Summary
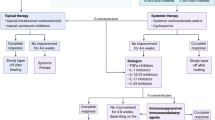
Pyoderma gangrenosum (PG) shows features of autoimmune and autoinflammatory disorders. Genetic defects which affect the inflammasome, and in particular the NLRP3 zone, can cause an abnormal secretion of interleukin 1 (IL-1). IL-1 may be involved in clinical manifestation of certain (genetic) forms of PG. IL-1 receptor antagonists reduce the activity of IL-1α and IL-1β. Mutations in the PSTPIP1 gene have been identified in patients with pyogenic arthritis, pyoderma gangrenosum and acne syndrome. In patients with a pyoderma gangrenosum, acne, and suppurative hidradenitis syndrome these mutations cannot be found and the effect of IL-1 inhibition is questionable. Another upcoming opportunity is targeted therapy by tumor necrosis factor-alfa inhibitors in steroid-resistant patients. This review has been focused on (1) the modern pathogenetic concepts, (2) the currently accepted criteria for differentiating the disease, (3) the target therapy and (4) valuable advice to the clinicians regarding a number of medicaments capable of aggravating or inducing the PG.
Zusammenfassung
Das Pyoderma gangraenosum (PG) weist Symptome der autoimmunen und autoinflammatorischen Erkrankungen auf. Genetische Defekte, die das Inflammasom beeinflussen, insbesondere die NLRP3-Zone, können zur abnormen Sekretion von Interleukin 1 (IL-1) führen. IL-1 scheint bei der klinischen Manifestation bestimmter (genetischer) Typen des PG beteiligt zu sein. IL-1-Rezeptorantagonisten reduzieren die Aktivität von IL-1α und IL-1β. Mutationen im PSTPIP1-Gen sind bei Patienten mit dem PAPA-Syndrom beobachtet worden. Bei Patienten mit einem PASH-Syndrom ließen sich derartige Mutationen nicht nachweisen. Hier ist der Einsatz von IL-1-Antagonisten fragwürdig. Eine weitere Option für steroid-resistente PG-Patienten stellt die zielgerichtete Behandlung mit Tumornekrosefaktor-a-Inhibitoren dar. In dieser Übersicht widmen wir uns folgenden Themen: 1) den modernen pathogenetischen Konzepten, 2) den aktuellen diagnostischen Kriterien, 3) der targeted therapy und 4) Hinweisen zur Induktion oder Aggravation des PG durch Medikamente.




Similar content being viewed by others
Abbreviations
- ANA:
-
Antinuclear antibodies
- ASC:
-
Apoptosis-associated speck-like protein possessing a caspase-recruiting domain (identical to TMS1)
- CAMPS:
-
CARD 14 mediated psoriasis
- CAPS:
-
Cryopyrin-associated periodic syndrome
- CARD14:
-
Caspase recruitment domain-coding protein 14
- CINCA:
-
Chronic infantile neurologic cutaneous and articular syndrome
- DIRA:
-
Deficiency of interleukin-1 receptor antagonist
- ECMPS:
-
Enteric-coated mycophenolate mofetil
- EO-IBD:
-
Early-onset inflammatory bowel diseases
- FACS:
-
Familial cold autoinflammatory syndrome
- FMF:
-
Familial Mediterranean fever
- HIDS:
-
Hyperimmunoglobulin D syndrome
- IL:
-
Interleukin
- IL-1Ra:
-
Interleukin-1 receptor antagonist
- mg:
-
Milligram
- MWS:
-
Muckle-Wells syndrome
- NLRP3:
-
Nucleotide-binding oligomerization domain, leucine-rich repeat and pyrin domain containing protein 3
- NOMID:
-
Neonatal-onset multisystem inflammatory disease
- PAPA:
-
Pyogenic arthritis, pyoderma gangrenosum and acne
- PASH:
-
Pyoderma gangrenosum, acne suppurative hidradenitis
- PEST:
-
(proline-, glutamic acid-, serine-, and threonine-rich) family of protein tyrosine phosphatases
- PGA:
-
Pediatric granulomatous arthritis
- PG:
-
Pyoderma gangrenosum
- PRAAS:
-
Proteasome associated autoinflammatory syndromes
- PSTIP1:
-
Proline-serine-threonine phosphatase-interacting protein-1
- TMS1:
-
Target of methylation-induced silencing-1 (identical to ASC)
- TNF-α:
-
Tumor necrosis factor alpha
- TRAPS:
-
Tumor necrosis factor receptor associated periodic syndrome
- TRECID:
-
Tumor necrosis factor-related chronic inflammatory diseases
References
Brunsting LA, Goeckerman WH, O’Leary PA. Pyoderma [ecthyma] gangrenosum: Clinical and experimental observations in five cases occurring in adults. Arch Dermatol Syph. 1930;22:655–80.
