Summary
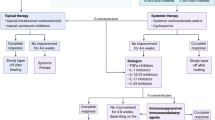
Pyoderma gangrenosum (PG) represents a rare skin disorder, with several clinical variants and still not fully understood ethiopathogenesis. Often associated with inflammatory or neoplastic disease, PG is nowadays considered an inflammatory neutrophilic disease with common underlying morbidity. Modern treatment options are oriented towards key mechanisms underlying the pathogenesis of the disease, namely inflammatory mediators, and seem to be the most effective treatment currently available. Although promising, the results are not invariable and these treatments are sometimes surrounded by controversy, as recent studies have reported cases that are refractory to therapy with biological agents. It is possible that refractoriness to the use of biological agents as monotherapy stems from the fact that a single agent is not able to affect the entire inflammatory cascade, or to simultaneously influence all of its levels. Based on the pathogenesis of inflammation, we can suggest that an ideal targeted therapy should be able to induce the following changes: 1) reduction of the secretion of interleukin (IL)-1a/b from the inflammasome with subsequent blocking of its biological effect (by therapy with IL-1 receptor antagonists); 2) blocking of the activation of the secreted procytokines in their active form (by therapy with caspase-1 inhibitors; 3) blocking of the effect of the already released active cytokines (by therapy with tumour necrosis factor alpha, TNF-α, inhibitors); 4) blocking of the effector action of the cytokines on the target intracellular molecules (by therapy with kinase inhibitors). The specific therapy should aim to attack more than one link in the inflammatory cascade, in order to achieve maximum therapeutic effectiveness. Most surely, this could be achieved with combined therapy with different groups of biological agents (for example a combined therapy with IL-1 receptor antagonist and a TNF-α inhibitor). Currently, no data in the literature exist to support this statement, and there are no safety data relating to such approaches. We focus this review on the novel etiopathogenetic concepts of PG and the future therapeutic approaches based on blocking different levels of the inflammatory cascade, which seems to be the most promising weapon in the target-oriented treatment options.
Zusammenfassung
Das Pyoderma gangraenosum (PG) ist eine seltene Hauterkrankung mit verschiedenen klinischen Subtypen und einer noch immer nicht komplett verstandenen Ätiopathogenese. Das PG wird als entzündliche neutrophile Dermatose verstanden, die oftmals eine Assoziation zu anderen entzündlichen oder neoplastischen Erkrankungen zeigt. Moderne Behandlungsansätze orientieren sich an den Schlüsselpositionen der zugrunde liegenden Pathogenese, insbesondere den inflammatorischen Mediatorsubstanzen. Sie verkörpern die derzeit effektivsten Therapieoptionen. Obwohl der Ansatz durchaus erfolgversprechend ist, sind die klinischen Resultate nicht konstant. Der Umstand sog. therapierefraktärer Fälle gegenüber einer zielgerichteten Therapie wird kontrovers diskutiert. Dieses Therapieversagen könnte jedoch auch daher rühren, dass eine Monotherapie mit Biologika nicht in der Lage ist, die gesamte Entzündungskaskade zu beeinflussen bzw. gleichermaßen simultan zu kontrollieren. Auf der Entzündungspathogenese basierend schlagen die Autoren für eine ideale Therapie folgende Eckpunkte vor: 1) Verminderung der IL-1a/b-Sekretion des Inflammasoms mit nachfolgender Blockade ihrer biologischen Wirkung (durch Einsatz von IL-1-Rezeptorantagonisten); 2) Blockade der Aktivierung sezernierter Prozytokine in ihrer aktiven Form (durch Einsatz von Caspase-1-Inhibitoren; 3) Hemmung der bereits sezernierten Zytokine (durch TNF-α-Inhibitoren); 4) Blockade der Effektoraktion der Zytokine auf entsprechende intrazelluläre Moleküle (mittels Kinaseinhibitoren). Die spezifische Therapie sollte an mehreren Schnittstellen der Entzündungskaskade angreifen, um eine maximale Wirkung zu entfalten. Aller Wahrscheinlichkeit nach lässt sich dieses Ziel nur durch Kombination verschiedener Biologika errreichen (z. B. eine Kombination von IL-1-Rezeptorantagonist und TNF-α-Inhibitor). Allerdings existieren derzeit noch keine harten wissenschaftlichen Daten, die dieses Konzept unterstützen. Ein weiterer ungeklärter Aspekt ist die Patientensicherheit. Die vorliegende Übersicht fokussiert auf neue ätiopathogenetische Konzepte zum PG und daraus abzuleitende zukünftige Behandlungsansätze, die auf dem Prinzip basieren, die Entzündungskaskade auf verschiedenen Ebenen zu unterbrechen. Dies scheint der erfolgversprechendste Ansatz einer zielgerichteten Therapie zu sein.

