Abstract
Background
The TRICC0808 trial is a phase II multi-institutional trial that investigated the efficacy of preoperative mFOLFOX6 + bevacizumab (BV) therapy for liver-only metastasis that is unsuitable for upfront resection. The R0 resection rate in the efficacy analysis has been reported to be 44.4%, and the final analysis for survival was conducted (data fixation on February 16, 2015).
Methods
Six cycles of mFOLFOX6 + BV therapy were applied to patients with liver-only metastases, which were > 5 cm in diameter or more than four tumors (H2 and H3), and hepatectomy was performed if possible. Primary and secondary endpoints were the R0 hepatectomy rate and overall survival (OS), respectively.
Results
Of 46 patients registered, OS was analyzed for 45 patients in whom the 3-year OS rate from the starting date of chemotherapy was 44.0% with a 33.6-month median survival time (MST). The 3-year OS rate of 31 patients with hepatectomy, including resection after an additional chemotherapy, was 61.3% with a 43.1-month MST, which was significantly better than 0% of the 3-year OS rate with a 21.0-month MST of 14 patients without hepatectomy (p value < 0.0001). In 24 patients who underwent hepatectomy after six cycles of protocol chemotherapy, the 3-year relapse-free survival rate was 8.3%, with a 36.8-month MST.
Conclusions
This final analysis of the TRICC0808 trial revealed a better long-term survival in patients with hepatectomy after mFOLFOX6 + BV therapy, although most examined patients eventually developed recurrence. Thus, hepatectomy after chemotherapy might improve the survival in patients with advanced liver metastases, although cure remains difficult.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The liver is a frequent site of metastases from colorectal cancer [1,2,3], and hepatectomy is the only curative treatment, with a 5-year survival rate of 40–60% [3,4,5,6,7]. However, only a minority of patients with liver metastases are initially eligible for radical hepatectomy [8]. Reportedly, the initial resection rate is reported to be < 25% because of the higher number and size and the complicated location of tumor [9, 10]. In patients with multiple or large liver metastases, liver tumors might not be completely resected or recurrence even after R0 hepatectomy is frequently observed. In addition, chemotherapies with new potent cytotoxic drugs, such as irinotecan and oxaliplatin [11], and molecule-targeted drugs [12,13,14,15,16] have improved the response rate for metastatic colorectal cancer. In the treatment of patients with unresectable liver metastases, conversion therapy has been applied to decrease the tumor size and facilitate resection via preoperative chemotherapy with new potent drugs [17,18,19].
Thus, we conducted a phase II multi-institutional clinical study—TRICC0808—to investigate the efficacy and safety of preoperative modified oxaliplatin-infused 5-fluorouracil leucovorin (mFOLFOX6) + bevacizumab (BV) therapy in patients with colorectal cancer and liver-only metastases in whom upfront surgery was unsuitable (maximum metastatic focal diameter, > 5 cm or number of metastases, ≥ 5; H2/H3) [20, 21]. Previously, we reported that mFOLFOX6 + BV yielded R0 hepatectomy rate of 44.4% and conversion rate of 23.1%, whereas the rate of surgical complications was low. This study presented the final survival data analysis of TRICC0808 after the 3-year follow-up from the start date of mFOLFOX6 + BV therapy (final data fixation was on February 16, 2015).
Patients and methods
Study design
TRICC0808 was a multicenter, phase II clinical study; details of the trial design and study procedures are available elsewhere [21]. The primary trial endpoint was the R0 hepatectomy rate for the entire study population, and secondary endpoints were the R0 hepatectomy rate relative to all resected cases, the percentage of initially resectable and subsequently unresectable cases, the percentage of initially unresectable and subsequently resectable cases, hepatectomy safety, recurrence rate, and survival period. The primary endpoint and treatment results of chemotherapy are provided elsewhere [21].
Patients
Patients eligible for this study were as follows: those aged 20–80 years; those with an Eastern Cooperative Oncology Group Performance Status (ECOG PS) of 0–1; those with histologically proven colorectal cancer; those with maximum liver metastatic focal diameter of > 5 cm or with more than five liver metastases (H2/H3); those who underwent curative primary tumor resection ≥ 28 days before registration; those with no detectable extrahepatic metastases; those with no history of chemotherapy. This study protocol was approved by the medical ethics committees of all participating facilities, and written informed consent was obtained from all patients before registration.
