Abstract
Objectives
Evaluate the effects of ionizing radiation on microarchitecture, the osteocyte lacunar network, and collagen maturity in a bone repair site.
Materials and methods
Bone defects were created on tibias of 20 New Zealand rabbits. After 2 weeks, the animals were randomly divided into (n = 10) NoIr (nonirradiated group) and Ir (irradiated group). In the Ir, the animals received single-dose irradiation of 30 Gy on the tibia and were euthanized after 2 weeks. Bone microarchitecture parameters were analyzed by using micro-CT, and the osteocyte lacunar network, bone matrix, and collagen maturation by histomorphometric analysis. The data were analyzed using unpaired Student’s t test (α = 0.05).
Results
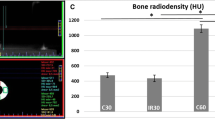
Trabecular thickness in Ir was lower than that in NoIr (P = 0.028). No difference was found for bone volume fraction and bone area. Lacunae filled with osteocytes were more numerous (P < 0.0001) in NoIr (2.6 ± 0.6) than in Ir (1.97 ± 0.53). Empty lacunae were more prevalent (P < 0.003) in Ir (0.14 ± 0.10) than in NoIr (0.1 ± 0.1). The mean osteocyte lacunae size was higher (P < 0.01) in Ir (15.4 ± 4.41) than in NoIr (12.7 ± 3.7). Picrosirius red analysis showed more (P < 0.05) mature collagen in NoIr (29.0 ± 5.3) than in Ir (23.4 ± 4.5). Immature collagen quantification revealed no difference between groups.
Conclusions
Ionizing radiation compromised bone formation and an impairment in bone repair in irradiated woven bone was observed.
Clinical relevance
Before radiotherapy, patients usually need surgical intervention, which may be better performed, if clinicians understand the repair process in irradiated bone, using novel approaches for treating these individuals.



Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global Cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Furdui CM (2014) Ionizing radiation: mechanisms and therapeutics. Antioxid Redox Signal 21(2):218–220. https://doi.org/10.1089/ars.2014.5935
Lima F, Swift JM, Greene ES, Allen MR, Cunningham DA, Braby LA, Bloomfield SA (2017) Exposure to low-dose X-ray radiation alters bone progenitor cells and bone microarchitecture. Radiat Res 188(4):433–442. https://doi.org/10.1667/RR14414.1
Bartlow CM, Mann KA, Damron TA, Oest ME (2018) Limited field radiation therapy results in decreased bone fracture toughness in a murine model. PLoS One 13(10):1–22. https://doi.org/10.1371/journal.pone.0204928
Pacheco R, Stock H (2013) Effects of radiation on bone. Curr Osteoporos Rep 11(4):299–304. https://doi.org/10.1007/s11914-013-0174-z
Chandra A, Lin T, Tribble MB, Zhu J, Altman AR, Tseng W, Zhang Y, Akintoye SO, Cengel K, Liu XS, Qin L (2014) PTH1-34 alleviates radiotherapy-induced local bone loss by improving osteoblast and osteocyte survival. Bone 67:33–40. https://doi.org/10.1016/j.bone.2014.06.030
Michel G, Blery P, Pilet P, Guicheux J, Weiss P, Malard O, Espitalier F (2015) Micro-CT analysis of radiation-induced osteopenia and bone hypovascularization in rat. Calcif Tissue Int 97(1):62–68. https://doi.org/10.1007/s00223-015-0010-9
Bellido T (2014) Osteocyte-driven bone remodeling. Calcif Tissue Int 94(1):25–34. https://doi.org/10.1007/s00223-013-9774-y
Bonewald LF (2011) The amazing osteocyte. J Bone Miner Res 26(2):229–238. https://doi.org/10.1002/jbmr.320
Chandra A, Lin T, Young T, Tong W, Ma X, Tseng WJ, Kramer I, Kneissel M, Levine MA, Zhang Y, Cengel K, Liu XS, Qin L (2017) Suppression of sclerostin alleviates radiation-induced bone loss by protecting bone-forming cells and their progenitors through distinct mechanisms. J Bone Miner Res 32(2):360–372. https://doi.org/10.1002/jbmr.2996
Dallas SL, Prideaux M, Bonewald LF (2013) The osteocyte: an endocrine cell ... and more. Endocr Rev 34(5):658–690. https://doi.org/10.1210/er.2012-1026
Inyang AF, Schwarz DA, Jamali AM, Buchman SR (2010) Quantitative histomorphometric assessment of regenerate cellularity and bone quality in mandibular distraction osteogenesis after radiation therapy. J Craniofac Surg 21(5):1438–1442. https://doi.org/10.1097/SCS.0b013e3181ec693f
