Abstract
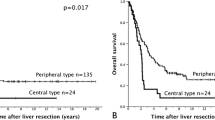
From 1960 to 1992 a total of 1718 patients with liver metastases from colorectal carcinoma were recorded. Of these patients, 469 (27.3%) underwent hepatic resection, which was performed with curative intent in 434 patients (25.3%). Operative mortality in this group was 4.4%, being 1.8% (2 of 114) during the last 3 years. Significant morbidity was observed in 16% of patients with a decrease to 5% (6 of 112) for the last 3 years. A 99.8% follow-up until November 1, 1993 was achieved. Excluding operative mortality, there are 350 patients with “potentially curative” resection and 65 corresponding patients with minimal macroscopic (n=19) or microscopic (n=46) residual disease. The latter group demonstrated a poor prognosis, with median and maximum survival times of 14.4 and 56.0 months, respectively. Among the 350 patients having potentially curative resection, the actuarial 5-, 10-, and 20-year survivals were 39.3%, 23.6%, and 17.7%, respectively. Tumor-free survival was 33.6% at 5 years. In the univariate analysis, the following factors were associated with decreased crude survival: presence and extent of mesenteric lymph node involvement (p=0.0001); grade III/IV primary tumor (p=0.013); synchronous diagnosis of metastases (p=0.014); satellite metastases (p=0.00001); metastasis diameter of>5 cm (p=0.003); preoperative carcinoembryonic antigen (CEA) elevation (p=0.03); limited resection margins (p=0.009); extrahepatic disease (p=0.009); and nonanatomic procedures (p=0.008). With respect to disease-free survival, extrahepatic disease (p=0.09) failed to achieve statistical significance, whereas patients with primary tumors in the colon did significantly better than those with rectal cancer (p=0.04). The presence of five or more independent metastases adversely affected resectability (p<0.05). However, once a radical excision of all detectable disease was achieved, no significant predictive value of an increasing number of metastases (1–3 versus≥4) on either overall (p=0.40) or disease-free (p=0.64) survival was found. Using Cox's multivariate regression analysis, the presence of satellite metastases, primary tumor grade, the time of metastasis diagnosis diameter of the largest metastasis, anatomic versus nnanatomic approach, year of resection, and mesenteric lymph node involvement each independently affected both crude and tumor-free survival.
Résumé
Entre 1960 et 1992, un total de 1718 patients ayant des métastases d'un cancer d'origine colorectale ont été enregistrés. Quatre cent soixante-neuf patients (27.3%) ont eu une résection hépatique qui a été effectuée avec une intention curatrice chez 434 (25.3%_. La mortalité opératoire a été de 4.4%, mais seulement de 1.8% pendant ces trois dernières années (2/114). La morbidité globale a été de 16%, et de 5% pendant ces trois dernières années (5/112). A la date du 1 Novembre 1993, on avait des nouvelles de 99.8% des patients. Après exclusion des patients décédés pendant l'intervention, 350 patients ont eu une résection «potentiellement» curatrice. Parmi ceux-là, 65 étaient le siège de tumeur résiduelle soit macroscopique (n=19) soit microscopique (n=46). Parmi ces derniers, le pronostic était moins bon car la médiane et le maximum de survie a été respectivement de 14.4 et 56 mois. Parmi les 350 patients ayant une cure «potentiellement» curatrice, la survie actuarielle à 5, 10 et à 20 ans a été respectivement de 39.3%, de 23.6% et de 17.7%. La survie sans tumeur a été de 33.6% à 5 ans. En analyse univariable, les facteurs suivants ont été associés avec une diminution de survie globale: présence de métastase lymphatique mésentérique étendue (p=0.0001), tumeur primitive stade III/IV (p=0.013), métastase synchrone (p=0.014), métastases satellites (p=0.00001), diamètre de métastase>5 cm (p=0.003), taux d'ACE élevé (p=0.03), marges de résection limitée (p=0.009), cancer extrahépatique (p=0.0009), et intervention non-anatomique (p=0.008). En ce qui concerne la survie sans tumeur, la présence de cancer extra-hépatique n'a pas atteint de signification statistique, alors que les patients avec un cancer primitif du côlon avaient un pronostic meilleur que ceux qui avaient un cancer du rectum (p=0.04). La présence de cinq métastases indépendantes ou plus influençait la résequabilité en sens inverse (p<0.05). Une fois qu'une résection radicale de toute maladie détectable a été faite, le nombre de métastases (1–3 vs. 4 ou+) n'avait plus de valeur prédictive sur ni la survie globale (p=0.40) ni la maladie sans métastases (p=0.64). En utilisant le modèle de Cox, la présence de métastases satellites, le stade de la tumeur primitive, le moment du diagnostic de métastases, le plus grand diamètre, de métastase, l'approche anatomique ou pas, l'année de la résection et la présence d'envahissement lymphatique mésentérique ont tous été des facteurs indépendants influençant la survie globale et la survie sans tumeur.