Procedures
Within 2 weeks of registration, each registered patient received the first mFOLFOX6 + BV therapy. After three treatment cycles, the first diagnostic imaging evaluation was performed. For patients in whom the diagnostic imaging evaluation was progressive disease (PD) or stable disease (SD), tumor growth might make resection impossible; therefore, in such patients, hepatectomy was performed if feasible or the protocol treatment was discontinued. In patients rated as complete response (CR), partial response (PR), or SD, mFOLFOX6 + BV therapy was administered for three additional cycles (during the sixth cycle, only mFOLFOX6 was administered). After six cycles, the second diagnostic imaging evaluation was performed. If deemed resectable, then hepatectomy was performed, whereas if deemed unresectable, then the protocol treatment was immediately discontinued.
R0 hepatectomy was defined by the absence of microscopic tumor invasion of the resection margins, R1 hepatectomy was defined by the presence of microscopic tumor invasion at the resection margins, and R2 hepatectomy was defined by the presence of macroscopic residual tumor [20]. Patients who underwent thermal coagulation therapy, radiofrequency ablation (RFA), or microwave coagulation therapy were considered for R2 hepatectomy. In addition, patients who underwent R1 or R2 hepatectomy were treated further at physicians’ discretion. Postoperative adjuvant chemotherapy was not routinely administered after R0 hepatectomy.
The pathological response of chemotherapy was evaluated in resected specimens based on the JSCCR criteria [20]. Patients were followed up every 6 months with contrast-enhanced computed tomography (CT) and the measurement of serum CEA level. Overall survival (OS) was defined as the time interval between the starting date of chemotherapy and the date of death. Furthermore, patients who underwent hepatectomy were assessed for relapse-free survival (RFS) and OS at 1-, 2-, and 3-year postoperatively by clinical examinations, including tumor markers, and contrast-enhanced CT.
Statistical analysis
The sample size calculation and null and alternative hypotheses about the primary endpoint have been reported previously [21]. OS and RFS rates were estimated using the Kaplan–Meier method and compared by the log-rank test. Groups were compared with the use of Fisher’s exact test or the Chi-square test for categorical variables and the Wilcoxon signed-rank test for continuous variables. In this study, statistical analyses were conducted using SAS version 9.3 (SAS Institute Inc., Cary, NC), and statistical significance was set at the 0.05 level.
Results
From April 2009 to October 2011, 46 patients from 25 institutes were enrolled. However, one patient was found ineligible after commencing the treatment. The median follow-up period after the start of protocol chemotherapy was 31.4 (range 10.1–63.7) months.
Patients’ characteristics
All eligible patients underwent curative primary tumor resection ≥ 28 days before registration. The median number of liver metastases was 6 (range 1–23). The reason for being unresectable was the inadequate volume of the remnant liver in most patients (88.5%) and poor anatomical localization of tumor in a few patients (7.7%) (Supplemental Table 1).
Protocol chemotherapy and hepatectomy
Forty-one patients completed the planned six cycles of protocol chemotherapy (chemotherapy completion rate, 91.1%) (Supplemental Fig. 1). Hepatectomy was performed after six cycles of the protocol treatment in 24 (53.3%) patients, with R0 hepatectomy in 20 and R1/R2 hepatectomy in four (including three patients judged as R2 for the additional RFA). Most surgical procedures were major hepatectomy (54.1%) that were hepatic resection of three or more adjacent Couinaud segments. Of 19 patients with initially resectable liver metastases, 18 (94.7%) underwent hepatectomy (R0, 16; R1/R2, 2). Of 26 initially unresectable patients, six (23.1%) underwent hepatectomy after the protocol treatment (R0, 4; R1/R2, 2), and therefore, the conversion rate was 23.1%. No surgery-related deaths or any second surgery owing to complications was required in this study population.
Chemotherapies after hepatectomy were performed in 10 (42%) of 24 patients (FOLFOX, 2; mFOLFOX6 + BV, 2; mFOLFOX6, 5; CapeOX, 1; uracil + tegafur/leucovorin, 1).
