Abstract
Purpose
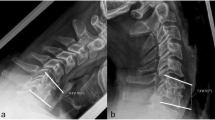
The purpose of the study is to describe the biomechanical theory explaining junctional breakdowns in thoraco-lumbar fusions, by taking the example of vertebral compression fractures. Also, a new angle, the cervical inclination angle (CIA), describing the relative position of the head at each vertebral level, is presented.
Methods
For the CIA, the data were collected from 137 asymptomatic subjects of a prospective database, containing clinical and radiologic informations. All the 137 subjects have an Oswestry score less than 15% and a pain score less than 2/10 and were part of a previously published study describing the Odontoïd-hip axis angle (ODHA). For each vertebral level from T1 to T12, the CIA as well as the vertical and horizontal distances was measured in reference to the sella turcica (ST), and a vertical line drawn from the ST. Average values and correlation coefficients were calculated.
Results
The CIA is an angle whose average value varies very little between T1 and T5 (74.9°–76.85°), and then increases progressively from T6 to T12. T1–T5 vertebra are always in line within the thoracic spine for each subject and can be considered as a straight T1–T5 segment. In addition, it was found that the vertical inclination of T1–T5 segment is correlated with the C7 slope (R 2 = 0.6383).
Conclusion
The T1–T5 segment inclination is correlated with the C7 slope, and because the latter defines the cervical curve as previously shown, the T1–T5 segment can be considered as the base from which the cervical spine originates. Its role is, thus, similar to the pelvis and its sacral slope, which is the base from which the lumbar spine originates. The CIA along with the ODHA, which describes the adequacy of the global balance in young and elderly asymptomatic populations, are two important parameters that could help us to better understand junctional breakdowns in thoraco-lumbar fusion surgeries.










Similar content being viewed by others
References
Cho SK, Shin JI, Kim YJ (2014) Proximal junctional kyphosis following adult spinal deformity surgery. Eur Spine J 23:2726–2736. https://doi.org/10.1007/s00586-014-3531-4
Hyun SJ, Kim YJ, Rhim SC (2016) Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J 16:1095–1101. https://doi.org/10.1016/j.spinee.2016.05.008
Mummaneni PV, Park P, Fu KM, Wang MY, Nguyen S, Lafage V, Uribe JS, Ziewacz J, Terran J, Okonkwo DO, Anand N, Fessler R, Kanter AS, LaMarca F, Deviren V, Bess RS, Schwab FJ, Smith JS, Akbarnia BA, Mundisjr GM, Shaffrey CI (2016) Does minimally invasive percutaneous posterior instrumentation reduce risk of proximal junctional kyphosis in adult spinal deformity surgery? A propensity-matched cohort analysis. Neurosurgery 78:101–108. https://doi.org/10.1227/neu.0000000000001002
Nguyen NL, Kong CY, Hart RA (2016) Proximal junctional kyphosis and failure-diagnosis, prevention, and treatment. Curr Rev Musculoskelet Med 9:299–308. https://doi.org/10.1007/s12178-016-9353-8
Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ, Kebaish K, Boachie-Adjei O, Complex Spine Study G (2014) Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976) 39:E607–E614. https://doi.org/10.1097/brs.0000000000000266
Hostin R, McCarthy I, O’Brien M, Bess S, Line B, Boachie-Adjei O, Burton D, Gupta M, Ames C, Deviren V, Kebaish K, Shaffrey C, Wood K, Hart R, International Spine Study G (2013) Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine 38:1008–1015. https://doi.org/10.1097/brs.0b013e318271319c
Ha Y, Maruo K, Racine L, Schairer WW, Hu SS, Deviren V, Burch S, Tay B, Chou D, Mummaneni PV, Ames CP, Berven SH (2013) Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine 19:360–369. https://doi.org/10.3171/2013.5.spine12737
Le Huec JC, Leijssen P, Duarte M, Aunoble S (2011) Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J 20(Suppl 5):669–680. https://doi.org/10.1007/s00586-011-1935-y
Bridwell KH, Lenke LG, Cho SK, Pahys JM, Zebala LP, Dorward IG, Cho W, Baldus C, Hill BW, Kang MM (2013) Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 72:899–906. https://doi.org/10.1227/NEU.0b013e31828bacd8
Cammarata M, Aubin CE, Wang X, Mac-Thiong JM (2014) Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976) 39:E500–E507. https://doi.org/10.1097/brs.0000000000000222
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 34:E729–E734. https://doi.org/10.1097/brs.0b013e3181ae2ab2
Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649
Yanik HS, Ketenci IE, Polat A, Ulusoy A, Deniz G, Kose O, Erdem S (2015) Prevention of proximal junctional kyphosis after posterior surgery of Scheuermann kyphosis: an operative technique. J Spinal Disord Tech 28:E101–105. https://doi.org/10.1097/BSD.0000000000000157
Kim HJ, Bridwell KH, Lenke LG, Park MS, Song KS, Piyaskulkaew C, Chuntarapas T (2014) Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976) 39:E576–E580. https://doi.org/10.1097/brs.0000000000000246