Tchernev G, Trebing D, Göring H-D, Steinhoff M, Zouboulis CC, Orfanos C. Pyoderma gangrenosum in Crohn’s disease—the role of immunologic parameters and histological data in diagnosis and differential diagnosis. Bulg J Hepatogastroenterol. 2005;7:56–60.
Wollina U. Clinical management of pyoderma gangrenosum. Am J Clin Dermatol. 2002;3:149–58.
Dinarello CA, van der Meer JW. Treating inflammation by blocking interleukin-1 in humans. Semin Immunol. 2013;25:469–84. doi: 10.1016/j.smim.2013.10.008.
Lipsker D, Lenormand C. Indications and modes of use for interleukin (IL)-1 antagonists in inflammatory dermatosis: a new therapeutic approach to immune-mediated inflammatory diseases. Ann Dermatol Venereol. 2012;139:459–67.
Kowalzick L, Bertolini J, Baumann C, Walther B, Truhm B, Eickenscheidt L. Paradoxical reaction to etanercept: development of pyoderma gangraenosum during therapy of psoriasis arthritis. J Dtsch Dermatol Ges. 2013;11:447–9.
Kikuchi N, Hiraiwa T, Ohashi T, Hanami Y, Satoh M, Takenoshita H, et al. Pyoderma gangrenosum possibly triggered by adalimumab. Eur J Dermatol. 2012;22:804–5.
Stichenwirth M, Riedl E, Pehamberger H, Tappeiner G. Pyoderma gangrenosum in a patient with seronegative rheumatoid arthritis during therapy with adalimumab: toxic effects of adalimumab or failure of adalimumab to prevent the onset of this phenomenon? Arch Dermatol. 2008;144:817–8.
Kleinpenning MM, Langewouters AM, Van De Kerkhof PC, Greebe RJ. Severe pyoderma gangrenosum unresponsive to etanercept and adalimumab. J Dermatolog Treat. 2011;22:261–5.
Wollina U. Pyoderma gangrenosum—a review. Orphanet J Rare Dis. 2007;2:19.
Powell FC, Su WP, Perry HO. Pyoderma gangrenosum: classification and management. J Am Acad Dermatol. 1996;34:395–409.
Farhi D, Cosnes J, Zizi N, Chosidow O, Seksik P, Beaugerie L, et al. Significance of erythema nodosum and pyoderma gangrenosum in inflammatory bowel diseases: a cohort study of 2,402 patients. Medicine (Baltimore). 2008;87:281–93.
Vavricka SR, Brun L, Ballabeni P, Pittet V, Prinz Vavricka BM, Zeitz J, et al. Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol. 2011;106:110–9.
Langan SM, Groves RW, Card TR, Gulliford MC. Incidence, mortality, and disease associations of pyoderma gangrenosum in the United Kingdom: a retrospective cohort study. J Invest Dermatol. 2012;132:2166–70.
Graham JA, Hansen KK, Rabinowitz LG, Esterly NB. Pyoderma gangrenosum in infants and children. Pediatr Dermatol. 1994;11:10–7.
Callen JP. Pyoderma gangrenosum and related disorders. Adv Dermatol. 1989;4:51–69.
Wolff K, Stingl G. Pyoderma gangrenosum. In: Freedberg IM, Eisen AZ, Wolff K, Austen FK, Goldsmith LA, Katz SI, et al., editors. Dermatology in general medicine. New York: McGraw Hill; 1999. pp. 1140–8.
Powell FC, Schroeter AL, Perry HO, Su WP. Direct immunofluorescence in pyoderma gangrenosum. Br J Dermatol. 1983;108:287–93.
Shaya S, Kindzelskii AL, Minor J, Moore EC, Todd RF 3rd, Petty HR. Aberrant integrin [CR4; αxβ2; CD11c/CD18] oscillation on neutrophils in a mild form of pyoderma gangrenosum. J Invest Dermatol. 1998;111:154–8.
