
Diarrhea is a common adverse event associated with TKIs. The incidence of all-grade diarrhea in the absence of anti-diarrheal prophylaxis varies from 18 to 95% depending on the agent [5,6,7,8,9,10,11,12]. Diarrhea associated with TKIs can be severe and, if not properly managed, can lead to severe dehydration, dose reductions, and treatment interruptions or discontinuations. It is difficult to determine if the incidence and severity of diarrhea is related to inhibition of a particular kinase target because of the multi-targeted and overlapping activity of many agents [13]. TKIs associated with the highest rate of diarrhea are those targeting the ErbB family of receptors (ErbB1 [HER1, EGFR1], ErbB2 [HER2], ErbB3 [HER3], ErbB4 [HER4]), Bcr-Abl, phosphatidylinositol 3-kinase (PI3K) delta, and vascular endothelial growth factor. In this review, we will focus on the ErbB-family TKIs, some of which target multiple members of the ErbB family, but generally do not have target receptors beyond the ErbB family. Evidence suggests that second-generation agents, including afatinib, lapatinib, and neratinib, which have broader inhibitory profiles, result in a greater incidence of both all-grade and severe diarrhea compared with first-generation agents such as erlotinib and gefitinib that are highly specific to epidermal growth factor receptor (EGFR). For example, the incidence of all-grade diarrhea reported in phase 3 clinical trials of erlotinib, a selective EGFR TKI, was 18–55%, and grade ≥ 3 diarrhea was reported in 3–6% of patients [14, 15]. In contrast, the incidence of all-grade diarrhea associated with afatinib, an ErbB-family TKI that blocks signaling from EGFR, human epidermal growth factor receptor 2 (HER2), and human epidermal growth factor receptor 4 (HER4), was 75–95%, with grade ≥ 3 diarrhea in 10–14% of patients [5, 16, 17].
Signaling by the ErbB family of receptors plays a critical role in normal physiological functioning of cells; these receptors are expressed in a variety of epithelial, mesenchymal, and neuronal tissues and initiate a complex signaling cascade, which regulates proliferation, differentiation, migration, and apoptosis [18]. Overexpression, activating mutations, and autocrine stimulation of ErbB-family receptors—particularly EGFR and HER2—can lead to uncontrolled cell division via activation of multiple downstream signaling pathways [19,20,21], which is particularly common in breast and lung cancers. For example, up to 15% of Caucasian patients and 20–40% of Asian patients with non-small cell lung cancer (NSCLC) have an activating EGFR mutation [22, 23]. HER2-positive breast cancers represent approximately 20% of all breast cancers and tend to be more aggressive than HER2-negative breast cancers [24]. Inhibiting EGFR and HER2 with receptor-targeted TKIs is an important therapeutic approach in these cancers. Currently, there are 6 approved TKIs that primarily target the ErbB family; some agents inhibit multiple members of the ErbB receptor family with varying levels of target specificity and activity (Table 2).
This review focuses on the incidence and management of diarrhea associated with the following 6 FDA-approved TKIs that target the ErbB-family receptors EGFR and HER2 (as of 31 August 2018): gefitinib, erlotinib, lapatinib, afatinib, neratinib, and osimertinib. Future considerations for optimizing the management of TKI-associated diarrhea based on current knowledge about the pathophysiology of diarrhea will also be discussed.
Literature search criteria and methods
Databases searched included Medline (last searched: March 6, 2018); American Society of Clinical Oncology abstracts (2011–2017); European Society for Medical Oncology abstracts (2012–2016); San Antonio Breast Cancer Symposium abstracts (2014–2017); International Association for the Study of Lung Cancer World Conference on Lung Cancer abstracts (2013–2016); clinicaltrials.gov; FDA oncology approvals. Search terms were “diarrhea” AND “target therapy” [substance name].
Definition and differential diagnosis
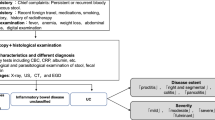
The National Cancer Institute Common Toxicity Criteria for Adverse Events (NCI-CTCAE) provides standard grading for the severity of diarrhea, based primarily on the increase in the number of stools per day compared with baseline (Table 3) [27]. In clinical practice, these criteria, combined with patient assessment, laboratory data, and information obtained from symptom diaries about other physical symptoms such as fever, chills, and nausea, provide insight into the etiology and severity of the diarrhea, all of which are required for optimal patient management.
Based on the NCI-CTCAE grade and the presence or absence of additional symptoms, treatment-related diarrhea may be categorized as uncomplicated or complicated. Uncomplicated diarrhea is defined as grade 1 or 2 diarrhea without complicating signs or symptoms, including moderate to severe cramping, nausea, vomiting, decreased performance status, fever, sepsis, neutropenia, bleeding, and dehydration [28]. Mild to moderate (grade 1 or 2) diarrhea in the presence of at least 1 complicating factor, or diarrhea that is grade ≥ 3 is considered complicated [28].
When a patient experiences diarrhea during treatment, the first step is to rule out alternative causes [28]. The type of diarrhea is also important for proper management and control. Osmotic diarrhea is caused primarily by use of laxatives or inefficient digestion of certain food substances. In this case, stool output is proportional to the intake of the unabsorbable substrate and is usually not severe; normal stool output returns with discontinuation of causative agent or food. In secretory diarrhea, the type of diarrhea that commonly occurs in patients taking TKIs, the ion transport processes of the epithelial cells of the gastrointestinal tract are in a state of active secretion. Common causes of acute-onset secretory diarrhea (in a healthy individual not taking TKIs) are bacterial and viral infections of the gut. This should, of course, be ruled out in patients receiving targeted therapies, although infections are not common in this setting.