Resumen
En el período 1960 a 1992 registramos un total de 1.718 pacientes con metástasis hepáticas de carcinomas colorectales; 469 (27.3%) fueron sometidos a resección, la cual fue realizada con propósito curativo en 434 pacientes (25.3%). La mortalidad en este grupo fue 4.4%, siendo 1.8% (2 de 114) en los últimos 3 años. Se observó morbilidad significativa en 16% de los casos con una disminución a 5% (6 de 112) en los últimos 3 anños. Hasta noviembre 1 de 1993, se logró un 99.8% de seguimiento. Excluyendo la mortalidad operatoria, hay 350 pacientes con resección “potencialmente curativa” y 65 pacientes con enfermedad residual macroscópica mínima (n=19) o microscópica (n=46). Este último grupo demuestra el pronóstico tan pobre con una sobrevida media y máxima de 14.4 y 56 meses, respectivamente. Entre los 350 pacientes que tuvieron una resección potencialmente curativa la tasa actuarial de sobrevida a 5, 10 y 20 años fue 39.3%, 23.6% y 17.7%, respectivamente. La tasa de sobrevida libre de tumor fue de 33.6% a 5 años. En el análisis univariable, los siguientes factores aparecieron asociados con disminución de la tasa cruda de sobrevida: presencia o extensión de la invasión ganglionar mesentérica (p=0.0001), tumor primario grado III/IV (p=0.013), diagnóstico sincrónico de metástasis (p=0.014), metástasis satélites (p=0.00001), diámetro de las metástasis>5 cm (p=0.003), elevación preoperatoria del CEA (p=0.03), márgenes limitados de resección (p=0.009), enfermedad extrahepática (p=0.009) y procedimiento no anatómico (p=0.008). Con respecto a la sobrevida libre de enfermedad, las lesiones extrahepáticas (p=0.09) demostraron no tener significancia estadística; los pacientes con tumores primarios del colon evolucionaron significativamente mejor que los pacientes con cáncer rectal (p=0.04). La presencia de 5 o más metástasis independientes afecta la resecabilidad (p<0.05). Sin embargo, una vez lograda la resección radical de todas las metástasis, no se encontró un valor significativo de predicción según un númeo creciente de metástasis (1–3 vs ≥ 4) sobre la tasa global de sobrevida (p=0.40) o sobre la tasa de sobrevida libre de enfermedad (p=0.64). En el análisis multivariable de regresión de Cox se encontró que los siguientes factores afectan en forma independiente la tasa cruda de sobrevida y la tasa de sobrevida libre de tumor: presencia de metástasis satélites, grado del tumor primario, momento del diagnóstico de las metástasis, diámetro de la mayor de las metástasis, abordaje anatómico vs no anatómico, año en que se efectuó la resección e invasión de los ganglios linfáticos mesentéricos.
