Abstract
Aim
The maintenance of physical activity (PA) over the life course is considered a hallmark for ageing well, but individuals who practice PA also often pursue lifestyles (e.g., smoking) that may inhibit the medicinal impact of PA on them. PA is said to protect against cardiovascular diseases (CVDs), but the literature has little to say about the impact of PA on the risk of CVDs when it is associated with lifestyle factors, comorbidities, and personal characteristics. This study aimed to assess the association between PA time and CVDs, with relevant lifestyle factors, comorbidities, and personal characteristics treated as covariates.
Subject and methods
The study’s population was retired and working older people aged 60 years or more in Accra, Ghana. A total of 686 individuals responded to self-reported questionnaires. Pearson’s chi-square test and binary logistic regression were used to present findings.
Results
The study found that the risk of having one or more CVDs increases as time spent in moderate and vigorous PA increases, whereas individuals who drank alcohol a few days a week or most days a week are respectively 2 (OR = 2.415; p = 0.037) and 22 (OR = 21.933; p = 0.000) times more likely to have one or more CVDs compared to those who never drank alcohol.
Conclusion
Health education should not only encourage PA maintenance but should also make individuals aware of the need to avoid unhealthy behaviours to maximize the positive effect of PA on health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases (CVDs) are the leading cause of mortality in older populations globally (Buecker et al. 2020; Fini et al. 2017; Higueras-Fresnillo et al. 2017; Zhang et al. 2021a, b) and have become a major health risk even in younger populations (Buecker et al. 2020; Granger et al. 2017). Consequently, CVDs account for much of the world’s disease burden and health care expenditure. The passion of public health stakeholders and researchers in championing population-level interventions for preventing CVDs and/or at least avoiding their progression is thus well-founded. Central to these interventions is the encouragement of individuals to meet recommended physical activity (PA) levels such as 150–300 minutes of moderate intensity PA per week (Bull et al. 2020). PA is a form of prophylactic behaviour, and research to date shows that meeting recommended PA levels protects the individual against not only cardiovascular disease (e.g., stroke, hypertension, type 2 diabetes, arteriosclerosis, etc.) but also depression, neurodegenerative diseases (i.e., dementia, Parkinson’s disease), and other morbidities (Asiamah and Mensah 2017; Bennett et al. 2017; Buecker et al. 2020; Buffart et al. 2012; Holtermann et al. 2021; Garnvik et al. 2020; Sun et al. 2013; Zhang et al. 2021a, b).
Sedentary behaviour (SB) is a health risk that facilitates the development or progression of CVDs like those mentioned above (Buecker et al. 2020; Rosenberg et al. 2016; Zhang et al. 2021a, b). If so, regular uptake of PA or meeting recommended PA levels is not enough to reduce the risk of CVDs; individuals must reduce their sedentary time to the lowest possible level to reap the maximum benefit of PA towards healthy ageing. To avoid SB and its health risks, the individual must achieve an energy expenditure of not less than 1.5 metabolic equivalent in PA and must avoid sedentary behaviours (e.g., sitting) lasting 30 or more minutes at any given period (Bull et al. 2020). As mentioned above, the most vulnerable group to CVDs in any population is older people, a reason why regular uptake of PA and the avoidance of SB in older populations are crucial and constitute a healthy habit. Even so, more than just meeting recommended PA levels and avoiding sedentary behaviour is expected of individuals to grow well and maintain health into later life.
Poor diet (e.g., high meat consumption diet, junk food, etc.) and eating habits, intake of excess alcohol, and smoking are lifestyle factors that have been frequently identified in the literature as health risk factors (Buscail et al. 2017; Zhang et al. 2021a, b). These behaviours have also been reported as major facilitators of CVDs in the general population (Buscail et al. 2017; Holtermann et al. 2021; Ramakrishnan et al. 2021), and they can exacerbate morbidity at old age, as they often serve as lurking life course health risks. Therefore, living healthy is about adopting healthy eating habits and avoiding smoking as well as excess intake of alcohol. Similarly, depending on diets rich in leafy vegetables and fruits and staying free of alcohol and tobacco is a hallmark for healthy living (Zhang et al. 2021a, b; Buscail et al. 2017). As a result, healthy ageing does not only require an uptake of regular physical activity and the avoidance of sedentary behaviour but also embraces eating healthy and living a life devoid of smoking and excessive intake of alcohol. To reduce the risk of CVDs in late-life, therefore, people must complement PA with all relevant health-seeking behaviours and avoid choices that increase disease risk. Given the above concerns, it is expected that health promotion efforts are cognizant of all lifestyle factors that are inherent in older populations in developing countries. This is to say that health promoters might find it necessary to educate older people not to only avoid SB and meet recommended PA levels but also to eschew key unhealthy behaviours that can nullify the impact of PA on the risk of CVDs (Temporelli 2021; Asiamah et al. 2019).