Kang SY, Deshpande SS, Zheutlin AR, Donneys A, Rodriguez JJ, Nelson NS, Felice PA, Chepeha DB, Buchman SR (2017) Role of parathyroid hormone in regeneration of irradiated bone in a murine model of mandibular distraction osteogenesis. Head Neck 39(3):464–470. https://doi.org/10.1002/hed.24612
Rabelo GD, Beletti ME, Dechichi P (2010) Histological analysis of the alterations on cortical bone channels network after radiotherapy: a rabbit study. Microsc Res Tech 73(11):1015–1018. https://doi.org/10.1002/jemt.20826
Batista JD, Zanetta-Barbosa D, Cardoso SV, Dechichi P, Rocha FS, Pagnoncelli RM (2014) Effect of low-level laser therapy on repair of the bone compromised by radiotherapy. Lasers Med Sci 29(6):1913–1918. https://doi.org/10.1007/s10103-014-1602-8
Rocha FS, Dias PC, Limirio PHJO, Lara VC, Batista JD, Dechichi P (2017) High doses of ionizing radiation on bone repair: is there effect outside the irradiated site? Injury 48(3):671–673. https://doi.org/10.1016/j.injury.2016.11.033
Ma Y, Shen G (2012) Distraction osteogenesis after irradiation in rabbit mandibles. Br J Oral Maxillofac Surg 50(7):662–667. https://doi.org/10.1016/j.bjoms.2011.10.008
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25(7):1468–1486. https://doi.org/10.1002/jbmr.141
Irie MS, Rabelo GD, Spin-Neto R, Dechichi P, Borges JS, Soares PBF (2018) Use of micro-computed tomography for bone evaluation in dentistry. Braz Dent J29(3):227–238. https://doi.org/10.1590/0103-6440201801979
Martins DE, de Medeiros VP, Wajchenberg M, Paredes-Gamero EJ, Lima M, Reginato RD et al (2018) Changes in human intervertebral disc biochemical composition and bony end plates between middle and old age. PLoS One 13(9):e0203932. https://doi.org/10.1371/journal.pone.0203932
Szendröi M, Vajta G, Kovács L, Schaff Z, Lapis K (1984) Polarization colours of collagen fibres: a sign of collagen production activity in fibrotic processes. Acta Morphol Hung 32(1):47–55
Retamoso LB, da Cunha TDMA, Knop LAH, Shintcovsk RL, Tanaka OM (2009) Organization and quantification of the collagen fibers in bone formation during orthodontic tooth movement. Micron 40(8):827–830. https://doi.org/10.1016/j.micron.2009.07.003
Zhang WB, Zheng LW, Chua D, Cheung LK (2010) Bone regeneration after radiotherapy in an animal model. J Oral Maxillofac Surg 68(11):2802–2809. https://doi.org/10.1016/j.joms.2010.04.024
Ocaña RP, Rabelo GD, Sassi LM, Rodrigues VP, Alves FA (2017) Implant osseointegration in irradiated bone: an experimental study. J Periodontal Res 52(3):505–511. https://doi.org/10.1111/jre.12416
Wagermaier W, Klaushofer K, Fratzl P (2015) Fragility of bone material controlled by internal interfaces. Calcif Tissue Int 97(3):201–212. https://doi.org/10.1007/s00223-015-9978-4
Hörth RM, Kerschnitzki M, Aido M, Schmidt I, Burghammer M, Duda GN et al (2018) Correlations between nanostructure and micromechanical properties of healing bone. J Mech Behav Biomed Mater 77:258–266. https://doi.org/10.1016/j.jmbbm.2017.08.022
Soares PBF, Soares CJ, Limirio PHJO, de Jesus RNR, Dechichi P, Spin-Neto R, Zanetta-Barbosa D (2018) Effect of ionizing radiation after-therapy interval on bone : histomorphometric and biomechanical characteristics. https://doi.org/10.1007/s00784-018-2724-3
Green DE, Rubin CT (2014) Consequences of irradiation on bone and marrow phenotypes, and its relation to disruption of hematopoietic precursors. Bone 63:87–94. https://doi.org/10.1016/j.bone.2014.02.018
Oest ME, Franken V, Kuchera T, Strauss J, Damron TA (2015) Long-term loss of osteoclasts and unopposed cortical mineral apposition following limited field irradiation. J Orthop Res 33(3):334–342. https://doi.org/10.1002/jor.22761
Zhang J, Wang Z, Wu A, Nie J, Pei H, Hu W, Wang B, Shang P, Li B, Zhou G (2017) Differences in responses to X-ray exposure between osteoclast and osteoblast cells. J Radiat Res 58(6):791–802. https://doi.org/10.1093/jrr/rrx026
Ma J, Shi M, Li J, Chen B, Wang H, Li B, Hu J, Cao Y, Fang B, Zhao RC (2007) Senescence-unrelated impediment of osteogenesis from Flk1+ bone marrow mesenchymal stem cells induced by total body irradiation and its contribution to long-term bone and hematopoietic injury. Haematologica 92(7):889–896. https://doi.org/10.3324/haematol.11106