Chemotherapy after post-protocol treatment and hepatectomy
Post-protocol chemotherapies were performed in 18 unresectable patients [mFOLFOX6/capecitabine + oxaliplatin (CapeOX) ± BV, 15; folinic acid, fluorourcil, and irinotecan (FOLFIRI) ± BV/cetuximab, 8; irinotecan + S-1 (IRIS) ± BV, 2; simplified biweekly leucovorin and fluorouracil (sLV5FU2) + BV, 1; hepatic arterial infusion (HAI), 1]. Of these, seven patients underwent hepatectomy. Regimens of post-protocol chemotherapy in patients undergoing hepatectomy were four cycles of mFOLFOX6 + BV plus seven cycles of FOLFIRI + panitumumab, three cycles of mFOLFOX6 + BV, six cycles of mFOLFOX6 + BV, one cycle of mFOLFOX6 + BV plus four cycles of FOLFIRI + BV, one cycle of FOLFIRI, six cycles of mFOLFOX6 + BV plus 3 years of sLV5FU2 + BV, six cycles of mFOLFOX6 + BV, and 22 cycles of IRIS/IRIS + S-1 plus FOLFIRI + BV.
Survival
The 1-, 2-, and 3-year OS rates in 45 eligible patients were 91.1% (95% CI 78.0–96.0%), 68.9% (95% CI 53.2–80.2%), and 44.0% (95% CI 29.2–57.8%), respectively, with 33.6 (95% CI 24.7–43.1) months of the MST (Fig. 1a). The 3-year OS rate in 31 patients with hepatectomy, including seven who underwent surgery after additional chemotherapy, was 61.3% (95% CI 42.0–75.8%), with the 43.1-month MST (95% CI 33.6–not reached), which was better than 0% of the 3-year OS rate with the 21.0-month MST (95% CI 11.9–27.0 months) in patients without hepatectomy (p value < 0.0001; Fig. 1b). No differences were observed in the survival time between 24 patients with hepatectomy after six cycles of protocol chemotherapy and seven patients with hepatectomy after an additional chemotherapy (p value = 0.2947; Fig. 1c).
Overall survival from start of mFOLFOX6 + BV therapy. a All eligible patients (N = 45). b Patients with hepatectomy including surgery after post-protocol chemotherapy (solid line, N = 31), Patients without hepatectomy (dashed line, N = 14). c Patients with hepatectomy after protocol 6 cycles mFOLFOX 6 + BV (solid line, N = 24); patients with hepatectomy after post-protocol additional chemotherapy (dashed line, N = 7)
In 24 patients with hepatectomy after six cycles of protocol chemotherapy, the 1-, 2-, and 3-year OS rates were 87.5% (95% CI 66.1–95.5%), 70.8% (95% CI 48.4–84.9%), and 53.0% (95% CI 31.2–70.8%), respectively, with the 36.8-month MST (95% CI 23.5–not reached), and the 1-, 2-, and 3-year RFS rates were 29.2% (95% CI 13.0–47.6%), 12.5% (95% CI 3.1–28.7%), and 8.3% (95% CI 1.4–23.3%), respectively, with the 5.9 months of median RFS (95% CI 4.1–10.2 months; Fig. 2). MST and median RFS in 20 patients with R0 hepatectomy were 39.2 (95% CI 23.5–not reached) and 6.2 months (95% CI 4.1–15.2 months), respectively. Among patients with R0 hepatectomy, the 3-year OS rates of 16 patients with resectable liver metastases at registration and four with unresectable liver metastases at registration were similar.
Tables 1 and 2 present clinicopathological factors and survival of eligible patients and 24 patients with hepatectomy after six cycles of protocol chemotherapy. In all eligible patients, the objective response to chemotherapy and presence of hepatectomy exhibited a markedly better OS, whereas T4a/T4b primary tumors exhibited a worse prognosis. In the 24 patients with hepatectomy, the survival period was not considerably different among the degrees of pathological response.
Recurrence
Recurrence was observed in 16 (80%) of 20 patients with R0 hepatectomy. All of four patients with R1/R2 hepatectomy developed remnant liver limited recurrence early after surgery. The median RFS after hepatectomy was 5.3 months. In addition, 14 (58.3%) patients developed recurrence in the liver, including 11 (45.8%) with liver-only diseases and 3 (12.5%) with liver diseases plus lung metastases (Table 3). Furthermore, surgeries for recurrent diseases were undergone in eight (40%) of 20 patients with recurrence, including five (45.5%) of 11 patients with liver-only recurrence and three (100%) of three patients with lung-only recurrence (Table 3).