The above assertions are consistent with available pieces of empirical evidence, but empirical studies supporting them have not adjusted for all relevant covariates (including lifestyle factors that can either support or counter PA’s influence on the risk of CVDs), particularly in an African context. For instance, volunteering and diet have been found to have a significant association with PA and its effect on health outcomes and the risk of cardiovascular disease (Buscail et al. 2017; Detollenaere et al. 2017). This evidence suggests that volunteering, diet, and any other correlate of PA can confound the association between PA and CVDs. Based on the above concerns, we attempted to examine the association between CVDs, PA, and other lifestyle factors. In testing this association, we controlled for potential confounding variables. Though previous studies (Asiamah et al. 2019; Temporelli 2021; Carré 2019) adjusted for different sets of confounding variables (e.g., gender, education, income, marital status) in the past, lifestyle factors (e.g., diet, sedentary behaviour) were not considered, particularly in an African sample. Thus, this study considers a unique set of potential confounding variables over an African sample. Apart from its contribution to public health policy development and implementation, this study is expected to guide future research work and provide implications for health promotion and education.
Methods
Study design
This study adopted a cross-sectional design. Binary logistic regression was employed to assess the primary relationships of interest while adjusting for potential confounding variables.
Sample and recruitment
The study setting was the head office of the Social Security and National Insurance Trust (SSNIT) in Accra, where access to eligible older participants was guaranteed. Participants were volunteer older people aged between 60 and 89 years who visited the said office during the study period. The criteria for selecting participants were: (a) being aged 60 or higher, (b) having at least a basic educational qualification (that was an indicator of the ability to read and write in English, which was the medium in which questionnaires were administered), and (c) being free of all physical and mental disabilities (e.g., blindness, mental disorders, etc.) that brought into question the ability of participants to provide accurate and objective responses. The study focused on SSNIT for two reasons. First, retired older adults had some formal education and could complete questionnaires in English. Secondly, older adults in the communities (i.e., those not affiliated to the SSNIT) could not be reached, possibly because they were socially excluded. An administrator at the head office of SSNIT in Accra verbally informed older adults who visited the office about the study. Older adults who agreed to participate in the study were shortlisted and subsequently screened with the selection criteria by a research assistant with a medical background. Selected individuals were then informed of their role in the study.
Seven hundred and thirty (730) older adults who met these conditions participated in the study. Sample size calculation was not possible for two reasons. First, there was no applicable sampling frame for the study; hence the researchers needed to recruit participants within the study period. Secondly, there were no similar studies from which relevant statistics (e.g., power, effect size, etc.) needed to compute sample size could be obtained. We, however, deemed our sample size appropriate because similar studies (Bhimla et al. 2019; Portegiis et al. 2020) utilizing logistic regression analysis produced reliable results with sample sizes < 200.
Variables and their operationalisation
The primary dependent variable was the CVD condition, whereas the independent variables (i.e., predictors) are shown in Table 1. CVD condition was measured by asking participants to report clinically diagnosed cardiovascular conditions (e.g., diabetes, hypertension, stroke) they had. The resulting variable was dummy coded into a dichotomous variable (i.e., those with no cardiovascular condition and those with one or more conditions). Table 1 shows the independent variables (including the lifestyle factors such as PA and volunteering) as well as information regarding their measurement and coding. This table shows of how each variable was measured and operationalized.
Data gathering
Questionnaires were delivered by hand to participants in the study area between September 3 and October 31, 2019. To maximize the response rate, participants were asked to respond to questionnaires instantly. Out of 730 questionnaires administered, 697 were completed and returned; however, 11 of these questionnaires were not usable and were discarded. Thus, 686 questionnaires were analysed.