Maeda M (1988) Effects of irradiation on cortical bone and their time-related changes. A biomechanical and histomorphological study. J Bone Jt Surg Am 70:392–399. https://doi.org/10.2106/00004623-198870030-00011
Fregene A, Jing XL, Monson LA, Buchman SR (2009) Alteration in volumetric bone mineralization density gradation patterns in mandibular distraction osteogenesis following radiation therapy. Plast Reconstr Surg 124(4):1237–1244. https://doi.org/10.1097/PRS.0b013e3181b5a42f
Zheutlin AR, Deshpande SS, Nelson NS, Polyatskaya Y, Rodriguez JJ, Donneys A, Buchman SR (2015) A Histomorphometric analysis of radiation damage in an isogenic murine model of distraction osteogenesis. J Oral Maxillofac Surg 73(12):2419–2428. https://doi.org/10.1016/j.joms.2015.08.002
Burger EH, Klein-Nulend J, Smit TH (2003) Strain-derived canalicular fluid flow regulates osteoclast activity in a remodelling osteon-a proposal. J Biomech 36(10):1453–1459. https://doi.org/10.1016/S0021-9290(03)00126-X
O’Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA et al (2004) Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology 145(4):1835–1841. https://doi.org/10.1210/en.2003-0990
Ma YL, Dai RC, Sheng ZF, Jin Y, Zhang YH, Fang LN, Fan HJ, Liao EY (2008) Quantitative associations between osteocyte density and biomechanics, microcrack and microstructure in OVX rats vertebral trabeculae. J Biomech 41(6):1324–1332. https://doi.org/10.1016/j.jbiomech.2008.01.017
Hemmatian H, Laurent MR, Bakker AD, Vanderschueren D, Klein-Nulend J, van Lenthe GH (2018) Age-related changes in female mouse cortical bone microporosity. Bone 113:1–8. https://doi.org/10.1016/j.bone.2018.05.003
Poort LJ, Ludlage JHB, Lie N, Böckmann RA, Odekerken JCE, Hoebers FJ et al (2017) The histological and histomorphometric changes in the mandible after radiotherapy: an animal model. J Cranio-Maxillofacial Surg 45(5):716–721. https://doi.org/10.1016/j.jcms.2017.02.014
Donneys A, Nelson NS, Page EE, Deshpande SS, Felice PA, Tchanque-Fossuo CN et al (2015) Targeting angiogenesis as a therapeutic means to reinforce osteocyte survival and prevent nonunions in the aftermath of radiotherapy. Head Neck 37(9):1261–1267. https://doi.org/10.1002/hed.23744
Chen X, Wang L, Zhao K, Wang H (2018) Osteocytogenesis: roles of physicochemical factors, collagen cleavage and exogenous molecules. Tissue Eng B Rev 24(3):215–225. https://doi.org/10.1089/ten.teb.2017.0378
Merkel JR, DiPaolo BR, Hallock GG, Rice DC (1988) Type I and type III collagen content of healing wounds in fetal and adult rats. Exp Biol Med 187(4):493–497. https://doi.org/10.3181/00379727-187-42694
Ashhurst DE (1990) Collagen synthesized by healing fractures. Clin Orthop Relat Res 255:273–283
Liu SH, Yang RS, Al-Shaikh R, Lane JM (1995) Collagen in tendon, ligament, and bone healing. A current review. Clin Orthop Relat Res 318:265–278
Bland YS, Critchlow MA, Ashhurst DE (1999) The expression of the fibrillar collagen genes during fracture healing: heterogeneity of the matrices and differentiation of the osteoprogenitor cells. Histochem J31(3):221–225. https://doi.org/10.1023/A:1003954104290
Limirio PHJO, Soares PBF, Emi ETP, Lopes CCA, Rocha FS, Batista JD, Rabelo GD, Dechichi P (2019) Ionizing radiation and bone quality: time-dependent effects. Radiat Oncol 14:15. https://doi.org/10.1186/s13014-019-1219-y
Acknowledgments
The authors are grateful to the Department of Clinical Oncology at Federal University of Triângulo Mineiro (UFTM), MG, Brazil.
Funding
This study was financed in part by Fundação de Amparo à Pesquisa de Minas Gerais (FAPEMIG) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mendes, E.M., Irie, M.S., Rabelo, G.D. et al. Effects of ionizing radiation on woven bone: influence on the osteocyte lacunar network, collagen maturation, and microarchitecture. Clin Oral Invest 24, 2763–2771 (2020). https://doi.org/10.1007/s00784-019-03138-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03138-x