Pathophysiology
Understanding the underlying pathologic cause of TKI-associated diarrhea is important for determining appropriate prophylactic and/or treatment regimens, as well as developing new therapeutic strategies to reduce incidence and severity. However, the exact mechanism(s) responsible for TKI-induced diarrhea still need to be fully elucidated, and may be multi-factorial in nature [6, 29].
EGFR and, to a much lesser extent, HER2 are expressed on healthy cells throughout the body including in the gastrointestinal tract [30]. EGFR is expressed at high levels in the basolateral membranes of epithelial cells and is critical for maintaining normal gut function through the regulation of ion transport, including the negative regulation of intestinal epithelial chloride secretion, which regulates the passive movement of water through the gastrointestinal lumen [31, 32]. Pre-clinical studies suggest that epidermal growth factor (EGF) decreases chloride secretion in T84 human colonic intestinal epithelial cells via a signaling cascade that involves protein kinase C and phosphatidylinositol 3-kinase [33]. Dysregulation of intestinal ion transport systems (e.g., through EGFR inhibition) can increase chloride secretion and lead to secretory diarrhea [32], suggesting a possible mechanism for EGFR TKI-associated secretory diarrhea. There is also pre-clinical evidence suggesting a role for HER2 in the inhibitory effect of EGF on epithelial chloride secretion through the formation of EGFR/HER2 heterodimers [34]. Inhibition of EGFR homodimer signaling vs EGFR/HER2 heterodimer signaling may explain the observed differences in the gastrointestinal effects of EGFR- and HER2-targeted agents; however, direct evidence of this effect in the gastrointestinal tract is lacking [35]. Nevertheless, the proposed mechanism involving the dysregulation of ion transport systems does provide researchers with a novel target for further development of management strategies for TKI-associated diarrhea (see discussion later in this article).
A number of other elegant pre-clinical models have been developed to further investigate the mechanism(s) responsible for TKI-associated diarrhea. An animal model of lapatinib-induced diarrhea that closely mimicked clinical symptoms did not support the hypothesis that disruption of chloride secretion contributes to lapatinib-induced diarrhea; lapatinib had no significant effect on serum chloride levels. In addition, there was no evidence of macroscopic or microscopic tissue injury within the jejunum or colon, suggesting that lapatinib alone does not cause epithelial damage. In contrast, combined treatment with paclitaxel and lapatinib in a rat model caused an increase in the incidence of severe diarrhea and weight loss compared with either agent alone, suggestive of intestinal tissue injury [36].
In contrast to the results reported for lapatinib [36], findings from models using other TKIs demonstrated TKI-induced direct mucosal damage apparently leading to diarrhea [37]. Mice that received a 10-day treatment course of gefitinib demonstrated significant atrophy of the small-intestinal wall, which resulted in a decreased absorptive surface area [38]. Similarly, intestinal mucosal damage was greater in mice treated with increasing doses of erlotinib over a 10-day period [39]. Finally, a rat model of neratinib-induced diarrhea suggested that inflammation may also contribute to the pathogenesis of diarrhea. In this model, neratinib increased histological damage in the distal ileum as well as production of pro-inflammatory cytokines, such as interferon-ɣ, in the ileum [40].
Treatment with budesonide, a corticosteroid with low oral bioavailability, decreased the number of days that the rats had diarrhea and reduced histopathological injury induced by neratinib [40]. In addition, budesonide reduced the activity of the inflammatory marker, myeloperoxidase, and increased levels of interleukin-4, an anti-inflammatory cytokine, while decreasing levels of interferon-ɣ. The effects of budesonide and colesevelam, a bile acid sequestrant, are currently being investigated in an ongoing Australian rat model study of neratinib-induced diarrhea.
Multiple other mechanisms—or a combination of mechanisms—have also been proposed as potential causes of TKI-induced diarrhea, including changes in gut motility, damage in the colonic crypts, and altered interstitial microflora [6]. Unfortunately, inter-species differences between model systems (and individuals), in conjunction with variability in the target profile of individual TKIs, make it difficult to pinpoint the precise mechanism(s) responsible for the associated diarrhea.
Clinical experience
Diarrhea, a common side effect of many cancer treatments, including chemotherapeutic agents, targeted therapies, and pelvic radiotherapy, is one of the most common adverse events reported during treatment with a TKI, and can be dose-limiting for TKIs that block EGFR signaling [41]. Effective clinical management of TKI-associated diarrhea requires a clear understanding of incidence, severity, onset, and duration. The incidence of all-grade diarrhea reported for gefitinib, erlotinib, afatinib, and osimertinib in NSCLC and lapatinib and neratinib in breast cancer varies from 18 to 95% depending on the agent (Table 4) [5,6,7,8,9,10,11,12]. Among TKIs targeting the ErbB family of receptors, it appears that the incidence and severity of diarrhea increase with the increasing breadth of targets. Newer, second-generation TKIs were developed with broader target profiles in an attempt to improve the duration of response and overcome resistance to acquired mutations. However, the benefits of these agents come at a cost, with the potential for a higher incidence of adverse events compared with more selective reversible TKIs. Diarrhea was reported in 87–95% of patients receiving afatinib and neratinib, both of which are second-generation irreversible TKIs [16, 29, 42], compared with 18–69% of patients receiving erlotinib and gefitinib [9, 12]. The severity of diarrhea also varies with target profile, with grade ≥ 3 diarrhea reported in up to 25% of patients treated with more focally targeted first-generation TKIs and up to 40% of patients treated with broadly targeted second-generation TKIs.