Statistical analysis method
Data were analysed using IBM SPSS Statistics, version 24 (IBM Corporation, NY, USA). Descriptive statistics (i.e., frequency and percentage) were used to summarise the data. Findings were presented using binary logistic regression, but before using this statistical tool, the Pearson's chi-square test was used to assess group differences concerning CVD conditions (see Table 2). At the level of logistic regression, associations were estimated in terms of adjusted odds ratios (ORs) given the control variables incorporated into the analysis. Values of p < .05 were considered statistically significant.
Findings
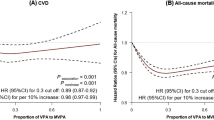
As Table 2 depicts, 9% (n = 63) of all older adults engaged in less than 30 minutes of PA per day, 57% (n = 392) of them engaged in between 30 and 60 minutes of PA per day, and 34% (n = 231) of them engaged in more than 60 minutes of PA per day. In addition, 26% (n = 175) of all older adults engaged in vigorous PA for less than 30 minutes a day, 33% (n = 224) of them engaged in vigorous PA for between 30 and 60 minutes a day, and 42% (n = 287) of them participated in vigorous PA for more than 60 minutes a day. Both moderate (Chi-square = 63.21; p = 0.000) and vigorous PA (Chi-square = 24.29; p = 0.000) are significantly associated with CVD condition. Only smoking (Chi-square = 4.03; p = 0.134) and gender (Chi-square = 2.64; p = 0.104) are not significantly associated with CVD condition.
In Table 3, older adults who less often engaged in volunteering were 24 times (OR =24.39; p = .000) more likely to have one or more CVDs compared with those who never volunteered. Older people who very often engaged in volunteering were also about 2 times (OR =1.83; p = .048) more likely to have one or more CVDs compared with those who never volunteered. In addition, older adults who participated in moderate PA for between 30 and 60 minutes a day were 3 times (OR = 3.34; p = .013) more likely to report having one or more CVDs compared with those who engaged in moderate PA for less than 30 minutes, and older adults who engaged in moderate PA for more than 60 minutes a day were 7 times (OR = 7.00; p = .000) likely to report having one or more CVDs compared with those who engaged in moderate PA for less than 30 minutes. Finally, older people who engaged in more than 60 minutes of vigorous PA a day were 4 times (OR = 3.99; p = .000) more likely to report having one or more CVDs compared with those who participated in less than 30 minutes of vigorous PA a day. In Table 3, sedentary behaviour and lifestyle factors such as smoking and alcohol intake status are significantly associated with CVD condition.
Discussion
This study confirmed that a significant relationship exists between moderate and vigorous PA time and the likelihood of having one or more CVDs, however, this evidence connotes that the risk of CVDs increases with increasing PA. Similarly, the risk of having one or more CVDs increases with the frequency of volunteering but decreases with the frequency of smoking. Interestingly, the confirmed influence of PA, smoking, and volunteering on the risk of CVDs in this study runs counter to most studies in the literature. For example, Lachman et al. (2018) in the Netherlands have reported that the risk of CVDs decreases with increasing PA or if recommended PA levels are met. In Nigeria, PA has been reported to reduce the risk of CVDs in an older population (Oyeyemi and Adeyemi 2013). Supporting our result on the association between PA and CVDs status, though, are studies (Asiamah et al. 2019; Temporelli 2021; Carré 2019) reporting that PA may be associated with injuries and other unwanted outcomes in older adults. Furthermore, many studies including a systematic review conducted by Sun et al. (2013) have indicated that smoking increases the risk of CVDs and other diseases such as lung cancer (Sun et al. 2013; Fini et al. 2017; Abuladze et al. 2017; Eaton 1992; Carnethon 2009; Zhang et al. 2021a, b). Volunteering has also been reported and confirmed as a novel buffer against the risk of diseases, including CVDs (Detollenaere et al. 2017; Zhang et al. 2021a, b).