Discussion
Several studies have investigated combination therapy with surgery and preoperative chemotherapy for resectable metastases to improve the R0 rate and for unresectable metastases to convert to a resectable status (conversion). However, several of these studies were retrospective or subgroup analysis in randomized trials, and randomized, controlled studies designed to assess conversion chemotherapy were limited [17,18,19, 22,23,24,25,26]. Thus, the optimal treatment approach for patients who are unsuitable for upfront resection liver metastases remains unclear.
Previously, the TRICC0808 study illustrated that preoperative mFOLFOX6 + BV therapy attained a high R0 hepatectomy rate (44.4%) and conversion rate (23.1%) for patients with liver metastases who were unsuitable for upfront resection [21]. As the R0 rate was approximately 45% of the anticipated rate, it fulfilled the primary endpoint. In addition, compared with the previous studies for patients who were unsuitable for upfront resection, the R0 and conversion rates in this study were encouraging [17,18,19, 23, 24]. This final survival analysis of TRIC0808 demonstrated that hepatectomy following mFOLFOX6 + BV therapy attained favorably extended survival. Precisely, 24 patients with hepatectomy after protocol chemotherapy attained 36.8 months of MST, and MST in all 31 patients who underwent hepatectomy, including seven patients after an additional chemotherapy, was 43.1 months, although most patients had surgical difficulties and poor prognostic factors [27]. However, disease recurrence occurred early after the surgery, with 5.3 months of median RFS, in patients with hepatectomy after protocol therapy.
We evaluated the associations of clinicopathological factors with OS (Tables 2, 1). The size and number were not prognostic factors, since most patients had numerous (median number, 6) and large (median size, 5.3 cm) hepatic metastases.
Patients with T4a/T4b primary tumor exhibited worse prognosis, although hepatectomy rate was similar to that of patients with T1/T2/T3 tumor. Patients with T4a/T4b developed only remnant liver limited recurrence.
In this trial, 68.9% of patients had colon cancer. Patients with colon cancer had a lower hepatectomy rate and worse OS compared with rectosigmoid/rectum cases (no statistical difference). Recently, primary tumor location (sidedness) has been reported to be a critical prognostic factor in metastatic colorectal cancer [28]. Regrettably, we did not collect information on sidedness of colon cancer; therefore, we were unable to do subset analysis for sidedness.
Previously, the pathological response to preoperative chemotherapy in liver metastases has been reported to correlate with a favorable survival outcome [18, 29]. However, in this study, the pathological response exhibited no marked impact on the survival, which may have been because of the small number of examined patients.
The CELIM study was a well-planned, prospective study investigating the efficacy of preoperative chemotherapy (FOLFOX or FOLFIRI plus cetuximab) for patients who were unsuitable for upfront resection liver metastases, which were defined as technically unresectable and/or more than five liver tumors [19, 30]. Although the entry criteria and definition of resectability were similar to our study, it slightly differed, which necessitated cautious and direct comparison. A similar number of patients recruited for hepatectomy (R0 rate; TRICC0808 44% vs. CELIM 34%) and a similar number of initially technically unresectable patients proceeded to hepatectomy (conversion rate; TRICC0808 23% vs. CELIM 28%). Regarding the survival, MST in all eligible patients was similar in both studies (TRICC0808 study, 33.6 months; CELIM study, 35.7 months). In contrast, for patients who underwent R0 hepatectomy, the MST of 39.2 months in this study is worse than 53.9 months reported in the CELIM study [30]. In both studies, disease recurrences occurred early after surgery in most patients; however, 6.2 months of the median RFS in this study was worse than 9.9 months in the CELIM study. A significant portion of patients enrolled in this study had unfavorable prognostic factors [27]; that is, 34% of our patients who underwent hepatectomy had massive disease infiltration (H3; ≤ 5 lesions and > 5 cm liver metastases) and 83% of patients had a synchronous metastatic tumor. Despite the limits of comparing the results of different studies, our survival results seem encouraging.
The previous studies have reported that patients with initially unresectable liver metastases, whose metastases were rendered resectable after chemotherapy and underwent hepatectomy, exhibited a high recurrence rate (> 70%) and short median RFS (16–19 months) [4, 31] but better OS [32, 33]. In addition, patients with postoperative recurrence of metastatic disease would likely benefit from an additional surgery or second-line chemotherapy [34], which might explain why patients exhibited a relatively prolonged survival, considering the early recurrences after hepatectomy in our study and in the other studies. However, other studies did not provide details of the recurrence and treatment for recurrent diseases. In this study, among 20 patients who developed recurrence after hepatectomy, eight (40%) underwent radical resection for recurrent tumors and nine (45%) proceeded to the second-line chemotherapy for recurrent diseases (Table 3), which might explain why patients in this study exhibited a relatively prolonged survival, considering the early recurrences after hepatectomy.
