Abstract
Background
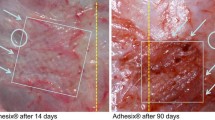
The aim of the study was to evaluate the influence of the pore size of a polypropylene mesh on the shrinkage and elasticity of the mesh–tissue complex and the inflammatory reaction to the implant in an open onlay hernia repair.
Materials and methods
Twenty-one 10 × 10 cm samples of polypropylene meshes of a different pore size (3.0 × 2.8 mm—PP3, 1.0 × 0.8 mm—PP1 and 0.6 × 0.5 mm—PP.5) were implanted in an onlay position in 21 New Zealand white rabbits. After 90 days of implantation the shrinkage, elasticity and foreign body reaction (FBR) were assessed.
Results
The shrinkage of PP3 was 30.6 ± 4.3 %, PP1 49.3 ± 2.9 % and PP.5 49.5 ± 2.6 %. The shrinkage of PP3 was significantly lower (PP3 × PP1 p = 0.007, PP3 × PP.5 p = 0.005), PP1 and PP.5 were similar. The elasticity was similar. The strength of FBR in mesh pores was similar. The width of foreign body granuloma layers at the mesh–tissue interface was significantly reduced with increasing pore size (inner: PP3 10.1 ± 1.2; PP1 12.5 ± 2.9; PP.5 17.4 ± 5.2 and outer: PP3 21.2 ± 2.5; PP1 30.6 ± 6.3; PP.5 60.4 ± 14.9). All differences between the widths of granuloma layers were statistically significant (p < 0.010). One animal (PP1) was excluded because of a mesh infection.
Conclusions
Implantation of polypropylene mesh of a pore size of 3 mm in an onlay position is associated with a significant reduction of shrinkage in comparison to a 1 mm pore lightweight and 0.5 mm pore heavyweight mesh. A pore size increase to 3 mm is not sufficient for an improvement of mesh–tissue complex elasticity in comparison to a 1 mm pore lightweight and 0.5 mm heavyweight mesh. Polypropylene mesh with enlarged pores to 3 mm is associated with a similar strength of FBR in mesh pores and a reduced foreign body granuloma in comparison to a 1 mm pore lightweight and 0.5 mm pore heavyweight mesh.








Similar content being viewed by others
References
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13:343–403
Korenkov M, Paul A, Sauerland S, Neugebauer E, Arndt M, Chevrel JP et al (2001) Classification and surgical treatment of incisional hernia. Results of an experts’ meeting. Langenbecks Arch Surg 386:65–73
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20:86–100
Amid PK (2003) The Lichtenstein repair in 2002: an overview of causes of recurrence after Lichtenstein tension-free hernioplasty. Hernia 7:13–16
Klinge U, Klosterhalfen B, Müller M, Ottinger AP, Schumpelick V (1998) Shrinking of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg 164:965–969
Klinge U, Junge K, Stumpf M, Ottinger AP, Klosterhalfen B (2002) Functional and morphological evaluation of a low-weight, monofilament polypropylene mesh for hernia repair. J Biomed Mater Res 63:129–136
Welty G, Klinge U, Klosterhalfen B, Kasperk R, Schumpelick V (2001) Functional impairment and complaints following incisional hernia repair with different polypropylene meshes. Hernia 5:142–147
Amid PK (1997) Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1:15–21
Klosterhalfen B, Junge K, Klinge U (2005) The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices 2:103–117
Eriksson A, Rosenberg J, Bisgaard T (2013) Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia doi:10.1007/s10029-013-1066-y
den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW (2008) Open surgical procedures for incisional hernias. Cochrane Database Syst Rev doi:10.1002/14651858.CD006438.pub2
Binnebösel M, Klink CD, Otto J, Conze J, Jansen PL, Anurov M, Schumpelick V, Junge K (2010) Impact of mesh positioning on foreign body reaction and collagenous ingrowth in a rabbit model of open incisional hernia repair. Hernia 14:71–77