In the light of the above disagreement, it is unmistakable that the current study opposes some previous studies and as a result presents some implications. The current study reveals that nearly 60% of older adults had one or more CVDs, and moderate and vigorous PA was high in the population. We would therefore want to deduce that older participants had modified their lifestyles recently by increasing their PA in response to their CVD conditions and health. Our result regarding the association between PA and CVDs status is backed by researchers (Asiamah 2019; Temporelli 2021; Carré 2019) indicating that the health benefits of PA are contingent on lifestyle and personal factors such as smoking, diet, and sedentary behaviour. These studies argue that sedentary behaviour can offset the health benefits of PA, so PA may be associated with negative health outcomes such as CVDs status among people who are highly sedentary or inactive. This notwithstanding, we are hesitant to rule out the presence of other covariates in the regression model as a potential cause of the disagreement of our results with most of what the empirical literature accounts for. Thus, because our regression model incorporates a unique set of covariates (including comorbidities and positive and negative lifestyles), these pieces of evidence could suggest the need for future researchers to be more cautious in analysing similar relationships. Understandably, adjusting for all potential confounders and covariates is key to unveiling the true nature of relationships, given that previous studies (Garnvik et al. 2020; Oyeyemi and Adeyemi 2013; Li and Siegrist 2012; Sesso et al. 1999) have not captured PA, sedentary behaviour, comorbidities, healthy and unhealthy lifestyles (behaviours), and demographic variables concurrently in their regression models.
The study affirms sedentary behaviour as a cardiovascular disease risk factor, and therefore endorses health promotion programs aimed at discouraging sedentary behaviour in older populations. It has been observed that more than 90% of older participants in this study participated in moderate PA for at least 30 minutes a day, and about 75% of older participants engaged in vigorous PA for at least 30 minutes. This finding implies that older people engaged in at least 150 minutes each of moderate and vigorous PA a week and as a result met recommended PA levels such as those from the World Health Organization (Bull et al. 2020). If so, the realization of SB as a CVDs risk factor in line with studies conducted in developed (Leung et al. 2017; Bull et al. 2020) and developing (Hajduk and Chaudhry 2016; de Rezende et al. 2014) countries suggests that meeting recommended PA levels does not mean an individual is not sedentary and is not vulnerable to the risks of SB. Even older adults who meet recommended PA levels can be sedentary and susceptible to CVDs. A key lesson from this study, therefore, is that older adults are not only required to keep active but are also expected to avoid sedentary behaviour or keep it as low as possible. Similarly, older people must always be preoccupied with physical and social activities during the day to reduce their sedentary time and maintain health. Given the consistency between our result and previous studies, it could be learned that SB is a major health risk when multiple covariates (including healthy and unhealthy behaviours) are adjusted for in analysing its association with CVD and possibly other health outcomes.
The current study indicates that the risk of CVDs increases with the frequency of alcohol intake, and this finding is much upheld in the empirical literature. While this result is consistent with previous studies conducted in both developed and developing countries (Fini et al. 2017; Abuladze et al. 2017; Liang and Chikritzhs 2013), we consider frequent alcohol consumption a behavioural health hazard that may have contributed to the reversal of the expected impact of PA and volunteering on cardiovascular disease in this study. Though the confirmed relationship between alcohol intake and CVDs in this study is not new, the presence of ‘alcohol intake’ in the regression model as a covariate implies that PA would not necessarily buffer against the risk of CVDs if an older person depends on alcohol. This study as a result discourages excessive intake of alcohol in older populations, especially if individuals expect to make the most of PA. Also in line with popular empirical evidence (Buscail et al. 2017; El Ansari et al. 2015; Burkert et al. 2014) is the result that the frequency of eating meaty and vegetarian diets is also associated with the risk of CVDs, whereby dependence on meaty diets increases the risk of CVDs while living on vegetarian diet decreases such a risk. This result gives weight to the idea that meaty diets increase the amount of fat deposited along the passageway of blood and other body fluids and thus increases the burden of the heart and cardiovascular system (El Ansari et al. 2015; Burkert et al. 2014). This view and result do not,however, mean that meaty food, when eating sparingly, cannot support health and healthy ageing as studies (Hackney et al. 2019; Dobersek et al. 2020; Mena et al. 2020) have reported that meat has essential nutrients that can support individual health.