TKI-associated diarrhea typically occurs early during a course of treatment. For example, in studies without anti-diarrheal prophylaxis, diarrhea associated with afatinib typically occurs in 50–62% of patients within the first 7 days of therapy and in 71% of patients by 14 days after initiating treatment [6]. Similarly, in the phase 3 ExteNET trial (which did not include anti-diarrheal prophylaxis), 40% of patients taking neratinib experienced grade 3 diarrhea after a median of 8 days (interquartile range 4–33), lasting a median of 5 days (interquartile range 2–9) per patient, with a median of two grade ≥ 3 diarrhea events per patient over the course of 1 year of treatment [42].
In clinical trials, TKI-associated diarrhea is a leading cause of dose reductions and treatment discontinuations. In the pivotal trial evaluating afatinib for metastatic NSCLC, diarrhea resulted in dose reductions and treatment discontinuations in 20% and 1.3% of patients in the afatinib arm, respectively [16]. Similarly, in the ExteNET trial, 26% of patients taking neratinib for 1 year without anti-diarrheal prophylaxis required dose reductions due to diarrhea and 17% discontinued treatment. Both dose reductions and discontinuations occurred early (median of 20 days after treatment initiation, interquartile range 9–56 days) [42]. Importantly, diarrhea associated with neratinib resolved quickly when treatment was held and was rarely associated with serious consequences (e.g., renal insufficiency) [43].
The safety profile is different for TKIs that specifically inhibit mutant targets and have a low affinity for wild-type receptors (e.g., osimertinib, a third-generation TKI that potently inhibits T790M EGFR but has a low affinity for wild-type EGFR). These agents are effective in patients whose tumors have acquired resistance to earlier-generation, more broadly specific TKIs and may reduce the adverse effects of inhibiting wild-type receptors and/or off-target effects in normal tissue. The reported incidence of all-grade and grade ≥ 3 diarrhea in patients treated with osimertinib was 41% and 1%, respectively, in the pivotal trial in patients with NSCLC [44]. Osimertinib-associated diarrhea may be due to low-level inhibition of wild-type EGFR [45] and/or non-EGFR related mechanisms that contribute to diarrhea, including direct mucosal damage, resulting in decreased absorption of water [37]. This hypothesis is consistent with the increased incidence of diarrhea observed with escalating doses of osimertinib in the phase 1 clinical trial [46]. Full investigations into third-generation agents are underway; however, toxicity is likely to vary by agent and target.
In summary, although diarrhea is a common side effect of all TKIs, data suggest that second-generation inhibitors are associated with the highest incidence of diarrhea, likely due to broader and off-target effects compared with first-generation agents.
Management strategies
Numerous consensus guidelines and clinical recommendations have been published on the management of cancer treatment-induced diarrhea [47,48,49,50] and, recently, agent-specific TKI-induced diarrhea [6, 29, 51, 52]. Diarrhea management recommendations are also included in the US prescribing information for these agents (Table 5) [5, 7, 9,10,11,12]. Cancer treatment-induced diarrhea management recommendations and those for TKI-associated diarrhea are similar, with management based on severity and associated complications [48]. For example, most cases of uncomplicated grade 1 or 2 diarrhea can be managed effectively with self-administered anti-diarrheal agents such as loperamide, diphenoxylate/atropine, or racecadotril. Loperamide acts as an agonist on opioid receptors in the gastrointestinal tract, decreasing gut motility and inhibiting ion transport, but is minimally absorbed and thus has limited central nervous system effects [49, 53]. Racecadotril is an enkephalinase inhibitor with proven efficacy in models of hypersecretory diarrhea, but it does not enter the brain after oral administration and therefore has no central nervous system effects [54, 55]. In contrast, patients with grade ≥ 3 and/or medically complicated diarrhea require more aggressive management, including treatment interruptions and re-initiation of treatment at a reduced dose, in addition to anti-diarrheal therapies. Medically complicated diarrhea may include moderate to severe cramping, grade ≥ 2 nausea/vomiting, decreased performance status, fever, sepsis, neutropenia, frank bleeding, and dehydration [48], each of which needs to be evaluated and treated. The early identification and proactive management of TKI-associated diarrhea may minimize the occurrence of high-grade events and further complications that lead to treatment discontinuations or hospitalizations.
Anti-diarrheal prophylaxis
Although anti-diarrheal prophylaxis is not recommended for all TKIs before treatment initiation, prophylaxis has demonstrated success at reducing the incidence, severity, and duration of diarrhea for agents with high upfront risk and continues to be investigated. The phase 3 ExteNET trial, evaluating 1 year of neratinib as extended adjuvant therapy in HER2 + breast cancer, did not mandate the use of anti-diarrheal prophylaxis, instead recommending treatment with anti-diarrheal agents and/or dose modifications after symptom onset. Even though most occurrences of diarrhea were self-limiting (resolving quickly after drug hold), grade 3 diarrhea occurred in 40% of patients and 17% of patients discontinued neratinib due to gastrointestinal adverse events. In patients with metastatic breast cancer or NSCLC, loperamide administered during the first month of neratinib treatment (with the first dose and continued through the first cycle of treatment) effectively reduced the rates of grade 3 diarrhea (0–17% across studies) [56,57,58]. As a result, anti-diarrheal prophylaxis with loperamide from the first dose through two cycles of treatment, along with patient education, is the recommended approach for patients receiving neratinib as extended adjuvant therapy [7]. The effectiveness of this approach, as well as other anti-diarrheal agents, continues to be investigated in this setting.
An international, open-label, sequential-cohort, phase 2 study (CONTROL) in HER2 + breast cancer patients receiving extended adjuvant neratinib therapy [59,60,61] is currently investigating the effects of several prophylactic strategies in reducing neratinib-associated diarrhea. The study cohorts include the following: mandatory loperamide prophylaxis (actual n = 137); loperamide + budesonide (actual n = 64); loperamide + the bile acid sequestrant colestipol (actual n = 136); colestipol + prn loperamide (actual n = 104); or a dose-escalation strategy (target n = 64, just starting to enroll) on neratinib-associated diarrhea [60, 61] (Table 6) [59, 62, 63].