Similar content being viewed by others
References
Adson, M.A.: Resection of liver metastases: when is it worthwhile. World J. Surg. 11:511, 1987
Scheele, J., Altendorf-Hofmann, A., Stangl, R., et al.: Hepatic metastases from colorectal carcinoma: impact of surgical resection on the natural history. Br. J. Surg. 77:1241, 1990
Hughes, K.S., Simon, R.M., Songhorabodi, S., et al.: Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of indications for resection. Surgery 103:278, 1988
Nordlinger, B., Jaeck, D., Guiguet, M., et al.: Surgical resection of hepatic metastases: multicentric retrospective study by the French Association of Surgery. In Treatment of Hepatic Metastases, B. Nordlinger, editor. Paris, Springer, 1992, pp. 129–146
Doci, R., German, L., Bigami, P., et al.: One hundred patients with hepatic metastases from colorectal cancer treated by resection: analysis of prognostic determinants. Br. J. Surg. 78:797, 1991
Adson, M.A.: Diagnosis and surgical treatment of primary and secondary solid hepatic tumors in the adult. Surg. Clin. North Am. 61:181, 1981
Butler, J., Attiyeh, F.F., Daly, J.M.: Hepatic resection for metastases of the colon and rectum. Surg. Gynecol. Obstet. 162:109, 1986
Scheele, J., Stangl, R., Altendorf-Hofmann, A., Gall, F.P.: Indicators of prognosis after hepatic resection for colorectal secondaries. Surgery 110:13, 1991
Scheele, J., Stangl, R.: Segment-orientated anatomical liver resections. In Surgery of the Liver and Biliary Tract (2nd ed.), L.H. Blumgart, editor. Edinburgh, Churchill Livingstone, 1994, pp. 1557–1578
Gabriel, W.B., Dukes, C., Bussey, H.J.R.: Lymphatic spread in cancer of the rectum. Br. J. Surg. 23:395, 1935
Iwatsuki, S., Esquivel, C.O., Gordon, R.D., Starzl, T.E.: Liver resection for metastatic colorectal cancer. Surgery 100:804, 1986
Holm, A., Bradley, E., Joaquim, S., Aldrek, S.: Hepatic resection of metastasis from colorectal carcinoma. Ann. Surg. 209:428, 1990
Bismuth, H., Castaing, D., Traynor, O.: Surgery for synchronous hepatic metastases of colorectal cancer. Scand. J. Gastroenterol. 23:144, 1988
Genari, L., Doci, R., Bignami, P., Bozetti, F.: Surgical treatment of hepatic metastases from colorectal cancer. Ann. Surg. 203:49, 1986
Cady, B., McDermott, W.V., Jr.: Major hepatic resection for metachronous metastases from colon cancer. Ann. Surg. 201:204, 1985
Pichlmayr, R., Grosse, H., Haus, J., et al.: Technique and preliminary results of extracorporeal liver surgery (bench procedure) and of surgery on the in situ perfused liver. Br. J. Surg. 77:21, 1990
Åberg, T., Malmberg, K.A., Nilsson, B., et al.: The effect of metastasectomy: fact or fiction. Ann. Thorac. Surg. 30:378, 1980
Silen, W.: Hepatic resection for metastases from colorectal carcinoma is of dubious value. Arch. Surg. 124:1021, 1989
Cady, B.: Lymph node metastases: indicators, but not governors of survival. Arch. Surg. 119:1067, 1984
Makuuchi, M., Hasegawa, H., Yamazaki, S.: Ultrasonically guided subsegmentectomy. Surg. Gynecol. Obstet. 161:346, 1985
Feinstein, A.R., Sosin, D.M., Wells, C.K.: The Will Rogers phenomenon: stage migration and new diagnostic techniques as a source of misleading statistics for survival in cancer. N. Engl. J. Med. 312:1604, 1985
Wilson, S.M., Adson, M.A.: Surgical treatment of hepatic metastases from colorectal cancers. Arch. Surg. 111:330, 1976