Adachi Y, Kindzelskii AL, Cookingham G, Shaya S, Moore EC, Todd RF 3rd. Aberrant neutrophil trafficking and metabolic oscillations in severe pyoderma gangrenosum. J Invest Dermatol. 1998;111:259–68.
Sams HH, Mitchell MM, Stratton CW, King LE Jr. Culture and immunohistochemical evidence of chlamydia infection in ulcerative pyoderma gangrenosum. J Am Acad Dermatol. 2003;48:966–9.
Braun-Falco M, Ruzicka T. Skin manifestations in autoinflammatory syndromes. J Dtsch Dermatol Ges. 2011;9:232–46.
Lamprecht P, Gross WL. Autoinflammatory syndromes. Internist (Berl). 2009;50:676–84.
Contassot E, Beer HD, French LE. Interleukin-1, inflammasomes, autoinflammation and the skin. Swiss Med Wkly. 2012;142:w13590.
Almeida de jA, Goldbach-Mansky R. Monogenic autoinflammatory diseases: concept and clinical manifestations. Clin Immunol. 2013;147:155–74.
Wollina U, Haroske G. Pyoderma gangraenosum. Curr Opin Rheumatol. 2011;23:50–6.
Nesterovitch AB, Hoffman MD, Simon M, Petukhov PA, Tharp MD, Glant TT. Mutations in the PSTPIP1 gene and aberrant splicing variants in patients with pyoderma gangrenosum. Clin Exp Dermatol. 2011;36:889–95.
Shoham NG, Centola M, Mansfield E, Hull KM, Wood G, Wise CA, et al. Pyrin binds the PSTPIP1/CD2BP1 protein, defining familial Mediterranean fever and PAPA syndrome as disorders in the same pathway. Proc Natl Acad Sci U S A. 2003;100:13501–6.
Hara H, Tsuchiya K, Kawamura I, Fang R, Hernandez-Cuellar E, Shen Y, et al. Phosphorylation of the adaptor ASC acts as a molecular switch that controls the formation of speck-like aggregates and inflammasome activity. Nat Immunol. 2013;14:1247–55.
Salminen A, Kauppinen A, Hiltunen M, Kaarniranta K. Epigenetic regulation of ASC/TMS1 expression: potential role in apoptosis and inflammasome function. Cell Mol Life Sci. 2014;71:1855–64.
Müller-Ladner U, Alten R, Heiligenhaus A, Kekow J, Koletzko S, Mrowietz U, et al. “TRECID”, TNFalpha related chronic inflammatory diseases—a new multiple diseases bridging concept. Dtsch Med Wochenschr. 2009;134:2132–6.
Fellermann K. Adverse events of tumor necrosis factor inhibitors. Dig Dis. 2013;31:374–8.
Wollina U, Hansel G, Koch A, Schönlebe J, Köstler E, Haroske G. Tumor necrosis factor-alpha inhibitor-induced psoriasis or psoriasiform exanthemata: first 120 cases from the literature including a series of six new patients. Am J Clin Dermatol. 2008;9:1–14.
Schadt CR, Callen JP. Management of neutrophilic dermatoses. Dermatol Ther. 2012;25:158–72.
Al Ghazal PH, Herberger K, Schaller J, Strölin A, Hoff NP, Goerge T, et al. Associated factors and comorbidities in patients with pyoderma gangrenosum in Germany: a retrospective multicentric analysis in 259 patients. Orphanet J Rare Dis. 2013;8:136.
Powell F, Schroeter A, Su W, Perry H. Pyoderma gangrenosum: a review of 86 patients. Q J Med. 1985;55:173–86.
Seitz CS, Berens N, Bröcker EB, Trautmann A. Leg ulceration in rheumatoid arthritis—an underreported multicausal complication with considerable morbidity: analysis of thirty-six patients and review of the literature. Dermatology. 2010;220:268–73.
Hasegawa M, Nagai Y, Sogabe Y, Hattori T, Inoue C, Okada E, et al. Clinical analysis of leg ulcers and gangrene in rheumatoid arthritis. J Dermatol. 2013;40:949–54.
Chia HY, Tang MB. Chronic leg ulcers in adult patients with rheumatological diseases—a 7-year retrospective review. Int Wound J. 2012;doi: 10.1111/iwj.12012. [Epub ahead of print]
Wollina U, Hein G. Lupus erythematosus: uncommon presentations. Clin Dermatol. 2005;23:470–9.