In patients who are unsuitable for upfront resection liver metastases, a regimen resulting in high response and large-size reduction is recommended [35]. According to a consensus statement for downsizing, FOLFOX and FOLFIRI are two standard chemotherapy techniques with equivalent efficacy [36]. Regarding biological agents, a recent meta-analysis concluded that the addition of an anti-EGFR antibody to chemotherapy markedly increases the response and R0 hepatectomy rate, whereas the addition of BV exhibits no benefit in tumor regression [13]. Furthermore, cetuximab plus FOLFOX or FOLFIRI has shown to improve both resectability and survival in patients with Kras wild-type liver metastases [25].
The ESMO guideline [37] states that only a few trials specifically designed to investigate “conversion” chemotherapy were randomized, controlled trials, making it difficult to reach any decision regarding the “best” regimen to use in this clinical setting. Seemingly, a combination of cytotoxic doublet and an anti-EGFR antibody has the best benefit risk/ratio in patients with RAS wild-type disease, although the combination of FOLFOXIRI plus BV might also be considered and to a lesser extent, a cytotoxic doublet plus BV.
In patients with an RAS-mutant disease, a cytotoxic doublet plus BV or fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) plus BV is recommended. Tumor RAS status should be determined for every case of metastatic colorectal cancer. However, the Japanese social insurance system did not include RAS mutation testing until 2010 after we started this trial. We, therefore, chose mFOLFOX6 + BV as protocol regimen and did not investigate RAS status.
The combined use of BV with FOLFOX or FOLFIRI is not compelling in the preoperative setting. However, the combined use of BV provides a higher response rate and prolonged survival in patients with both Kras wild-type and mutant [38]. Reportedly, chemotherapeutic agents might cause liver injuries, such as steatohepatitis and sinusoidal congestion, and surgical complications [39]. In contrast, the combined use of BV and oxaliplatin can decrease sinusoidal congestion [40]. In this study, a high radiological response rate (55.6%) and pathological response rate (major response with necrosis of > 1/3 of the tumor; 42.5%) were observed. However, the rate of surgical complication was low. Based on these perspectives, the combined use of BV and oxaliplatin is acceptable for patients who are unsuitable for upfront resection liver metastases, which are not confined to the Kras wild-type population.
In patients with extensive liver involvement, mFOLFOX6 + BV preoperative therapy has proven to be a promising first-line treatment to improve the R0 rate and for conversion. MST of 43.1 months in the patients with hepatectomy is much longer than what could be expected with chemotherapy alone; however, MST of 33.6 months in all eligible patients might not be enough for including 69% of the patients with hepatectomy. Synchronous liver metastases with major liver involvement were usually characterized as having a very poor prognosis [27]. In our study, 87% of patients had a synchronous metastatic tumor and 31% of patients had massive disease infiltration (H3; 5 ≤ lesions and 5 cm < size). Therefore, survival in unresectable patients was very poor, and disease recurrences occurred early after hepatectomy in most patients. The survival benefit of preoperative mFOLFOX6 + BV therapy for patients with very poor prognosis factors might still be controversial.
Conclusion
Preoperative mFOLFOX6 + BV therapy for patients who are unsuitable for upfront resection liver metastases from colorectal cancer could contribute to the better survival outcome by increasing the number of patients undergoing R0 hepatectomy. However, most patients in this study eventually developed recurrence. Regarding the treatment of disease, clinical benefits of preoperative chemotherapy for patients who are unsuitable for upfront resection colorectal liver metastases might still be controversial.