This study also found that vegetarians were less likely to report one or more CVDs compared to non-vegetarians. This outcome of the study is not new, and supports previous studies (El Ansari et al. 2015; Burkert et al. 2014) that confirmed that living on a vegetarian diet reduces the risk of CVDs and morbidity, but it can be considered special given our unique covariate adjustment. Arguably, findings in correlational studies such as ours are more reliable when covariate adjustment is as complete as possible. We would want to concede that a correlational design is weak and cannot establish causation even in the light of a potentially holistic covariate adjustment. For this reason, we strongly encourage future researchers to advance this study to a longitudinal design that can establish dose–response effects and causation, which in the public health and epidemiological literature are the strongest evidence that could inform policy action. We acknowledge that our measurement of PA as a categorical variable and CVDs as a self-reported measure is a limitation of our study. Though studies (Garnvik et al. 2020; Oyeyemi and Adeyemi 2013; Buffart et al. 2012) have shown that this limitation does not make our results unimportant, the use of objective measures such as accelerometers and pedometers in future research is recommended. Another limitation of this study is that CVD conditions may have been underreported since some participants may be unaware of their CVD status. This study also has limited generalizability as it employed a sample of retired older adults in Accra, most of whom reported having at least one chronic condition. Thus, our result may be typical of older adults who are modifying their lifestyle in response to long-term conditions. Similarly, this study’s findings may not be generalized to older adults living in rural areas because this segment of the population is less educated (compared with the current sample) and may be unable to speak and write in English. Future studies targeting this segment are, therefore, needed. Despite the above limitations, the current study can guide covariate selection in future interventional trials as well as discussions of future pieces of evidence vis-à-vis the extant literature. Finally, our study poses implications that are worth applying in health promotion and public health interventional programs. These implications are identified and discussed later in this paper.
Conclusion
The risk of having one or more CVDs increases as time spent in moderate and vigorous PA increases, possibly because 58% (n = 399) of older adults in our study had one or more CVDs and were possibly responding to recommended PA levels to maintain or improve health. Moreover, older adults who volunteered less often and very often were respectively 24 and 2 times more likely to report having one or more CVDs compared with those who never volunteered. Individuals who drank alcohol a few times or several times a week were more likely to report having one or more CVDs as compared with those who never drank alcohol. This result means that frequent alcohol intake increases the risk of CVDs. Older people who engaged in SB most hours of the day and a few hours of the day were 4 times likely to report having one or more CVDs compared to those who were sedentary at all times, which confirms that sedentary behaviour can increase the risk of CVDs in older populations. Vegetarians were also less likely to report having one or more CVDs compared with non-vegetarians. If so, living on a diet rich in vegetables and fruits reduces the risk of CVD. Interestingly, older people who never ate ‘meaty food’ (i.e., meat or food containing meat) were 8 times more likely to report having one or more CVDs. This study concludes that when key lifestyle factors and personal variables are adjusted for, PA increases the risk of CVD, but this outcome may be an explanation of older adults’ effort to enhance their PA levels upon knowing they have one or more CVDs.
Implications for health promotion
Our evidence indicates that older participants recently modified their lifestyles in response to their health and CVD conditions. This study consequently implies that health promotion campaigns in Ghana and possibly other developing countries are sitting well with older populations. The belief has been that such campaigns and educational programs are either not enough or not adhered to in developing African countries (Abuladze et al. 2017; Oyeyemi and Adeyemi 2013; Park et al. 2018). Our evidence may thus serve as an incentive for stakeholders (e.g., researchers, public health organizations, and governments) to intensify health promotion programs, especially awareness-creation efforts focused on such themes as “active living” (used to emphasize the need for all, including older people, to remain active and meet recommended PA levels), "healthy ageing" (used to promote general behaviours that can support the health of seniors), and “smart cities” (used to educate people regarding what they can do to make the most of communities that provide social resources for healthy ageing).
It is impressive that most older adults met recommended PA levels, but they indulged in some level of sedentary behaviour that may have led to their health and CVD condition being unimpacted or less impacted by PA. Of course, the possibility that SB is a factor that makes PA a cardiovascular disease risk factor (as our finding indicates) cannot be ruled out. This study, therefore, suggests that individual efforts to increase PA are as good as pursuing a life devoid of sedentary behaviour. More so, health promotion programs, especially “active living” campaigns, should always stress the need for older people to engage in PA regularly and avoid SB simultaneously. Health educators must also portray SB as a lifestyle that can render PA unbeneficial, especially if its recommended levels are not met. In this regard, stakeholders must adapt their viral health promotion campaigns by, for example, not just endorsing constant uptake of PA as a healthy behaviour but also emphasizing the need for recommended PA levels to be met on a daily or weekly basis.