Interim data demonstrated that loperamide prophylaxis modestly reduced the incidence of grade ≥ 3 neratinib-associated diarrhea compared with that reported in the phase 3 ExteNET trial without anti-diarrheal prophylaxis (30.7% vs 39.9%, respectively). Adding budesonide or colestipol further reduced the incidence of grade ≥ 3 diarrhea (26.6% and 10.8%, respectively) [60, 61], suggesting that the etiology of neratinib-associated diarrhea may involve inflammation and/or bile acid malabsorption. Compared with the ExteNET trial, prophylaxis with loperamide alone also reduced the median cumulative duration of diarrhea grade ≥ 2 (4 vs 10 days) and grade ≥ 3 (3 vs 5 days) and reduced the median number of diarrhea episodes (any grade) per patient (2 vs 8 episodes). Of note, no grade 4 diarrhea events have occurred. These data suggest that effective anti-diarrheal prophylaxis may help improve the tolerability of neratinib, and ongoing cohorts are exploring colestipol alone or a neratinib dose-escalation strategy.
Investigations are underway to develop pharmacologic management approaches targeting chloride channels, which may be an important mechanism associated with EGFR inhibitors. Crofelemer, an established anti-diarrheal agent for other conditions, inhibits chloride channels in the membrane of epithelial cells [64] and has been investigated in patients with breast cancer receiving targeted therapies in combination with chemotherapy [65, 66]. An ongoing study is investigating anti-diarrheal prophylaxis with crofelemer in HER2-positive patients treated with adjuvant trastuzumab and neratinib followed by neratinib monotherapy (Table 5) [63].
Based on the incidence and severity of lapatinib-associated diarrhea, studies continue to assess the clinical utility of anti-diarrheal prophylaxis. A small retrospective analysis of 44 patients treated with lapatinib suggested that anti-diarrheal prophylaxis may be an effective strategy for patients to achieve therapy goals without interruptions or dose adjustments [67]. An ongoing, randomized, phase 2 study with an estimated enrollment of 140 patients will assess the effect of prophylactic octreotide, a somatostatin analog and established anti-diarrheal agent for cancer treatment-induced diarrhea, to prevent or reduce the frequency and severity of diarrhea in subjects receiving lapatinib in combination with capecitabine for the treatment of HER2 + metastatic breast cancer (Table 5) [62].
Further research is needed to reduce constipation associated with prophylactic regimens and optimize tolerability. For example, in the CONTROL trial, rates of grade 1/2 constipation were 42.3%/14.6% in patients receiving loperamide prophylaxis alone, 62.5%/12.5% with loperamide plus budesonide, and 53.3%/9.2% with loperamide plus colestipol [61]. An ongoing area of investigation in the CONTROL trial is whether anti-diarrheal prophylaxis will have a significant impact on health-related quality of life (HRQoL) [59].
Monitoring
Clear communication between patients and physicians is critical to ensure accurate reporting and characterization of symptoms, exclude other potential causes, and to initiate therapy adjustments as needed. Close patient monitoring is critical for management of diarrhea during the first few weeks of therapy because diarrhea generally occurs within the first week for most TKIs (Table 3) [27]. Patients should be educated that diarrhea is a common side effect of TKIs and about the potential consequences of diarrhea, including dehydration, electrolyte imbalances, and renal insufficiency. Patients should be instructed on the use of anti-diarrheal treatment regimens either as prophylaxis or in case of mild to moderate diarrhea per treatment guidelines, and to monitor the frequency of bowel movements. In addition, patients should be advised to inform their healthcare provider immediately if diarrhea develops (i.e., more than 2–3 episodes per day), for severe or persistent diarrhea, or if diarrhea is associated with weakness, dizziness, or fever. In clinical practice, patient diaries combined with proactive triage management and a thorough evaluation of treatment-emergent diarrhea help to ensure that appropriate management measures are taken.
Intervention
Proactive management of treatment-related diarrhea is recommended to reduce the incidence, duration, and severity. Loperamide is the mainstay for the pharmaceutical management of uncomplicated mild to moderate diarrhea and is recommended in the prescribing information after the onset of diarrhea or as upfront prophylaxis [68]. In some cases, diarrhea persists despite administration of anti-diarrheal agents given prophylactically or at first onset of diarrhea. In this case, TKI treatment should be withheld until diarrhea has resolved to baseline or grade ≤1 and may be reinitiated per labeling. In cases of severe or persistent diarrhea, supportive care including the administration of oral or intravenous electrolytes and fluids, addition of alternative anti-diarrheal agents (e.g., diphenoxylate–atropine, octreotide, or tincture of opium), and diet modification are recommended [48]. Evaluation for infectious diarrhea or other causes should also be considered along with appropriate use of anti-infectives.
In all cases, patient education is critical to help patients identify the signs and symptoms of diarrhea and stress the need for urgent action (i.e., loperamide administration and contacting the patient’s physician for severe or persistent diarrhea).
Future directions
Novel pharmacologic approaches to TKI-associated diarrhea based on its pathophysiology will improve the quality of care and further optimize diarrhea management approaches for patients receiving these targeted therapies [59,60,61]. Research is needed to better understand risk factors for TKI-associated diarrhea, with the goal of identifying those patients at greater risk and to manage diarrhea both proactively and emergently. A proof-of-principle study designed to quantify the risk factors for diarrhea in breast cancer patients treated with lapatinib identified risk factors including advanced age, starting treatment in the spring, a higher incidence of skin metastases, and grade 1 diarrhea in earlier treatment cycles [69]. Pharmacogenomic studies may help to further elucidate the pathophysiology of TKI-induced diarrhea and allow for the identification of vulnerable patients.