Reddy V, Dziadzio M, Hamdulay S, Boyce S, Prasad N, Keat A. Lupus and leg ulcers–a diagnostic quandary. Clin Rheumatol. 2007;26:1173–5.
Feld J, Bergman R, Weltfriend S, Zisman D. Pyoderma gangrenosum in a patient with systemic sclerosis. J Rheumatol. 2012;39:197.
Fujikura M, Ohtsuka T, Oyamada Y. Systemic sclerosis in association with peristomal pyoderma gangrenosum. Br J Dermatol. 2007;157:618–9.
Shah M, Lewis FM, Harrington CI. Scrotal pyoderma gangrenosum associated with dermatomyositis. Clin Exp Dermatol. 1996;21:151–3.
Zycinska K, Wardyn K, Zielonka TM, Nitsch-Osuch A, Smolarczyk R. Cutaneous changes: an initial manifestation of pulmonary Wegener’s granulomatosis. Adv Exp Med Biol. 2013;755:307–10.
Halac U, Al Dhaybi R, Powell J, Bouron-Dal Soglio D, Alvarez F. Unusual association between autoimmune hepatitis and severe pyoderma gangrenosum. J Pediatr Gastroenterol Nutr. 2010;50:219–21.
Chandrasekhara PK, Jayachandran NV, Thomas J, Agrawal S, Narsimulu G. Successful treatment of pyoderma gangrenosum associated with juvenile idiopathic arthritis with a combination of topical tacrolimus and oral prednisolone. Clin Rheumatol. 2009;28:489–90.
Ravic-Nikolic A, Milicic V, Ristic G, Jovovic-Dagovic B. Pyoderma gangrenosum associated with Sjögren syndrome. Eur J Dermatol. 2009;19:392–3.
Richetta AG, D’Epiro S, Mattozzi C, Giancristoforo S, Calvieri S. Folgoration as an example of pathergy in a patient affected by pyoderma gangrenosum and Takayasu’s arteritis. Dermatol Res Pract. 2009;2009:393452.
Dejardin Botelho A, Delesalle F, Delaporte E, Wallaert B. Pyoderma gangrenosum and Churg-Strauss syndrome. Rev Med Interne. 2007;28:564–5.
Mehta AJ, Charman CR. Pyoderma gangrenosum in association with autoimmune neutropenia of infancy. Pediatr Dermatol. 2008;25:620–2.
Coors EA, von den Driesch P. Pyoderma gangrenosum in a patient with autoimmune haemolytic anaemia and complement deficiency. Br J Dermatol. 2000;143:154–6.
Necas M, Semrádova V, Vaskù V. Pyoderma gangraenosum associated with autoimmune thyreopathy and hyperandrogenic syndrome. Acta Dermatovenerol Alp Panonica Adriat. 2005;14:57–60.
Livideanu C, Lipsker D, Paul C, Juillard J, Schubert B. Pyoderma gangrenosum as initial manifestation of Graves’ disease. Clin Exp Dermatol. 2006;31:659–61.
Matis WL, Ellis CN, Griffiths CEM, Lazarus GS. Treatment of pyoderma gangrenosum with cyclosporin. Arch Dermatol. 1992;128:1060–4.
O’Donnell B, Powell FC. Cyclosporin treatment of pyoderma gangrenosum. J Am Acad Dermatol. 1991;24:141–3.
Zumdick M, Goerz G, Schuppe HC, Milde P, Ruzicka T. Niedrig dosierte Cyclosporin-A-Therapie bei Pyoderma gangraenosum. Erfahrungen bei 6 Patienten. Hautarzt. 1995;46:697–701.
Van den Driesch P. Pyoderma gangrenosum: a report of 44 cases with follow-up. Br J Dermatol. 1997;137:1000–5.
Prystowsky JH, Kahn SN, Lazarus GS. Present status of pyoderma gangrenosum. Arch Dermatol. 1989;125:57–64.
Arbiser JL, Moschella SL. Clofazimine: a review of its medical uses and mechanisms of action. J Am Acad Dermatol. 1995;32:241–7.
Peuckmann V, Fisch M, Bruera E. Potential novel uses of thalidomide: focus on palliative care. Drugs. 2000;60:273–92.
