Abstract
Background
Ultrasonic activated devices (USADs) may produce inadvertent injuries due to heat or shock waves. However, thermal injury and shock waves are considered to be avoidable if these devices are used appropriately.
Methods
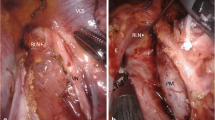
Utilizing a porcine model, we examined the relationship between the occurrence of tissue damage around the iliac artery and sciatic nerve and the usage of an USAD. Thereafter, we prospectively determined the clinical outcomes following the usage of the USAD during dissection along the recurrent laryngeal nerves (RLN) in 114 consecutive patients who underwent thoracoscopic esophageal surgery.
Results
The temperatures measured in the pig iliac artery and sciatic nerve more than 2 mm from the activating blade (at a power setting of 70 %, within 2 s) did not increase to 42 °C. In a subsequent clinical series using the short activating technique according to the findings of in vivo experiments, scheduled laryngoscopic studies showed the rate of vocal cord palsy after esophagectomy to be 39 %, which was more sensitive than the substantial presence of hoarseness (28 %).
Conclusions
Adverse effects by using the USAD on the nerves may be avoidable if the activation of the current using an USAD is conducted within 2 s at positions more than 2 mm from the nerves. This short activation technique using the USAD is therefore considered to be safe and feasible for lymph node dissection along the RLNs during thoracoscopic esophagectomy, although the apparent reasons for postoperative dysfunction in the vocal cords remain unclear.



Similar content being viewed by others
References
Feder BJ. Surgical device poses a rare but serious peril. New York Times, March 17; Business Section Page 17, 2006.
Kadesky KM, Schopf B, Blair GK. Proximity injury by the ultrasonically activated scalpel during dissection. J Paediatr Surg. 1997;32:878–9.
Emam TA, Cuschieri A. How safe is high-power ultrasonic dissection? Ann Surg. 2003;237:186–91.
Govekar HR, Robinson TN, Stiegmann GV, et al. Residual heat of laparoscopic energy devices: how long must the surgeon wait to touch additional tissue? Surg Endosc. 2011;25:3499–502.
Gockel I, Kneist W, Keilmann A, et al. Recurrent laryngeal nerve paralysis (RLNP) following esophagectomy for carcinoma. Eur J Surg Oncol. 2005;31:277–81.
Johnson PR, Kanegoanker GS, Bates T. Indirect laryngoscopic evaluation of vocal cord function in patients undergoing transhiatal esophagectomy. J Am Coll Surg. 1994;178:605–8.
Akiyama H, Tsurumaru M, Udagawa H, et al. Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg. 1994;220:364–72.
Udagawa H, Ueno M, Shinohara H, et al. The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol. 2012;106:742–7.
Ikeda Y, Inoue T, Ogawa E, et al. Recurrent laryngeal nerve monitoring during thoracoscopic esophagectomy. World J Surg. 2014;38:897–901.
Feng M, Shen Y, Wang H. Thoracolaparoscopic esophagectomy: is the prone position a safe alternative to the decubitus position? J Am Coll Surg. 2012;214:838–44.
Shen Y, Zhang Y, Tan L, et al. Extensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single center. J Gastrointest Surg. 2012;16:715–21.
Daiko H, Nishimura M. A pilot study of the technical and oncologic feasibility of thoracoscopic esophagectomy with extended lymph node dissection in the prone position for clinical stage I thoracic esophageal carcinoma. Surg Endosc. 2012;26:673–80.
Kinjo Y, Kurita N, Nakamura F, et al. Effectiveness of combined thoracoscopic–laparoscopic esophagectomy: comparison of postoperative complications and midterm oncological outcomes in patients with esophageal cancer. Surg Endosc. 2012;26:381–90.
Ninomiya I, Osugi H, Fujimura T, et al. Thoracoscopic esophagectomy with extended lymph node dissection in the left lateral position: technical feasibility and oncologic outcomes. Dis Esophagus. 2014;27:159–67.
Suda K, Ishida Y, Kawamura Y, et al. Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: technical report and short-term outcomes. World J Surg. 2012;36:1608–16.
Taniyama Y, Miyata G, Kamei T, et al. Complications following recurrent laryngeal nerve lymph node dissection in oesophageal cancer surgery. Interact Cardiovasc Thorac Surg. 2015;20:41–6.
Okuyama M, Motoyama S, Suzuki H, et al. Hand-sewn cervical anastomosis versus stapled intrathoracic anastomosis after esophagectomy for middle or lower thoracic esophageal cancer: a prospective randomized controlled study. Surg Today. 2007;37:947–52.
Perry KA, Enestvedt CK, Diggs BS, et al. Perioperative outcomes of laparoscopic transhiatal inversion esophagectomy compare favorably with those of combined thoracoscopic-laparoscopic esophagectomy. Surg Endosc. 2009;23:2147–54.
Kim DJ, Park SY, Lee S, et al. Feasibility of a robot-assisted thoracoscopic lymphadenectomy along the recurrent laryngeal nerves in radical esophagectomy for esophageal squamous carcinoma. Surg Endosc. 2014;28:1866–73.
Noshiro H, Iwasaki H, Kobayashi K, et al. Lymphadenectomy along the left recurrent laryngeal nerve by a minimally invasive esophagectomy in the prone position for thoracic esophageal cancer. Surg Endosc. 2010;24:2965–73.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Owaki T, Nakano S, Arimura K, et al. The ultrasonic coagulating and cutting system injures nerve function. Endoscopy. 2002;34:575–9.
Xu D, Pollock M. Experimental nerve thermal injury. Brain. 1994;117:375–84.
Shimi SM. Dissection techniques in laparoscopic surgery: a review. J R Coll Surg Edinb. 1995;40:249–59.
Engstad K, Schipper PH. Laryngopharyngeal dysfunction after esophagectomy. In: Jobe BA, Thomas CR, Hunter JG, editors. Esophageal cancer: principles and practice. New York: Demos Medical Publishing; 2009. p. 660–1.
Gelpke H, Grieder F, Decurtins M, et al. Recurrent laryngeal nerve monitoring during esophagectomy and mediastinal lymph node dissection. World J Surg. 2010;34:2379–82.
Rino Y, Yukawa N, Sato T, et al. Using NU-KNIT® for hemostasis around recurrent laryngeal nerve during transthoracic esophagectomy with lymphadenectomy for esophageal cancer. BMC Res Notes. 2014;7:127.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
This study conforms to the guidelines set forth in the Declaration of Helsinki revised in 2000. We have protected the privacy of the patient, and the manuscript does not include any identifying information. All institutional and national guidelines for the care and use of laboratory animals were followed. This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of interest
Drs. Hirokazu Noshiro, Keita Kai, Yukie Yoda, Hiroshi Kono, and Akihiko Uchiyama have no conflicts of interest or financial ties to disclosure.
Rights and permissions
About this article
Cite this article
Noshiro, H., Kai, K., Yoda, Y. et al. Palsy of the recurrent laryngeal nerves in association with an ultrasonic activated device during thoracoscopic esophagectomy with three-field lymphadenectomy. Esophagus 13, 351–360 (2016). https://doi.org/10.1007/s10388-016-0543-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-016-0543-7