Melman L, Jenkins ED, Hamilton NA, Bender LC, Brodt MD, Deeken CR, Greco SC, Frisella MM, Matthews BD (2011) Histologic and biomechanical evaluation of a novel macroporous polytetrafluoroethylene knit mesh compared to lightweight and heavyweight polypropylene mesh in a porcine model of ventral incisional hernia repair. Hernia 15:423–431
Pascual G, Rodríguez M, Sotomayor S, Pérez-Köhler B, Bellón JM (2012) Inflammatory reaction and neotissue maturation in the early host tissue incorporation of polypropylene prostheses. Hernia 16:697–707
Pascual G, Hernández-Gascón B, Rodríguez M, Sotomayor S, Peña E, Calvo B, Bellón JM (2012) The long-term behavior of lightweight and heavyweight meshes used to repair abdominal wall defects is determined by the host tissue repair process provoked by the mesh. Surgery 152:886–895
Cobb WS, Burns JM, Peindl RD, Carbonell AM, Matthews BD, Kercher KW et al (2006) Textile analysis of heavy weight, mid-weight, and light weight polypropylene mesh in a porcine ventral hernia model. J Surg Res 136:1–7
Coda A, Lamberti R, Martorana S (2012) Classification of prosthetics used in hernia repair based on weight and biomaterial. Hernia 16:9–20
Weyhe D, Belyaev O, Müller C, Meurer K, Bauer KH, Papapostolou G, Uhl W (2007) Improving outcomes in hernia repair by the use of light meshes—a comparison of different implant constructions based on a critical appraisal of the literature. World J Surg 31:234–244
Mühl T, Binnebösel M, Klinge U, Goedderz T (2008) New objective measurement to characterize the porosity of textile implants. J Biomed Mater Res B Appl Biomater 84:176–183
García-Ureña MA, Vega Ruiz V, Díaz Godoy A, Báez Perea JM, Marín Gómez LM, Carnero Hernández FJ et al (2007) Differences in polypropylene shrinkage depending on mesh position in an experimental study. Am J Surg 193:538–542
Conze J, Junge K, Klinge U, Weiss C, Polivoda M, Oettinger AP et al (2005) Intraabdominal adhesion formation of polypropylene mesh. Influence of coverage of omentum and polyglactin. Surg Endosc 19:798–803
Gonzalez R, Fugate K, McClusky D 3rd, Ritter EM, Lederman A, Dillehay D et al (2005) Relationship between tissue ingrowth and mesh contraction. World J Surg 29:1038–1043
Conze J, Prescher A, Kisielinski K, Klinge U, Schumpelick V (2005) Technical consideration for subxiphoidal incisional hernia repair. Hernia 9:84–87
Ozog Y, Konstantinovic ML, Werbrouck E, De Ridder D, Edoardo M, Deprest J (2011) Shrinkage and biomechanical evaluation of lightweight synthetics in a rabbit model for primary fascial repair. Int Urogynecol J 22:1099–1108
Zogbi L, Trindade EN, Trindade MR (2013) Comparative study of shrinkage, inflammatory response and fibroplasia in heavyweight and lightweight meshes. Hernia 17:765–772
Potic M, Ignjatovic I, Savic V, Djekic P, Radenkovic G (2011) Mechanical properties and tissue reinforcement of polypropylene grafts used for pelvic floor repair—an experimental study. Hernia 15:685–690
Zhong C, Wu B, Yang Z, Deng X, Kang J, Guo B, Fan Y (2013) A meta-analysis comparing lightweight meshes with heavyweight meshes in Lichtenstein inguinal hernia repair. Surg Innov 20:24–31
Li J, Ji Z, Cheng T (2012) Lightweight versus heavyweight in inguinal hernia repair: a meta-analysis. Hernia 16:529–539
Junge K, Binnebösel M, von Trotha KT, Rosch R, Klinge U, Neumann UP, Lynen Jansen P (2012) Mesh biocompatibility: effects of cellular inflammation and tissue remodelling. Langenbecks Arch Surg 397:255–270
Acknowledgments
This study was funded by Výzkumný ústav pletařský, a.s., Brno, The Czech Republic.
Conflict of interest
Drs. J. J., T. N., K. V., J. C., V. J., P. V. and I. C. have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jerabek, J., Novotny, T., Vesely, K. et al. Evaluation of three purely polypropylene meshes of different pore sizes in an onlay position in a New Zealand white rabbit model. Hernia 18, 855–864 (2014). https://doi.org/10.1007/s10029-014-1278-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-014-1278-9