Drinking alcohol more frequently also comes with a higher risk of having one or more CVDs, an outcome that supports measures being taken to discourage or at least minimize excessive intake of alcohol in the general and older populations. About 66% of older participants' dependence on alcohol may have also reversed the expected association between PA and CVD condition. Hence, alcohol consumption can contribute to the elimination or reversal of the desired impact of PA on the risk of CVDs. Given this finding, health promotion programs that tend to uphold constant uptake of PA as a healthy behaviour must also discourage the excessive intake of alcohol by older adults. Additionally, whatever measures are tailored by stakeholders towards discouraging SB and encouraging PA must not only take unhealthy behaviours (alcohol intake, smoking, poor dieting, etc.) into account but must also discourage these behaviours. Researchers, public health personnel, and health promoters must always accompany their message of active living with the advice that anyone who engages in negative lifestyles such as smoking, drinking alcohol, and sedentary behaviour cannot benefit from PA or may make minimal gains from meeting WHO’s recommended PA levels. That is to say that health education geared towards increasing PA in older populations must go together with promotional efforts that discourage the said negative lifestyles.
Availability of data and material
Available upon request
Code availability
Not applicable
References
Abuladze L, Kunder N, Lang K, Vaask S (2017) Associations between self-rated health and health behaviour among older adults in Estonia: a cross-sectional analysis. BMJ Open 7:1–9. https://doi.org/10.1136/bmjopen-2016-013257
Asiamah N, Mensah HK (2017) The association between work-related physical activity and depression. J Phys Activity Res 2(1):1–6. https://doi.org/10.12691/jpar-2-1-1
Asiamah N, Kouveliotis K, Petersen C, Eduafo R, Borkey R (2019) Injuries, dislocations, and poor health perceived by older adults to result from vigorous physical activity: implications for active living, health promotion, and gerontology. Adv Gerontol = Uspekhi Gerontologii 32(4):652–657
Bennett DA, Du H, Clarke R, Guo Y, Yang L, Bian Z, Chen Y, Millwood I, Yu C, He P, Zheng X, Collins R, Chen J, Peto R, Li L, Chen Z, China Kadoorie Biobank Study Collaborative Group (2017) Association of physical activity with risk of major cardiovascular diseases in chinese men and women. JAMA Cardiol 2(12):1349–1358. https://doi.org/10.1001/jamacardio.2017.4069
Bhimla A, Gadegbeku C, Tan Y, Zhu L, Aczon F, Ma G (2019) A study of physical activity determinants among high-risk hypertensive Filipino and Korean Americans. Int J Environ Res Public Health 16(7):1–13. https://doi.org/10.3390/ijerph16071156
Buecker S, Simacek T, Ingwersen B, Terwiel S, Simonsmeier BA (2020) Physical activity and subjective well-being in healthy individuals: a meta-analytic review. Health Psychol Rev 15(4):574–592. https://doi.org/10.1080/17437199.2020.1760728
Buffart LM, Thong MSY, Schep G, Chinapaw MJM, Brug J, van de Poll-Franse LV (2012) Self-reported physical activity: its correlates and relationship with health-related quality of life in a large cohort of colorectal cancer survivors. Plos One 7(5):1–9. https://doi.org/10.1371/journal.pone.0036164
Bull FC et al (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British J Sports Med 54:1451–1462. https://doi.org/10.1136/bjsports-2020-102955
Burkert NT, Muckenhuber J, Großschädl F, Rásky É, Freidl W (2014) Nutrition and health — the association between eating behavior and various health parameters: a matched sample study. PLoS One 9(2):1–7. https://doi.org/10.1371/journal.pone.0088278
Buscail C, Sabate JM, Bouchoucha M, Torres MJ, Allès B, Hercberg S, Benamouzig R, Julia C (2017) Association between self-reported vegetarian diet and the irritable bowel syndrome in the French NutriNet cohort. PLoS One 12(8):1–16. https://doi.org/10.1371/journal.pone.0183039