References
Borner MM (1999) Neoadjuvant chemotherapy for unresectable liver metastases of colorectal cancer—too good to be true? Ann Oncol 10:623–626
Fong Y, Cohen AM, Fortner JG et al (1997) Liver resection for colorectal metastases. J Clin Oncol 15:938–946
Kato T, Yasui K, Hirai T et al (2003) Therapeutic results for hepatic metastasis of colorectal cancer with special reference to effectiveness of hepatectomy; analysis of prognostic factors for 763 cases recorded at 18 institutions. Dis Colon Rectum 46:S22–S31
Alberts S, Curley S, Figueras J et al (2005) OncoSurge: a strategy for improving resectability with curative intent in metastatic colorectal cancer. J Clin Oncol 23:7125–7134
Beppu T, Sakamoto Y, Hasegawa K et al (2012) A nomogram predicting disease-free survival in patients with colorectal liver metastases treated with hepatic resection: multicenter data collection as a Project Study for Hepatic Surgery of the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci 19:72–84
Choti MA, Sitzmann JV, Tiburi MF et al (2002) Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 235:759–766
Pawlik TM, Scoggins CR, Zorzi D et al (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241:715–722
Wang X, Hershman DL, Abrams JA et al (2007) Predictors of survival after hepatic resection among patients with colorectal liver metastasis. Br J Cancer 97:1606–1612
Scheele J, Stang R, Altendorf-Hofmann A et al (1995) Resection of colorectal liver metastases. World J Surg 19:59–71
Bismuth H, Adam R, Levi F et al (1996) Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg 224:509–522
Tournigand C, André T, Achille E et al (2004) FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 22:229–237
Hurwitz H, Fehrenbacher L, Novotny W et al (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Saltz LB, Clarke S, Díaz-Rubio E et al (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 26:2013–2019
Van Cutsem E, Köhne CH, Hitre E et al (2009) Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med 360:1408–1417
Bokemeyer C, Bondarenko I, Makhson A et al (2009) Fluorouracil, leucovorin, and oxaliplatin with and without cetuximab in the first-line treatment of metastatic colorectal cancer. J Clin Oncol 27:663–671
Douillard JY, Siena S, Cassidy J et al (2010) Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J Clin Oncol 28:4697–4705
Garufi C, Torsello A, Tumolo S et al (2010) Cetuximab plus chronomodulated irinotecan, 5-fluorouracil, leucovorin and oxaliplatin as neoadjuvant chemotherapy in colorectal liver metastases: POCHER trial. Br J Cancer 103:1542–1547
Adam R, Delvart V, Pascal G et al (2004) Rescue surgery for unresectable colorectal liver metastases down staged by chemotherapy: a model to predict long-term survival. Ann Surg 240(4):644–657
Folprecht G, Gruenberger T, Bechstein WO et al (2010) Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol 11:38–47
Japanese society of cancer of the colon and rectum (2009) Japanese Classification of Colorectal carcinoma. Kanehara-Shuppan, Tokyo
Uetake U, Yasuno M, Ishiguro M et al (2015) A multicenter phase II trial of mFOLFOX6 plus bevacizumab to treat liver-only metastases of colorectal cancer that are unsuitable for upfront resection (TRICC0808). Ann Surg Oncol 22:908–915
Wong R, Cunningham D, Barbachano Y et al (2011) A multicentre study of capecitabine, oxaliplatin plus bevacizumab as perioperative treatment of patients with poor-risk colorectal liver-only metastases not selected for upfront resection. Ann Oncol 22:2042–2048
Bridgewater GJ, Chau I, Alfonso PG et al (2015) Bevacizumab plus mFOLFOX-6 or FOLFOXIRI in patients with initially unresectable liver metastases from colorectal cancer; the OLIVIA multinational randomized phase II trial. Ann Oncol 26:702–708
Ychou M, Rivoire M, Thezenas S et al (2013) A randomized phase II trial of three intensified chemotherapy regimens in first-line treatment of colorectal cancer patients with initially unresectable or not optimally resectable liver metastases. The METHEP trial. Ann Surg Oncol 20:4289–4297
Ye LC, Liu TS, Ren L et al (2013) Randomized controlled trial of cetuximab plus chemotherapy for patients with KRAS wild-type unresectable colorectal liver-limited metastases. J Clin Oncol 31:1931–1938
Oki E, Emi Y, Miyamoto Y et al (2015) Phase II trial of S-1 and oxaliplatin plus cetuximab for colorectal cancer patients with initially unresectable or not optimally resectable liver metastases (KSCC1002). Ann Surg Oncol 22:S1067–S1074