Similar content being viewed by others
References
Cozzani E, Gasparini G, Parodi A. Pyoderma gangrenosum: a systematic review. G Ital Dermatol Venereol. 2014;149(5):587–600.
Wollina U, Tchernev G. Pyoderma gangrenosum: pathogenetic oriented treatment approaches. Wien Med Wochenschr. 2014;164:263.
Gameiro А, Pereira N, Cardoso JC, Margarida Gonçalo M. Pyoderma gangrenosum: challenges and solutions. Clin Cosmet Investig Dermatol. 2015;8:285–93.
Argüelles-Arias F, Castro-Laria L, Lobatón T, Aguas-Peris M, Rojas-Feria M, Barreiro-de Acosta M, Soto-Escribano P, Calvo-Moya M, Ginard-Vicens D, Chaparro-Sánchez M, Hernández-Durán M, Castro-Senosiain B, Fernández-Villaverde A, García-Sánchez V, Domínguez-Muñoz E, Caunedo-Álvarez A, Herrerías-Gutiérrez JM. Characteristics and treatment of pyoderma gangrenosum in inflammatory bowel disease. Dig Dis Sci. 2013;58(10):2949–54.
Beer HD, Contassot E, French LE. The inflammasomes in autoinflammatory diseases with skin involvement. J Invest Dermatol. 2014;134(7):1805–10.
Wollina U. Clinical management of pyoderma gangrenosum. Am J Clin Dermatol. 2002;3:149–58.
Lipsker D, Lenormand C. Indications and modes of use for interleukin (IL)-1 antagonists in inflammatory dermatosis: a new therapeutic approach to immune-mediated inflammatory diseases. Ann Dermatol Venereol. 2012;139(6–7):459–67.
Braun-Falco M, Kovnerystyy O, Lohse P, Ruzicka TJ. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH) – a new autoinflammatory syndrome distinct from PAPA syndrome. Am Acad Dermatol. 2012;66(3):409–15.
Charles A. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117(14):3720–32.
Lukens JR, Kanneganti TD. SHP-1 and IL-1α conspire to provoke neutrophilic dermatoses. Rare Dis. 2014;2:e27742.
Dinarello CA, Meer JW van der. Treating inflammation by blocking interleukin-1 in humans. Semin Immunol. 2013;pii: S1044-5323(13):00089–00084.
Doherty TA, Brydges SD, Hoffman HM. Autoinflammation: translating mechanism to therapy. J Leukoc Biol. 2011;90(1):37–47.
Jaeger T, Andres C, Grosber M, Zirbs M, Hein R, Ring J, Traidl-Hoffmann C. Pyoderma gangrenosum and concomitant hidradenitis suppurativa – rapid response to canakinumab (anti-IL-1b). Eur J Dermatol. 2013;23(3):408–10.
Church LD, Cook GP. Michael F McDermott. Primer: inflammasomes and interleukin 1 bold beta in inflammatory disorders. Nat Clin Pract Rheumatol. 2008;4:34–42.
Arend WP. The mode of action of cytokine inhibitors. J Rheumatol Suppl. 2002;65:16–21.
Dinarello CA, Simon A, Meer JWM van der. Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat Rev Drug Discov. 2012;11(8):633–52.
Oka M, Berking C, Nesbit M, Satyamoorthy K, Schaider H, Murphy G, Ichihashi M, Sauter E, Herlyn M. Interleukin-8 overexpression is present in pyoderma gangrenosum ulcers and leads to ulcer formation in human skin xenografts. Lab Invest. 2000;80(4):595–604.
Rallis E, Koumantaki-Mathioudaki E, Tsiatoura A, Stavropoulos P, Katsambas A. Pyoderma gangrenosum and tumor necrosis factor α agents. Cutis. 2013;92(4):E1–2.
Callus BA, Vaux DL. Caspase inhibitors: viral, cellular and chemical. Cell Death Differ. 2007;14:73–8.
Zippi M, Pica R, De Nitto D, Paoluzi P. Biological therapy for dermatological manifestations of inflammatory bowel disease. World J Clin Cases. 2013;1(2):74–8.
Kleinpenning MM, Langewouters AM, Van De Kerkhof PC, Greebe RJ. Severe pyoderma gangrenosum unresponsive to etanercept and adalimumab. J Dermatolog Treat. 2011;22:261–5.