Carnethon MR (2009) Physical activity and cardiovascular disease: how much is enough? Am J Lifestyle Med 3(1):44S–49S. https://doi.org/10.1177/1559827609332737
Carré F (2019) Physical activity as the cure-all, is it always true? Eur J Prevent Cardiol 26(17):1874–1876. https://doi.org/10.1177/2047487319862068
de Rezende LFM, Rey-López JP, Matsudo VKR, Luiz OC (2014) Sedentary behaviour and health outcomes among older adults: a systematic review. BMC Public Health 14:1–9. https://doi.org/10.1186/1471-2458-14-333
Detollenaere J, Willems S, Baert S (2017) Volunteering, income and health. PLoS One 12(3):1–11. https://doi.org/10.1371/journal.pone.0173139
Dobersek U, Wy G, Adkins J, Altmeyer S, Krout K, Lavie CJ, Archer E (2020) Meat and mental health: a systematic review of meat abstention and depression, anxiety, and related phenomena. Crit Rev Food Sci Nutrition 2020:1–14. https://doi.org/10.1080/10408398.2020.1741505
Eaton CB (1992) Relation of physical activity and cardiovascular fitness to coronary heart disease, part i: a meta-analysis of the independent relation of physical activity and coronary heart disease. J Am Board Family Pract 5:31–42
El Ansari W, Suominen S, Berg-Beckhoff G (2015) Is healthier nutrition behaviour associated with better self-reported health and less health complaints? Evidence from Turku, Finland. Nutrition 7:8478–8490. https://doi.org/10.3390/nu7105409
Fini NA, Bernhardt J, Holland AE (2017) What is the relationship between physical activity and cardiovascular risk factors in stroke survivors post completion of rehabilitation? Protocol for a longitudinal study. BMJ Open 7:1–5. https://doi.org/10.1136/bmjopen-2017-019193
Garnvik LE, Malmo V, Janszky I, Ellekjær H, Wisløff U, Loennechen JP, Nes BM (2020) Physical activity, cardiorespiratory fitness, and cardiovascular outcomes in individuals with atrial fibrillation: the HUNT study. Eur Heart J 41(15):1467–1475. https://doi.org/10.1093/eurheartj/ehaa032
Granger E, Williams G, Di Nardo F, Harrison A, Verma A (2017) The relationship between physical activity and self-rated health status in European adolescents: results of the EURO-URHIS 2 survey. Eur J Public Health 27(2):107–111. https://doi.org/10.1093/eurpub/ckw177
Hackney KJ, Trautman K, Johnson N, Mcgrath R, Stastny S (2019) Protein and muscle health during aging: benefits and concerns related to animal-based protein. Animal Front 9(4):12–17. https://doi.org/10.1093/af/vfz030
Hajduk AM, Chaudhry SI (2016) Sedentary behavior and cardiovascular risk in older adults: a scoping review. Curr Cardiovasc Risk Rep 10(1):1–17. https://doi.org/10.1007/s12170-016-0485-6
Higueras-Fresnillo S, Guallar-Castillón P, Cabanas-Sanchez V, Banegas JR, Rodríguez-Artalejo F, Martinez-Gomez D (2017) Changes in physical activity and cardiovascular mortality in older adults. J Geriatric Cardiol 14:280–281. https://doi.org/10.11909/j.issn.1671-5411.2017.04.009
Holtermann A, Schnohr P, Nordestgaard BG, Marott JL (2021) The physical activity paradox in cardiovascular disease and all-cause mortality: the contemporary Copenhagen General Population Study with 104,046 adults. Eur Heart J 42(15):1499–1511. https://doi.org/10.1093/eurheartj/ehab087
Lachman S, Boekholdt SM, Luben RN, Sharp SJ, Brage S, Khaw K, Peters RJG, Wareham NJ (2018) Impact of physical activity on the risk of cardiovascular disease in middle-aged and older adults: EPIC Norfolk prospective population study. Eur J Prevent Cardiol 25(2):200–208. https://doi.org/10.1177/2047487317737628
Leung P, Ejupi A, van Schooten KS, Aziz O, Feldman F, Mackey DC, Ashe MC, Robinovitch SN (2017) Association between sedentary behaviour and physical, cognitive, and psychosocial status among older adults in assisted living. BioMed Res Int 2017:1–7. https://doi.org/10.1155/2017/9160504