Fong Y, Fortner J, Sun RL et al (1999) Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 230:309–318
Loupakis F, Yang D, Yau L et al (2015) Primary tumor location as a prognostic factor in metastatic colorectal cancer. J Natl Cancer Inst Feb24 107(3):dju427. https://doi.org/10.1093/jnci/dju427
Blazer DG III, Kishi Y, Maru DM et al (2008) Pathologic response to preoperative chemotherapy: a new outcome endpoint after resection of hepatic colorectal metastases. J Clin Oncol 26:5344–5351
Folprecht G, Gruenberger T, Bechstein W et al (2014) Survival of patients with initially unresectable colorectal liver metastases treated with FOLFOX/cetuximab or FOLFIRI/cetuximab in a multidisciplinary concept (CELIM study). Ann Oncol 25:1018–1025
Adam R, Wicherts DA, de Haas RJ et al (2009) Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol 27:1829–1835
Adam R, De Gramont A, Figueras J et al (2012) The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist 17:1225–1239
Nordlinger B, Van Cutsem E, Rougier P et al (2007) Does chemotherapy prior to liver resection increase the potential for cure in patients with metastatic colorectal cancer? A report from the European Colorectal Metastases Treatment Group. Eur J Cancer 43:2037–2045
Kopetz S, Chang GJ, Overman MJ et al (2009) Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol 27:3677–3683
Folprecht G, Grothey A, Alberts S et al (2005) Neoadjuvant treatment of unresectable colorectal liver metastases: correlation between tumour response and resection rates. Ann Oncol 16:1311–1319
Schwarz RE, Berlin JD, Lenz HJ et al (2013) Systemic cytotoxic and biological therapies of colorectal liver metastases: expert consensus statement. HPB (Oxford) 15:106–115
Van Cutsem E, Cervantes A, Adam R et al (2016) ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 27:1386–1422
Hurwits HI, Yi J, Ince W et al (2009) The clinical benefit of bevacizumab in metastatic colorectal cancer is independent of K-ras mutation status: analysis of a phase III study of bevacizumab with chemotherapy in previously untreated metastatic colorectal cancer. Oncologist 14:22–28
Kishi Y, Zorzi D, Contreras CM et al (2010) Extended preoperative chemotherapy does not improve pathologic response and increases postoperative liver insufficiency after hepatic resection for colorectal liver metastases. Ann Surg Oncol 17:2870–2876
Klinger M, Eipeldauer S, Hacker S et al (2009) Bevacizumab protects against sinusoidal obstruction syndrome and does not increase response rate in neoadjuvant XELOX/FOLFOX therapy of colorectal cancer liver metastases. Eur J Surg Oncol 235:515–520
Acknowledgements
The authors thank all patients and co-investigators for their cooperation in the TRICC0808 study.
Funding
This study was conducted jointly by Tokyo Medical and Dental University and Foundation for Biomedical Research and Innovation (Kobe, Japan; http://www.ibri-kobe.org/english/foundation.html), with funding supplied by Foundation for Biomedical Research and Innovation. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Uetake Hiroyuki received honoraria from Taiho Pharmaceutical, Chugai, Takeda, Merk, Eli Lilly, Sanofi and Bayer, and received research funding from Taiho, Chugai, and Takeda; Kenichi Sugihara received honoraria from Chugai, Taiho, Takeda, Bristol-Meyers Squib, Eli Lilly, Novartis, Bayer Yakuhin, and Sanofi, and received research funding from Chugai and Taiho; Megumi Ishiguro received honoraria from Taiho Pharmaceutical, Yakult Honsha and Merck Serono, and received research funding from Taiho Pharmaceutical and Yakult Honsha. None of the remaining authors has conflicts of interest that could be perceived as prejudicing the impartiality of the research reported and none has any financial support from industrial companies that are related with this research.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
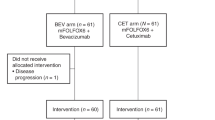
Supplemental Figure 1
. Trial progress. Abbreviations; CR, complete response; NE, not evaluated; PD, progressive disease; PR, partial response; SD, stable disease. *: Hepatectomy after 4 cycle therapy (PPTX 51 KB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Yasuno, M., Uetake, H., Ishiguro, M. et al. mFOLFOX6 plus bevacizumab to treat liver-only metastases of colorectal cancer that are unsuitable for upfront resection (TRICC0808): a multicenter phase II trial comprising the final analysis for survival. Int J Clin Oncol 24, 516–525 (2019). https://doi.org/10.1007/s10147-018-01393-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-01393-8