Tchernev G, Trebing D, Göring H‑D, Steinhoff M, Zouboulis CC, Orfanos C. Pyoderma gangrenosum in Crohn’s disease – the role of immunologic parameters and histological data in diagnosis and differential diagnosis. Bulg J Hepatogastroenterol. 2005;7:56–60.
Tan MH, Gordon M, Lebwohl O, George J, Lebwohl MG. Improvement of Pyoderma gangrenosum and psoriasis associated with Crohn disease with anti-tumor necrosis factor alpha monoclonal antibody. Arch Dermatol. 2001;137:930–3.
Teich N, Klugmann T. Rapid improvement of refractory pyoderma gangrenosum with infliximab gel in a patient with ulcerative colitis. J Crohns Colitis. 2014;8(1):85–6.
Alexis AF, Strober BE. Off-label dermatologic uses of anti-TNF-α therapies. J Cutan Med Surg. 2005;9(6):296–302.
Vitale A, Rigante D, Lucherini OM, Caso F, Muscari I, Magnotti F, Brizi MG, Guerrini S, Patti M, Punzi L, Galeazzi M, Cantarini L. Biological treatments: new weapons in the management of monogenic autoinflammatory disorders. Mediat Inflamm. 2013;2013:939847.
Wollina U, Hansel G, Koch A, Schönlebe J, Köstler E, Haroske G. Tumor necrosis factor-alpha inhibitor-induced psoriasis or psoriasiform exanthemata: first 120 cases from the literature including a series of six new patients. Am J Clin Dermatol. 2008;9:1–14.
Chen TL, Chang CC, Lin YL, Ueng YF, Chen RM. Signal-transducing mechanisms of ketamine-caused inhibition of interleukin-1 beta gene expression in lipopolysaccharide-stimulated murine macrophage-like Raw 264.7 cells. Toxicol Appl Pharmacol. 2009;240(1):15–25.
Wu GJ, Chen TL, Ueng YF, Chen RM. Ketamine inhibits tumor necrosis factor-alpha and interleukin-6 gene expressions in lipopolysaccharide-stimulated macrophages through suppression of toll-like receptor 4‑mediated c‑Jun N‑terminal kinase phosphorylation and activator protein-1 activation. Toxicol Appl Pharmacol. 2008;228(1):105–13.
Pazyar N, Feily A, Yaghoobi R. An overview of interleukin-1 receptor antagonist, anakinra, in the treatment of cutaneous diseases. Curr Clin Pharmacol. 2012;7(4):271–5.
Brenner M, Ruzicka T, Plewig G, Thomas P, Herzer P. Targeted treatment of pyoderma gangrenosum in PAPA (pyogenic arthritis, pyoderma gangrenosum and acne) syndrome with the recombinant human interleukin-1 receptor antagonist anakinra. Br J Dermatol. 2009;161(5):1199–201.
Geusau A, Mothes-Luksch N, Nahavandi H, Pickl WF, Wise CA, Pourpak Z, Ponweiser E, Eckhart L, Sunder-Plassmann R. Identification of a homozygous PSTPIP1 mutation in a patient with a PAPA-like syndrome responding to canakinumab treatment. JAMA Dermatol. 2013;149(2):209–15.
Gönül M, Cevirgen Cemil B, Keseroglu HO, Kaya Akis H. New Described Dermatological Disorders. Biomed Res Int. 2014;2014:616973.
Bruzzese V. Pyoderma gangrenosum, acne conglobata, suppurative hidradenitis, and axial spondyloarthritis: efficacy of anti-tumor necrosis factor α therapy. J Clin Rheumatol. 2012;18(8):413–5.
Powell FC, O’Kane M. Management of pyoderma gangrenosum. Dermatol Clin. 2002;20:347–55.
Wollina U. Pyoderma gangrenosum – a review. Orphanet J Rare Dis. 2007;2:19.
Powell FC, Su WP, Perry HO. Pyoderma gangrenosum: Classification and management. J Am Acad Dermatol. 1996;34:395–409.
Goodarzi H, Sivamani RK, Garcia MS, Wehrli LN, Craven H, Ono Y, Maverakis E. Effective Strategies for the Management of Pyoderma Gangrenosum. Adv Wound Care (New Rochelle). 2012;1(5):194–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.A. Chokoeva, J.C. Cardoso, U. Wollina and G. Tchernev declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Chokoeva, A.A., Cardoso, J.C., Wollina, U. et al. Pyoderma gangrenosum—a novel approach?. Wien Med Wochenschr 167, 58–65 (2017). https://doi.org/10.1007/s10354-016-0472-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-016-0472-z