Abbreviations
- EGF:
-
Epidermal growth factor
- EGFR:
-
Epidermal growth factor receptor
- FDA:
-
US Food and Drug Administration
- HER:
-
Human epidermal growth factor receptor
- NSCLC:
-
Non-small cell lung cancer
- TKI:
-
Tyrosine kinase inhibitors
References
US Food and Drug Administration. Hematology/Oncology (Cancer) Approvals & Safety Notifications. Updated July 3 (2018) https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm279174.htm. Accessed 9 July 2018
Jeong W, Doroshow JH, Kummar S (2013) United States Food and Drug Administration approved oral kinase inhibitors for the treatment of malignancies. Curr Probl Cancer 37(3):110–144. https://doi.org/10.1016/j.currproblcancer.2013.06.001
Amitay-Laish I, Stemmer SM, Lacouture ME (2011) Adverse cutaneous reactions secondary to tyrosine kinase inhibitors including imatinib mesylate, nilotinib, and dasatinib. Dermatol Ther 24(4):386–395. https://doi.org/10.1111/j.1529-8019.2011.01431.x
Bowen JM (2013) Mechanisms of TKI-induced diarrhea in cancer patients. Curr Opin Support Palliat Care 7(2):162–167. https://doi.org/10.1097/SPC.0b013e32835ec861
Gilotrif [package insert] (2016) Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT
Yang JC, Reguart N, Barinoff J, Kohler J, Uttenreuther-Fischer M, Stammberger U, O’Brien D, Wolf J, Cohen EE (2013) Diarrhea associated with afatinib: an oral ErbB family blocker. Expert Rev Anticancer Ther 13(6):729–736. https://doi.org/10.1586/era.13.31
Nerlynx [package insert] (2017) Puma Biotechnology, Inc., Los Angeles, CA
Mortimer J, Di Palma J, Jahanzeb M, Schmid K, Ye Y (2016) Characterization of neratinib-induced diarrhea in patients with early-stage HER2 + breast cancer: analyses from the phase III ExteNET trial [poster]. Presented at: 39th Annual San Antonio Breast Cancer Symposium; December 6–10, 2016; San Antonio, TX. Abstract P4-21-10
Tykerb [package insert] (2017) Novartis Pharmaceuticals Corporation, East Hanover, NJ
Tarceva [package insert] (2016) Genentech USA, Inc., South San Francisco
Tagrisso [package insert] (2017) AstraZeneca Pharmaceuticals LP, Wilmington, DE
Iressa [package insert] (2015) AstraZeneca Pharmaceuticals LP, Wilmington, DE
Kitagawa D, Yokota K, Gouda M, Narumi Y, Ohmoto H, Nishiwaki E, Akita K, Kirii Y (2013) Activity-based kinase profiling of approved tyrosine kinase inhibitors. Genes Cells 18(2):110–122. https://doi.org/10.1111/gtc.12022
Ciuleanu T, Stelmakh L, Cicenas S, Miliauskas S, Grigorescu AC, Hillenbach C, Johannsdottir HK, Klughammer B, Gonzalez EE (2012) Efficacy and safety of erlotinib versus chemotherapy in second-line treatment of patients with advanced, non-small-cell lung cancer with poor prognosis (TITAN): a randomised multicentre, open-label, phase 3 study. Lancet Oncol 13(3):300–308. https://doi.org/10.1016/S1470-2045(11)70385-0
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S, Smylie M, Martins R, van Kooten M, Dediu M, Findlay B, Tu D, Johnston D, Bezjak A, Clark G, Santabarbara P, Seymour L, National Cancer Institute of Canada Clinical Trials G (2005) Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 353(2):123–132. https://doi.org/10.1056/NEJMoa050753
Sequist LV, Yang JC, Yamamoto N, O’Byrne K, Hirsh V, Mok T, Geater SL, Orlov S, Tsai CM, Boyer M, Su WC, Bennouna J, Kato T, Gorbunova V, Lee KH, Shah R, Massey D, Zazulina V, Shahidi M, Schuler M (2013) Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 31(27):3327–3334. https://doi.org/10.1200/JCO.2012.44.2806
Soria JC, Felip E, Cobo M, Lu S, Syrigos K, Lee KH, Goker E, Georgoulias V, Li W, Isla D, Guclu SZ, Morabito A, Min YJ, Ardizzoni A, Gadgeel SM, Wang B, Chand VK, Goss GD, Investigators LU-L (2015) Afatinib versus erlotinib as second-line treatment of patients with advanced squamous cell carcinoma of the lung (LUX-Lung 8): an open-label randomised controlled phase 3 trial. Lancet Oncol 16(8):897–907. https://doi.org/10.1016/S1470-2045(15)00006-6
Olayioye MA, Neve RM, Lane HA, Hynes NE (2000) The ErbB signaling network: receptor heterodimerization in development and cancer. EMBO J 19(13):3159–3167. https://doi.org/10.1093/emboj/19.13.3159
Scagliotti GV, Selvaggi G, Novello S, Hirsch FR (2004) The biology of epidermal growth factor receptor in lung cancer. Clin Cancer Res 10(12 Pt 2):4227s–4232s. https://doi.org/10.1158/1078-0432.CCR-040007
Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, Levin WJ, Stuart SG, Udove J, Ullrich A et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244(4905):707–712
