Abstract
Introduction and hypothesis
The experiment evaluated different lightweights (<32 g/m2) in terms of shrinkage and biomechanics.
Methods
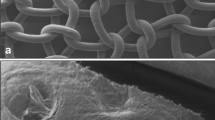
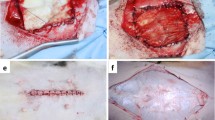
PP-8 (polypropylene of 7.6 g/m2), PP-s (PP-8 with absorbable sheets), PP-32 (PP with absorbable fibers; 32.0 g/m2) and polyvinylidinefluoride (PVDF; 24.9 g/m2) augmented primary sutured repairs of the anterior abdominal wall in a total of 40 rabbits. Rabbits were implanted by only one type of mesh at four abdominal sites. After 7, 14, 30, 60 and 120 days, 2 rabbits were sacrificed per group. Three additional unoperated rabbits were used as controls. Shrinkage and uni-axial tensiometry were evaluated.
Results
PP-s implants wrinkled in 70%. PP-32 did not shrink whereas PP-8 and PVDF shrank by 20%. Explants were as strong as the controls; however, they differed in compliance. At lower stress, the tested materials were equally stiff.
Conclusions
The biomechanical behaviour of the tested lightweights does not mimic that of native controls. Weight reduction does not prevent shrinkage.





Similar content being viewed by others
References
Jia X, Glazener C, Mowatt G, MacLennan G, Bain C, Fraser C et al (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. BJOG 115:1350–1361
Quiroz LH, Gutman RE, Shippey S, Cundiff GW, Sanses T, Blomquist JL et al (2008) Abdominal sacrocolpopexy: anatomic outcomes and complications with Pelvicol, autologous and synthetic graft materials. Am J Obstet Gynecol 198:557 e1–5
Altman D, Anzen B, Brismar S, Lopez A, Zetterstrom J (2006) Long-term outcome of abdominal sacrocolpopexy using xenograft compared with synthetic mesh. Urology 67:719–724
Deprest J, De Ridder D, Roovers J, Werbrouck E, Coremans G, Claerhout F (2009) Medium term outcome of laparoscopic sacrocolpopexy with xenografts as compared to synthetic grafts. Urology 182(5):2362–2368
Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S (2008) Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn 27:3–12
Feiner B, Jelovsek JE, Maher C (2009) Efficacy and safety of transvaginal mesh kits in the treatment of prolapse of the vaginal apex: a systematic review. BJOG 116:15–24
Bako A, Dhar R (2009) Review of synthetic mesh-related complications in pelvic floor reconstructive surgery. Int Urogynecol J Pelvic Floor Dysfunct 20:103–111
Kohli N, Walsh PM, Roat TW, Karram MM (1998) Mesh erosion after abdominal sacrocolpopexy. Obstet Gynecol 92:999–1004
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12:63–69
Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V (2002) Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res 103:208–214
Jones KA, Feola A, Meyn L, Abramowitch SD, Moalli PA (2009) Tensile properties of commonly used prolapse meshes. Int Urogynecol J 20(7):847–853
Ozog Y, Konstantinovic ML, Verschueren S, Spelzini F, De Ridder D, Deprest J (2009) Experimental comparison of abdominal wall repair using different methods of enhancement by small intestinal submucosa graft. Int Urogynecol J Pelvic Floor Dysfunct 20(4):435–441
Sergent F, Desilles N, Lacoume Y, Bunel C, Marie JP, Marpeau L (2009) Experimental biomechanical evaluation of polypropylene prostheses used in pelvic organ prolapse surgery. Int Urogynecol J Pelvic Floor Dysfunct. Epub ahead of print
Movat HZ (1955) Demonstration of all connective tissue elements in a single section; pentachrome stains. AMA Arch Pathol 60:289–295
Rubod C, Boukerrou M, Brieu M, Jean-Charles C, Dubois P, Cosson M (2008) Biomechanical properties of vaginal tissue: preliminary results. Int Urogynecol J Pelvic Floor Dysfunct 19(6):811–816