Kim HJ, Yagi M, Nyugen J, Cunningham ME, Boachie-Adjei O (2012) Combined anterior–posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 470:1633–1639. https://doi.org/10.1007/s11999-011-2179-1
Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33:2179–2184. https://doi.org/10.1097/brs.0b013e31817c0428
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 30:2045–2050
Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G, Yoon J (2007) Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976) 32:2731–2738. https://doi.org/10.1097/brs.0b013e31815a7ead
Lau D, Clark AJ, Scheer JK, Daubs MD, Coe JD, Paonessa KJ, LaGrone MO, Kasten MD, Amaral RA, Trobisch PD, Lee JH, Fabris-Monterumici D, Anand N, Cree AK, Hart RA, Hey LA, Ames CP, Committee SRSASD (2014) Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976) 39:2093–2102. https://doi.org/10.1097/brs.0000000000000627
Liu FY, Wang T, Yang SD, Wang H, Yang DL, Ding WY (2016) Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J 25:2376–2383. https://doi.org/10.1007/s00586-016-4534-0
Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, Deviren V, Burch S, William S, Ames CP, Mummaneni PV, Chou D, Berven SH (2013) Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38:E1469–E1476. https://doi.org/10.1097/brs.0b013e3182a51d43
Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL (2011) Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J 31:199–206
O’Leary PT, Bridwell KH, Lenke LG, Good CR, Pichelmann MA, Buchowski JM, Kim YJ, Flynn J (2009) Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: a matched cohort analysis performed at a single center. Spine (Phila Pa 1976) 34:2134–2139. https://doi.org/10.1097/brs.0b013e3181b2e17e
Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH (2016) Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. https://doi.org/10.1227/NEU.0000000000001240
Wang J, Zhao Y, Shen B, Wang C, Li M (2010) Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury 41:415–420. https://doi.org/10.1016/j.injury.2010.01.001
Yagi M, Akilah KB, Boachie-Adjei O (2011) Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976) 36:E60–E68. https://doi.org/10.1097/brs.0b013e3181eeaee2
Yagi M, King AB, Boachie-Adjei O (2012) Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976) 37:1479–1489. https://doi.org/10.1097/brs.0b013e31824e4888
Fechtenbaum J, Etcheto A, Kolta S, Feydy A, Roux C, Briot K (2016) Sagittal balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos Int 27:559–567. https://doi.org/10.1007/s00198-015-3283-y
Nachemson A (1965) The effect of forward leaning on lumbar intradiscal pressure. Acta Orthop Scand 35:314–328
Skalli W, Champain S, Mosnier T (2007) Biomécanique du Rachis. In: Elsevier (ed) Cahiers d’enseignement de la SOFCOT, pp 8–17
Nardi A, Tarantino U, Ventura L, Armotti P, Resmini G, Cozzi L, Tonini G, Ramazzina E, Rossini M (2011) Domino effect: mechanic factors role. Clin Cases Miner Bone Metab 8:38–42
Amabile C, Le Huec JC, Skalli W (2016) Invariance of head–pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J. https://doi.org/10.1007/s00586-016-4830-8
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Vital JM, Senegas J (1986) Anatomical bases of the study of the constraints to which the cervical spine is subject in the sagittal plane. A study of the center of gravity of the head. Surg Radiol Anat 8:169–173
Amabile C, Pillet H, Lafage V, Barrey C, Vital JM, Skalli W (2016) A new quasi-invariant parameter characterizing the postural alignment of young asymptomatic adults. Eur Spine J 25:3666–3674. https://doi.org/10.1007/s00586-016-4552-y
Morvan G, Mathieu P, Vuillemin V, Guerini H, Bossard P, Zeitoun F, Wybier M (2011) Standardized way for imaging of the sagittal spinal balance. Eur Spine J 20(Suppl 5):602–608. https://doi.org/10.1007/s00586-011-1927-y
Faro FD, Marks MC, Pawelek J, Newton PO (2004) Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2284–2289
Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J. https://doi.org/10.1007/s00586-016-4485-5
Le Huec JC, Demezon H, Aunoble S (2015) Sagittal parameters of global cervical balance using EOS imaging: normative values from a prospective cohort of asymptomatic volunteers. Eur Spine J 24:63–71. https://doi.org/10.1007/s00586-014-3632-0
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL (ed) Pediatric spine: principles and practice. Raven Press, New York, pp 480–481
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Le Huec, JC., Richards, J., Tsoupras, A. et al. The mechanism in junctional failure of thoraco-lumbar fusions. Part I: Biomechanical analysis of mechanisms responsible of vertebral overstress and description of the cervical inclination angle (CIA). Eur Spine J 27 (Suppl 1), 129–138 (2018). https://doi.org/10.1007/s00586-017-5425-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5425-8