Adson, M.A., van Heerden, J.A.: Major hepatic resection for metastatic colorectal cancer. Ann. Surg. 191:576, 1980
Logan, S.E., Meier, S.J., Ramming, K.P., et al.: Hepatic resection for metastatic colorectal carcinoma: a ten-year experience. Arch. Surg. 117:25, 1982
August, D.A., Sugarbaker, P.H., Ottow, R.T., et al.: Hepatic resection of colorectal metastases: influence of clinical factors and adjuvant intraperitoneal 5-fluorouracil via Tenckhoff catheter on survival. Ann. Surg. 201:210, 1985
Taylor, I.: Colorectal liver metastases-to treat or not to treat? Br. J. Surg. 72:511, 1985
Attiyeh, F.F., Wichern, W.A., Jr.: Hepatic resection for primary and metastatic tumors. Am. J. Surg. 156:368, 1988
Hohenberger, P., Schlag, P., Schwarz, V., et al.: Leberresektion bei Patienten mit Metastasen colorectaler Carcinome: Ergebnisse und prognostische Faktoren. Chirurg 59:410, 1988
Fortner, J.G., Silva, J.S., Golbey, R.B., et al.: Multi-variate analysis of a personal series of 247 consecutive patients with liver metastases from colorectal cancer. I. Treatment by hepatic resection. Ann. Surg. 199:306, 1984
Ekberg, M., Tranberg, K.G., Andersson, R., et al.: Determinants of survival in liver resection for colorectal secondaries. Br. J. Surg. 73:727, 1986
Hughes, K., Scheele, J., Sugarbaker, P.H.: Surgery for metastatic colorectal cancer to the liver: optimizing the results of treatment. Surg. Clin. North Am. 69:339, 1989
Saenz, N.C., Cady, B., McDermott, W.V., Jr., et al.: Experience with colorectal carcinoma metastatic to the liver. Surg. Clin. North Am. 69:361, 1989
Sugihara, K., Hojo, K., Moriya, Y., et al.: Pattern of recurrence after hepatic resection for colorectal metastases. Br. J. Surg. 80:1032, 1993
Gall, F.P., Scheele, J.: Die operative Therapie von Lebermetastasen. In Chirurgische Behandlung von Tumormetastasen, F.W. Schildberg, editor. Melsungen, Bibliomed, 1986, pp. 223–240
Brown, D.A., Pommier, R.F., Woltering, E.A., et al.: Nonanatomic hepatic resection for secondary hepatic tumors with special reference to hemostatic technique. Arch. Surg. 123:1063, 1988
Cady, B., Stone, M.D.: The role of surgical resection of liver metastases in colorectal carcinoma. Semin. Clin. Oncol. 18:399, 1991
Viadana, E., Bross, I.D.J., Pickren, J.W.: Cascade spread of blood-borne metastases in solid and nonsolid cancers of humans. In Pulmonary Metastases, L. Weiss, H.A. Gilbert, editors. Boston, G.K. Hall, 1978, pp. 142–167
Hegemann, G., Mühe, E.: Die Resektion von Metastasen und Rezidiven: Indikation und Ergebnisse. Dtsch. Med. Wochenschr. 99:989, 1974
Iwatsuki, S., Starzl, T.E.: Personal experience with 411 hepatic resections. Ann. Surg. 208:421, 1988
Fortner, J.G.: Recurrence of colorectal cancer after hepatic resection. Am. J. Surg. 155:378, 1988
Author information
Authors and Affiliations
Additional information
This paper is dedicated to Gerd Hegemann, Emeritus Professor of Surgery, outstanding teacher of surgical thinking and practice.
Rights and permissions
About this article
Cite this article
Scheele, J., Stang, R., Altendorf-Hofmann, A. et al. Resection of colorectal liver metastases. World J. Surg. 19, 59–71 (1995). https://doi.org/10.1007/BF00316981
Issue Date:
DOI: https://doi.org/10.1007/BF00316981