Farin K, Di Segni A, Mor A, Pinkas-Kramarski R (2009) Structure-function analysis of nucleolin and ErbB receptors interactions. PLoS ONE 4(7):e6128. https://doi.org/10.1371/journal.pone.0006128
Carpenter RL, Lo HW (2012) Dacomitinib, an emerging HER-targeted therapy for non-small cell lung cancer. J Thorac Dis 4(6):639–642. https://doi.org/10.3978/j.issn.2072-1439.2012.10.09
Jang TW, Oak CH, Chang HK, Suo SJ, Jung MH (2009) EGFR and KRAS mutations in patients with adenocarcinoma of the lung. Korean J Intern Med 24(1):48–54. https://doi.org/10.3904/kjim.2009.24.1.43
Gullick WJ, Srinivasan R (1998) The type 1 growth factor receptor family: new ligands and receptors and their role in breast cancer. Breast Cancer Res Treat 52(1–3):43–53
Peters S, Zimmermann S, Adjei AA (2014) Oral epidermal growth factor receptor tyrosine kinase inhibitors for the treatment of non-small cell lung cancer: comparative pharmacokinetics and drug-drug interactions. Cancer Treat Rev 40(8):917–926. https://doi.org/10.1016/j.ctrv.2014.06.010
Feldinger K, Kong A (2015) Profile of neratinib and its potential in the treatment of breast cancer. Breast Cancer (Dove Med Press) 7:147–162. https://doi.org/10.2147/BCTT.S54414
US Department of Health and Human Services, National Institutes of Health, National Cancer Institute (June 14, 2010) Common Terminology Criteria for Adverse Events (CTCAE); Version 4.0. v4.03. ClinicalTrials.gov. https://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed 20 Oct 2017
Cherny NI (2008) Evaluation and management of treatment-related diarrhea in patients with advanced cancer: a review. J Pain Symptom Manag 36(4):413–423. https://doi.org/10.1016/j.jpainsymman.2007.10.007
Hirsh V, Blais N, Burkes R, Verma S, Croitoru K (2014) Management of diarrhea induced by epidermal growth factor receptor tyrosine kinase inhibitors. Curr Oncol 21(6):329–336. https://doi.org/10.3747/co.21.2241
Gullick WJ, Berger MS, Bennett PL, Rothbard JB, Waterfield MD (1987) Expression of the c-erbB-2 protein in normal and transformed cells. Int J Cancer 40(2):246–254
Uribe JM, Barrett KE (1997) Nonmitogenic actions of growth factors: an integrated view of their role in intestinal physiology and pathophysiology. Gastroenterology 112(1):255–268
McCole DF, Barrett KE (2009) Decoding epithelial signals: critical role for the epidermal growth factor receptor in controlling intestinal transport function. Acta Physiol (Oxf) 195(1):149–159. https://doi.org/10.1111/j.1748-1716.2008.01929.x
Uribe JM, Keely SJ, Traynor-Kaplan AE, Barrett KE (1996) Phosphatidylinositol 3-kinase mediates the inhibitory effect of epidermal growth factor on calcium-dependent chloride secretion. J Biol Chem 271(43):26588–26595
Keely SJ, Barrett KE (1999) ErbB2 and ErbB3 receptors mediate inhibition of calcium-dependent chloride secretion in colonic epithelial cells. J Biol Chem 274(47):33449–33454
Laux I, Jain A, Singh S, Agus DB (2006) Epidermal growth factor receptor dimerization status determines skin toxicity to HER-kinase targeted therapies. Br J Cancer 94(1):85–92. https://doi.org/10.1038/sj.bjc.6602875
Bowen JM, Mayo BJ, Plews E, Bateman E, Stringer AM, Boyle FM, Finnie JW, Keefe DM (2012) Development of a rat model of oral small molecule receptor tyrosine kinase inhibitor-induced diarrhea. Cancer Biol Ther 13(13):1269–1275. https://doi.org/10.4161/cbt.21783
Loriot Y, Perlemuter G, Malka D, Penault-Llorca F, Boige V, Deutsch E, Massard C, Armand JP, Soria JC (2008) Drug insight: gastrointestinal and hepatic adverse effects of molecular-targeted agents in cancer therapy. Nat Clin Pract Oncol 5(5):268–278. https://doi.org/10.1038/ncponc1087
Hare KJ, Hartmann B, Kissow H, Holst JJ, Poulsen SS (2007) The intestinotrophic peptide, glp-2, counteracts intestinal atrophy in mice induced by the epidermal growth factor receptor inhibitor, gefitinib. Clin Cancer Res 13(17):5170–5175. https://doi.org/10.1158/1078-0432.CCR-07-0574
Rasmussen AR, Viby NE, Hare KJ, Hartmann B, Thim L, Holst JJ, Poulsen SS (2010) The intestinotrophic peptide, GLP-2, counteracts the gastrointestinal atrophy in mice induced by the epidermal growth factor receptor inhibitor, erlotinib, and cisplatin. Dig Dis Sci 55(10):2785–2796. https://doi.org/10.1007/s10620-009-1104-x