Junge K, Rosch R, Krones CJ, Klinge U, Mertens PR, Lynen P et al (2005) Influence of polyglecaprone 25 (Monocryl) supplementation on the biocompatibility of a polypropylene mesh for hernia repair. Hernia 9:212–217
Conze J, Junge K, Weiss C, Anurov M, Oettinger A, Klinge U et al (2008) New polymer for intra-abdominal meshes—PVDF copolymer. J Biomed Mater Res B Appl Biomater 87:321–328
Konstantinovic ML, Pille E, Malinowska M, Verbeken E, De Ridder D, Deprest J (2007) Tensile strength and host response towards different polypropylene implant materials used for augmentation of fascial repair in a rat model. Int Urogynecol J Pelvic Floor Dysfunct 18(6):619–626
Konstantinovic ML, Ozog Y, Spelzini F, Pottier C, De Ridder D, Deprest J (2009) Biomechanical findings in rats undergoing fascial reconstruction with graft materials suggested as an alternative to polypropylene. Neurourol Urodyn 29(3):488–493
Garcia-Urena MA, Vega Ruiz V, Diaz Godoy A, Baez Perea JM, Marin Gomez LM, Carnero Hernandez FJ et al (2007) Differences in polypropylene shrinkage depending on mesh position in an experimental study. Am J Surg 193:538–542
Klinge U, Klosterhalfen B, Muller M, Ottinger AP, Schumpelick V (1998) Shrinking of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg 164:965–969
Klosterhalfen B, Junge K, Klinge U (2005) The lightweight and large porous mesh concept for hernia repair. Expert Rev Med Devices 2:103–117
Deprest J, Zheng F, Konstantinovic M, Spelzini F, Claerhout F, Steensma A et al (2006) The biology behind fascial defects and the use of implants in pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct 17(Suppl 1):S16–S25
Bellon JM, Garcia-Honduvilla N, Rodriguez M, Pascual G, Gomez-Gil V, Bujan J (2006) Influence of the structure of new generation prostheses on shrinkage after implant in the abdominal wall. J Biomed Mater Res B Appl Biomater 78:340–346
Epstein LB, Graham CA, Heit MH (2007) Systemic and vaginal biomechanical properties of women with normal vaginal support and pelvic organ prolapse. Am J Obstet Gynecol 197:165 e1–6
Epstein LB, Graham CA, Heit MH (2008) Impact of sacral colpopexy on in vivo vaginal biomechanical properties. Am J Obstet Gynecol 199:664 e1–6
Epstein LB, Graham CA, Heit MH (2008) Correlation between vaginal stiffness index and pelvic floor disorder quality-of-life scales. Int Urogynecol J Pelvic Floor Dysfunct 19:1013–1018
Abramowitch SD, Feola A, Jallah Z, Moalli PA (2009) Tissue mechanics, animal models, and pelvic organ prolapse: a review. Eur J Obstet Gynecol Reprod Biol 144(Suppl 1):S146–S158
Conflicts of interest
This work was supported by an unconditional grant from Johnson & Johnson Medical (Norderstedt Germany). The company did not interfere with the planning, execution or reporting of this experiment and is neither the owner of the results. The authors have no financial interests in this company.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was awarded with the Young Investigators Award at the biannual joint meeting of the International Continence Society the International Urogynecology Association, held in Toronto, ON, August 23-27, 2010.
Rights and permissions
About this article
Cite this article
Ozog, Y., Konstantinovic, M.L., Werbrouck, E. et al. Shrinkage and biomechanical evaluation of lightweight synthetics in a rabbit model for primary fascial repair. Int Urogynecol J 22, 1099–1108 (2011). https://doi.org/10.1007/s00192-011-1440-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1440-1