Li J, Siegrist JS (2012) Physical activity and risk of cardiovascular disease—a meta-analysis of prospective cohort studies. Int J Environ Res Public Health 9:391–407. https://doi.org/10.3390/ijerph9020391
Liang W, Chikritzhs T (2013) The association between alcohol exposure and self-reported health status: the effect of separating former and current drinkers. PLoS One 8(2):1–5. https://doi.org/10.1371/journal.pone.0055881.g003
Mena B, Ashman H, Dunshea FR, Hutchings S, Ha M, Warner RD (2020) Exploring meal and snacking behaviour of older adults in Australia and China. Foods 9(4):1–24. https://doi.org/10.3390/foods9040426
Oyeyemi AL, Adeyemi O (2013) Relationship of physical activity to cardiovascular risk factors in an urban population of Nigerian adults. Arch Public Health 71(6):1–9. https://doi.org/10.1186/0778-7367-71-6
Park J, Joh J, Lee G, Je S, Cho S, Kim S, Oh S, Kwon H (2018) Association between sedentary time and cardiovascular risk factors in Korean adults. Korean J Family Med 39:29–36. https://doi.org/10.4082/kjfm.2018.39.1.29
Portegijs E, Keskinen KE, Eronen J, Saajanaho M, Rantakokko M, Rantanen T (2020) Older adults’ physical activity and the relevance of distances to neighborhood destinations and barriers to outdoor mobility. Front Public Health 8:1–11. https://doi.org/10.3389/fpubh.2020.00335
Ramakrishnan R, Doherty A, Smith-Byrne K, Rahimi K, Bennett D, Woodward M, Walmsley R, Dwyer T (2021) Accelerometer measured physical activity and the incidence of cardiovascular disease: Evidence from the UK Biobank cohort study. PLoS Med 18(1):1–16. https://doi.org/10.1371/journal.pmed.1003487
Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J (2016) Independent associations between sedentary behaviors and mental, cognitive, physical, and functional health among older adults in retirement communities. J Gerontol Med Sci 71(1):78–83. https://doi.org/10.1093/gerona/glv103
Sesso HD, Paffenbarger RS, Ha T, Lee I (1999) Physical activity and cardiovascular disease risk in middle-aged and older women. Am J Epidemiol 150(4):408–416. https://doi.org/10.1093/oxfordjournals.aje.a010020
Sun F, Norman IJ, While AE (2013) Physical activity in older people: a systematic review. BMC Public Health 13:1–17. https://doi.org/10.1186/1471-2458-13-449
Temporelli PL (2021) Is physical activity always good for you? The physical activity paradox. Eur Heart J Suppl 23:168–171. https://doi.org/10.1093/eurheartj/suab115
Zhang X, Liu Y, Li S, Lichtenstein AH, Chen S, Na M, Veldheer S, Xing A, Wang Y, Wu S, Gao X (2021a) Alcohol consumption and risk of cardiovascular disease, cancer and mortality: a prospective cohort study. Nutrition J 20(1):1–10. https://doi.org/10.1186/s12937-021-00671-y
Zhang S, Xiang K, Li S, Pan HF (2021b) Physical activity and depression in older adults: the knowns and unknowns. Psychiat Res 297:1–8. https://doi.org/10.1016/j.psychres.2021.113738
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
NA conceived the research idea, wrote the original manuscript, and analysed the data. KK and CP critically reviewed the draft manuscript. RE and RB supervised data collection and analysis. All authors proofread and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval
The study received ethics approval from an institutional ethics review board in Accra (No. 001ACE-2018) after the study protocol was reviewed.
Consent to participate
All participants were required to sign an informed consent form to confirm and formalize their voluntary participation in the study.
Consent for publication
Not applicable
Conflict of interest statement
None declared.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Asiamah, N., Kouveliotis, K., Petersen, C. et al. Physical activity time and lifestyle correlates of cardiovascular disease status in older adults in Accra. J Public Health (Berl.) 31, 1453–1462 (2023). https://doi.org/10.1007/s10389-022-01712-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-022-01712-4