Secombe KR, Ball IA, Shirren J, Wignall AD, Wardill HR, Van Sebille YZA, Bowen JM (2017) Budesonide reduces neratinib-induced gastrointestinal injury and diarrhoea in rats [abstract]. Presented at: Clinical Oncology Society of Australia (COSA) 2017 Annual Scientific Meeting; November 13–17, 2017; Sydney, Australia. Abstract 1069
Keefe DM, Gibson RJ (2007) Mucosal injury from targeted anti-cancer therapy. Support Care Cancer 15(5):483–490. https://doi.org/10.1007/s00520-006-0181-z
Chan A, Delaloge S, Holmes FA, Moy B, Iwata H, Harvey VJ, Robert NJ, Silovski T, Gokmen E, von Minckwitz G, Ejlertsen B, Chia SK, Mansi J, Barrios CH, Gnant M, Buyse M, Gore I, Smith J II, Harker G, Masuda N, Petrakova K, Zotano AG, Iannotti N, Rodriguez G, Tassone P, Wong A, Bryce R, Ye Y, Yao B, Martin M, ExteNET Study Group (2016) Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 17(3):367–377. https://doi.org/10.1016/S1470-2045(15)00551-3
Martin M, Holmes FA, Ejlertsen B, Delaloge S, Moy B, Iwata H, von Minckwitz G, Chia SKL, Mansi J, Barrios CH, Gnant M, Tomasevic Z, Denduluri N, Separovic R, Gokmen E, Bashford A, Ruiz Borrego M, Kim SB, Jakobsen EH, Ciceniene A, Inoue K, Overkamp F, Heijns JB, Armstrong AC, Link JS, Joy AA, Bryce R, Wong A, Moran S, Yao B, Xu F, Auerbach A, Buyse M, Chan A, ExteNET Study Group (2017) Neratinib after trastuzumab-based adjuvant therapy in HER2-positive breast cancer (ExteNET): 5-year analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 18(12):1688–1700. https://doi.org/10.1016/S1470-2045(17)30717-9
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, Shepherd FA, He Y, Akamatsu H, Theelen WS, Lee CK, Sebastian M, Templeton A, Mann H, Marotti M, Ghiorghiu S, Papadimitrakopoulou VA, Aura Investigators (2017) Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med 376(7):629–640. https://doi.org/10.1056/NEJMoa1612674
Santarpia M, Liguori A, Karachaliou N, Gonzalez-Cao M, Daffina MG, D’Aveni A, Marabello G, Altavilla G, Rosell R (2017) Osimertinib in the treatment of non-small-cell lung cancer: design, development and place in therapy. Lung Cancer 8:109–125. https://doi.org/10.2147/LCTT.S119644
Gao X, Le X, Costa DB (2016) The safety and efficacy of osimertinib for the treatment of EGFR T790M mutation positive non-small-cell lung cancer. Expert Rev Anticancer Ther 16(4):383–390. https://doi.org/10.1586/14737140.2016.1162103
Andreyev J, Ross P, Donnellan C, Lennan E, Leonard P, Waters C, Wedlake L, Bridgewater J, Glynne-Jones R, Allum W, Chau I, Wilson R, Ferry D (2014) Guidance on the management of diarrhoea during cancer chemotherapy. Lancet Oncol 15(10):e447–e460. https://doi.org/10.1016/S1470-2045(14)70006-3
Benson AB III, Ajani JA, Catalano RB, Engelking C, Kornblau SM, Martenson JA Jr, McCallum R, Mitchell EP, O’Dorisio TM, Vokes EE, Wadler S (2004) Recommended guidelines for the treatment of cancer treatment-induced diarrhea. J Clin Oncol 22(14):2918–2926. https://doi.org/10.1200/JCO.2004.04.132
Kornblau S, Benson AB, Catalano R, Champlin RE, Engelking C, Field M, Ippoliti C, Lazarus HM, Mitchell E, Rubin J, Stiff PJ, Vokes E, Wadler S (2000) Management of cancer treatment-related diarrhea. Issues and therapeutic strategies. J Pain Symptom Manage 19(2):118–129
National Comprehensive Cancer Network (June 1, 2017) NCNN Clinical Practice Guidelines in Oncology; Palliative Care Version 2.2017. https://www.nccn.org/professionals/physician_gls/pdf/palliative.pdf. Accessed 27 Oct 2017
Frankel C, Palmieri FM (2010) Lapatinib side-effect management. Clin J Oncol Nurs 14(2):223–233. https://doi.org/10.1188/10.CJON.223-233
Ustaris F, Saura C, Di Palma J, Bryce R, Moran S, Neuman L, Ruiz R (2015) Effective management and prevention of neratinib-induced diarrhea. Am J Hematol/Oncol 11(11):13–22
Hughes S, Higgs NB, Turnberg LA (1982) Antidiarrhoeal activity of loperamide: studies of its influence on ion transport across rabbit ileal mucosa in vitro. Gut 23(11):974–979
Matheson AJ, Noble S (2000) Racecadotril. Drugs 59(4):829–835; discussion 836–827
Schwartz JC (2000) Racecadotril: a new approach to the treatment of diarrhoea. Int J Antimicrob Agents 14(1):75–79
Besse B, Soria JC, Yao B, Kris M, Chao B, Cortot A, Mazieres J, Socinski MA, Horn L, Waqar S, Barlesi F, Gray JE, Moro-Sibilot D, Oton A, Quoix E, Lalani A, McCulloch L, Bryce R, Gandhi L (2014) Neratinib (N) with or without temsirolimus (TEM) in patients (pts) with non-small cell lung cancer (NSCLC) carrying HER2 somatic mutations: an international randomized phase II study [abstract]. Ann Oncol 25(suppl 4):39-PR. https://doi.org/10.1093/annonc/mdu438.47 Abstract LAB.