Wollina U, Karamfilov T. Treatment of recalcitrant ulcers in pyoderma gangrenosum with mycophenolate mofetil and autologous keratinocyte transplantation on a hyaluronic acid matrix. J Eur Acad Dermatol Venereol. 2000;14:187–90.
Daniels NH, Callen JP. Mycophenolate mofetil is an effective treatment for peristomal pyoderma gangrenosum. Arch Dermatol. 2004;140:1427–9.
Lee MR, Cooper AJ. Mycophenolate mofetil in pyoderma ganrenosum. J Dermatolog Treat. 2004;15:303–7.
Baumgart DC, Wiedenmann B, Dignass AU. Successful therapy of refractory pyoderma gangrenosum and periorbital phlegmona with tacrolimus [FK506] in ulcerative colitis. Inflamm Bowel Dis. 2004;10:421–4.
Kontochristopoulos GJ, Stavropoulos PG, Gregoriou S, Zakopoulou N. Treatment of pyoderma gangrenosum with low-dose colchicine. Dermatology. 2004;209:233–6.
Schmidt C, Wittig BM, Moser C, Zeitz M, Stallmach A. Cyclophosphamide pulse therapy followed by azathioprine or methotrexate induces long-term remission in patients with steroid-refractory Crohn’s disease. Aliment Pharmacol Ther. 2006;24:343–50.
Budde K, Glander P, Diekmann F, Waiser J, Fritsche L, Dragun D, et al. Review of the immunosuppressant enteric-coated mycophenolate sodium. Expert Opin Pharmacother. 2004;5:1333–45.
Fujimoto E, Fujimoto N, Kuroda K, Tajima S. Leukocytapheresis treatment for pyoderma gangrenosum. Br J Dermatol. 2004;151:1090–2.
Mori S, Nagashima M, Yoshida K, Yoshino K, Aoki M, Kawana S, et al. Granulocyte adsorptive apheresis for leg ulcers complicated by rheumatoid arthritis: a report on three successfully treated cases. Int J Dermatol. 2004;43:732–5.
Girolomoni G, Pastore S, Albanesi C, Cavani A. Targeting tumor necrosis factor-alpha as a potential therapy in inflammatory skin diseases. Curr Opin Investig Drugs. 2002;3:1590–5.
Mimouni D, Anhalt GJ, Kouba DJ, Nousari HC. Infliximab for peristomal pyoderma gangrenosum. Br J Dermatol. 2003;148:813–6.
Sapienza MS, Cohen S, Dimarino AJ. Treatment of pyoderma gangrenosum with infliximab in Crohn’s disease. Dig Dis Sci. 2004;49:1454–7.
Kaufman I, Caspi D, Yeshurun D, Dotan I, Yaron M, Elkayam O. The effect of infliximab on extraintestinal manifestations of Crohn’s disease. Rheumatol Int. 2005;25:406–10.
Roy DB, Conte ET, Cohen DJ. The treatment of pyoderma gangrenosum using etanercept. J Am Acad Dermatol. 2006;54(Suppl 2):128–34.
Hinterberger L, Müller CS, Vogt T, Pföhler C. Adalimumab: a treatment option for pyoderma gangrenosum after failure of systemic standard therapies. Dermatol Ther (Heidelb). 2012;2(1):6.
Sims JE, Smith DE. The IL-1 family: regulators of immunity. Nat Rev Immunol. 2010;10:89–102.
Steiger S, Harper JL. Mechanisms of spontaneous resolution of acute gouty inflammation. Curr Rheumatol Rep. 2014;16:392.
Tavares AH, Magalhães KG, Almeida RD, Correa R, Burgel PH, Bocca AL. NLRP3 Inflammasome activation by Paracoccidioides brasiliensis. PLoS Negl Trop Dis. 2013;7:e2595.
Garlanda C, Dinarello CA, Mantovani A. The interleukin-1 family: back to the future. Immunity. 2013;39:1003–18.
Cunha LD, Zamboni DS. Subversion of inflammasome activation and pyroptosis by pathogenic bacteria. Front Cell Infect Microbiol. 2013;3:76.
Mao L, Zhang L, Li H, Chen W, Wang H, Wu S, et al. Pathogenic fungus Microsporum canis activates the NLRP3 inflammasome. Infect Immun. 2014;82:882–92.