Gajria D, Modi S, Saura C, Sakr R, Solano K, Won H, Pannu H, Patil S, Lake D, Traina T, King T, Berger M, Baselga J, Rosen N, Hudis C, Chandarlapaty S (2015) A phase I/II study of neratinib plus temsirolimus in HER2 + metastatic breast cancer reveals ongoing HER2 pathway dependence in many patients despite several lines of HER2 targeted therapy [abstract]. Cancer Res 75(9 suppl): Abstract P5-19-04. https://doi.org/10.1158/1538-7445.SABCS14-P5-19-04
Jankowitz RC, Abraham J, Tan AR, Limentani SA, Tierno MB, Adamson LM, Buyse M, Wolmark N, Jacobs SA (2013) Safety and efficacy of neratinib in combination with weekly paclitaxel and trastuzumab in women with metastatic HER2positive breast cancer: an NSABP Foundation Research Program phase I study. Cancer Chemother Pharmacol 72(6):1205–1212. https://doi.org/10.1007/s00280-013-2262-2
US National Library of Medicine NCT02400476 (2017) A study looking at the incidence and severity of diarrhea in patients with early-stage HER2 + breast cancer treated with neratinib and loperamide. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02400476?term=NCT02400476&rank=1. Accessed August 10, Cited October 24, 2017
Ibrahim E, Tripathy D, Wilkinson M, Hurvitz S, Iannotti N, Kellum A, Manalo Y, Wong S, Hansen V, Alvarez R, Chan A, Gore I, Kendall D, Wade J, Olek E, Hunt D, Fang P, Ebtahaj A, Barcenas CH (2017) Effects of adding budesonide or colestipol to loperamide prophylaxis on neratinib-associated diarrhea in patients (pts) with HER2 + early-stage breast cancer (eBC): the CONTROL trial. Cancer Res 77(13 suppl): Abstract CT128. https://doi.org/10.1158/1538-7445.AM2017-CT128
Hurvitz S, Chan A, Iannotti N, Ibrahim E, Chien J, Chan N, Kellum A, Hansen V, Marx G, Kendall S, Wilkinson M, Castrello A, Ruiz R, Fang P, Hunt D, Moran S, Olek E, Barcenas CH, Rugo HS (2017) Effects of adding budesonide or colestipol to loperamide prophylaxis on neratinib-associated diarrhea in patients with HER2 + early-stage breast cancer: the CONTROL trial[poster]. Presented at: 40th Annual San Antonio Breast Cancer Symposium; December 5–9, 2017; San Antonio, TX. Abstract P3-14-01
US National Library of Medicine NCT02294786. Study of prophylactic octreotide to prevent or reduce the frequency and severity of diarrhoea in subjects receiving lapatinib with capecitabine for the treatment of metastatic breast cancer. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02294786?term=NCT02294786&rank=1. Accessed November 8, 2017 Updated September 28, 2017
US National Library of Medicine NCT03094052 (2017) Diarrhea prophylaxis in patients with HER2 + breast cancer treated with trastuzumab and neratinib, followed by neratinib monotherapy. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03094052?term=NCT03094052&rank=1. Accessed November 8, Updated September 1, 2017
Cottreau J, Tucker A, Crutchley R, Garey KW (2012) Crofelemer for the treatment of secretory diarrhea. Expert Rev Gastroenterol Hepatol 6(1):17–23. https://doi.org/10.1586/egh.11.87
Gao JJ, Tan M, Pohlmann PR, Swain SM (2017) HALT-D: a phase II evaluation of Crofelemer for the prevention and prophylaxis of diarrhea in patients with breast cancer on pertuzumab-based regimens. Clin Breast Cancer 17(1):76–78. https://doi.org/10.1016/j.clbc.2016.08.005
US National Library of Medicine NCT02910219 (2017) Diarrhea prevention and prophylaxis with crofelemer in HER2 positive breast cancer patients (HALT-D). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02910219. Accessed April 20, Cited October 27, 2017
Jamil MO, Rizwan M, Carpenter JT (2015) Prophylactic use of antidiarrheal agents to control diarrhea associated with lapatinib therapy in breast cancer patients [abstract]. J Clin Oncol 33(29 suppl): Abstract 205. https://doi.org/10.1200/jco.2015.33.29_suppl.205
Imodium [package insert] (2016) Johnson & Johnson Consumer Inc., NJ, New Brunswick
Dranitsaris G, Lacouture ME (2014) Development of prediction tools for diarrhea and rash in breast cancer patients receiving lapatinib in combination with capecitabine. Breast Cancer Res Treat 147(3):631–638. https://doi.org/10.1007/s10549-014-3126-0
Acknowledgements
We are grateful to Amanda C. Vreeland, PhD (Accuverus) and to Lee Miller (Miller Medical Communications Ltd) for editorial assistance in the preparation of this manuscript. We would also like to thank Puma Biotechnology Inc for the support in funding this assistance.
Disclaimer
Puma Biotechnology, Inc., provided financial support for medical editorial assistance. Richard Bryce and Elizabeth Olek are employees of Puma Biotechnology, Inc. Susan Moran was previously employed by and is a shareholder of Puma Biotechnology, Inc.
Funding
Funding for this study and article processing charges was provided by Puma Biotechnology, Inc.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors take complete responsibility for the integrity and accuracy of the data as a whole and have given final approval for the version to be published. Hope S. Rugo: Research funding to UCSF from Genentech/Roche, MacroGenics, and Pfizer; Travel support as an unpaid consultant to Puma Biotechnology, Inc. Jack A. Di Palma: Member, Independent Data Monitoring Committee, Puma Biotechnology. Debu Tripathy: Serves on Scientific Advisory Board for Puma Biotechnology, Inc. (unpaid.) Richard Bryce and Elizabeth Olek are employees of Puma Biotechnology, Inc. Susan Moran was previously employed by and is a shareholder of Puma Biotechnology, Inc. Linda Bosserman: Serves as an advisor and on the speaker bureau for Puma Biotechnology (paid).
Ethical approval
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Additional information
Susan Moran was an employee of Puma Biotechnology, Inc., during the development and writing of the manuscript. She is now an employee of QED Therapeutics.
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Rugo, H.S., Di Palma, J.A., Tripathy, D. et al. The characterization, management, and future considerations for ErbB-family TKI-associated diarrhea. Breast Cancer Res Treat 175, 5–15 (2019). https://doi.org/10.1007/s10549-018-05102-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-05102-x