Miao EA, Leaf IA, Treuting PM, Mao DP, Dors M, Sarkar A, et al. Caspase-1-induced pyroptosis is an innate immune effector mechanism against intracellular bacteria. Nat Immunol. 2010;11:1136–42.
Brenner M, Ruzicka T, Plewig G, Thomas P, Herzer P. Targeted treatment of pyoderma gangrenosum in PAPA (pyogenic arthritis, pyoderma gangrenosum and acne) syndrome with the recombinant human interleukin-1 receptor antagonist anakinra. Br J Dermatol. 2009;161:1199–201.
Braun-Falco M, Kovnerystyy O, Lohse P, Ruzicka T. Pyoderma gangrenosum, acne, and suppurative hidradenitis (PASH)–a new autoinflammatory syndrome distinct from PAPA syndrome. J Am Acad Dermatol. 2012;66:409–15.
Baumgart DC, Wiedenmann B, Dignass AU. Successful therapy of refractory pyoderma gangrenosum and periorbital phlegmona with tacrolimus [FK506] in ulcerative colitis. Inflamm Bowel Dis. 2004;10:421–4.
Khurrum Baig M, Marquez H, Nogueras JJ, Weiss EG, Wexner SD. Topical tracrolimus [FK506] in the treatment of recalcitrant parastomal pyoderma gangrenosum associated with Crohn’s disease: report of two cases. Colorectal Dis. 2004;6:250–3.
Wollina U. Letter to the editor: Temporary renal insufficiency associated with topical tacrolimus treatment of multilocal pyoderma gangrenosum. J Dermatol Case Rep. 2013;7:106–7.
Neiderer K, Martin B, Hoffman S, Jolley D, Dancho J. A mechanically powered negative pressure device used in conjunction with a bioengineered cell-based product for the treatment of pyoderma gangrenosum: a case report. Ostomy Wound Manage. 2012;58:44–8.
Hill DS, O’Neill JK, Toms A, Watts AM. Pyoderma gangrenosum: a report of a rare complication after knee arthroplasty requiring muscle flap cover supplemented by negative pressure therapy and hyperbaric oxygen. J Plast Reconstr Aesthet Surg. 2011;64:1528–32.
Ghersi MM, Ricotti C, Nousari CH, Newman MI. Negative pressure dressing in the management of pyoderma gangrenosum ulcer. Arch Dermatol. 2007;143:1249–51.
Mir-Bonafé JM, Blanco-Barrios S, Romo-Melgar A, Santos-Briz A, Fernández-López E. Photoletter to the editor: Localized pyoderma gangrenosum after interferon-alpha2b injections. J Dermatol Case Rep. 2012;6:98–9.
ten Freyhaus K, Homey B, Bieber T, Wilsmann-Theis D. Pyoderma gangrenosum: another cutaneous side-effect of sunitinib? Br J Dermatol. 2008;159:242–3.
Nadauld LD, Miller MB, Srinivas S. Pyoderma gangrenosum with the use of sunitinib. J Clin Oncol. 2011;29:e266–7.
Sagara R, Kitami A, Nakada T, Iijima M. Adverse reactions to gefitinib (Iressa): revealing sycosis- and pyoderma gangrenosum-like lesions. Int J Dermatol. 2006;45:1002–3.
Bustillo I, Kaley K, Saif MW. Rash associated with the use of pegylated filgrastim in a patient with advanced pancreatic cancer. Cutan Ocul Toxicol. 2009;28:181–4.
Tinoco MP, Tamler C, Maciel G, Soares D, Avelleira JC, Azulay D. Pyoderma gangrenosum following isotretinoin therapy for acne nodulocystic. Int J Dermatol. 2008;47:953–6.
Freiman A, Brassard A. Pyoderma gangrenosum associated with isotretinoin therapy. J Am Acad Dermatol. 2006;55:107–8.
Hong SB, Lee MH. A case of propylthiouracil-induced pyoderma gangrenosum associated with antineutrophil cytoplasmic antibody. Dermatology. 2004;208:339–41.
Srebrnik A, Shachar E, Brenner S. Suspected induction of a pyoderma gangrenosum-like eruption due to sulpiride treatment. Cutis. 2001;67:253–6.
Conflict of interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wollina, U., Tchernev, G. Pyoderma gangrenosum: pathogenetic oriented treatment approaches. Wien Med Wochenschr 164, 263–273 (2014). https://doi.org/10.1007/s10354-014-0285-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-014-0285-x