Abstract
Purpose
Because previous studies have not focused on postoperative cervical collapse, the purpose of the present study was to introduce the overloaded vertebral body (OVB) phenomenon following multilevel zero-profile anterior cervical discectomy and fusion (ACDF) as well as to investigate its effects on radiographic outcomes.
Methods
We conducted a retrospective study involving patients who underwent ACDF. A total of 55 patients were included in the analysis, including 110 OVB and 110 non-OVB. The evaluated vertebral parameters included the vertebral cross-sectional area (CSA), wedge angle (WA), vertebral height [anterior (AH) and posterior (PH)] and anterior–posterior vertebral diameter [upper (UD) and lower (LD)].
Results
The CSA and WA were significantly lower in the OVB group than in the non-OVB group at 3, 6, and 12 months after surgery as well as at the final follow-up (p < 0.01). The AH of the OVB group was significantly lower at 3, 6, and 12 months after surgery as well as at the final follow-up compared to 1 week after surgery (p < 0.01).
Conclusions
OVB, a new phenomenon following multilevel ACDF, is defined as the cervical vertebral body located in the middle of the surgical segments in multilevel anterior cervical spine surgery. Statistical analysis of vertebral parameters, including CSA, WA, AH, PH, UD, and LD, showed that OVB occurs mainly at the anterior edge of the vertebra and that its largest radiographic manifestation is the loss of height at the anterior edge of the vertebra in the early postoperative period.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Aging is a serious worldwide problem, and as patients age, they develop cervical degenerative disc disease (CDDD) [1, 2]. The cervical spine is complex as it allows a great range of motion, and its main function is to support the weight of the head. However, CDDD causes compression of radiculopathy and/or myelopathy symptoms, which can cause neck discomfort, radiating upper extremity pain, numbness, and decreased muscle strength, reducing the patient's ability to perform daily activities and even leading to paralysis [3, 4]. Anterior cervical discectomy and fusion (ACDF) is an effective surgical option for the treatment of multilevel degenerative disc disease. It has been reported that multilevel ACDF with anterior mini-plates has some biomechanical advantages over conventional long fixation, such as reducing the occurrence of postoperative dysphagia and preserving more adjacent segment range of motion (ROM), resulting in a lower risk of adjacent segment degeneration (ASD) [5, 6].
Although multilevel ACDF is a common procedure, the potential complications associated with anterior surgery are not negligible, especially loss of segmental angle (SA) [7]. It has been widely accepted that cervical lordosis plays an important role in maintaining sagittal head and spinal balance [8]. Compromise on this lordotic curvature of the cervical spine, such as hypolordosis or kyphosis, is usually associated with neck pain, disability, and cervical disc degeneration [9]. In contrast, several retrospective studies have shown that a significant decrease in SA can be observed after multilevel ACDF [10, 11]. There are many speculative reasons for this occurrence, including osteoporosis, blood supply, damage to the endplate, and stress concentration [12, 13].
In the present study, we observed the uniqueness through the vertebral parameters and vertebral ratios after multilevel ACDF surgery with Zero-P fusion cage, which may explain the loss of cervical curvature. Due to the distinctive characteristics, we defined the cervical vertebra located in the middle of the surgical segments in multilevel zero-profile anterior cervical spine surgery as overloaded vertebra (OV), indicating that the upper and lower segments of OV are operated on. This study suggests that the primary changes occur in the vertebral body, so the main focus of this research is on overloaded vertebral body (OVB). To our knowledge, few studies have reported on postoperative vertebral conditions in multilevel ACDF. The purpose of the present study was to introduce the OVB phenomenon following multilevel ACDF as well as to investigate its effects on radiographic outcomes.
Materials and methods
Participants and procedure selection
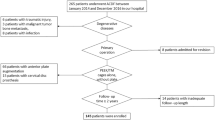
We conducted a retrospective study involving patients with three-level CDDD who underwent ACDF with Zero-P or Zero-P VA implants (Synthes, Oberdorf, Switzerland) at our institution between March 2015 and June 2021. The vertebrae in the middle of the operated segment of the patients with three-level ACDF were considered the OVB group, and the upper and lower vertebrae of the OVB were considered the non-OVB group. A total of 55 patients were included in the analysis, including 110 OVB and 110 non-OVB (Fig. 1). The inclusion criteria were as follows: (1) diagnosis of spondylotic radiculopathy or myelopathy; (2) refractory to conservative treatment for at least 6 weeks; (3) confirmation of the lesion area by clinical symptoms and imaging (computed tomography, magnetic resonance imaging, and radiology); and (4) surgery at three levels between C3 and C7. The exclusion criteria were as follows: (1) previous cervical spine surgery; (2) presence of cervical stenosis, osteoporosis, tumor, or infection; (3) history of trauma or deformity; and (4) follow-up < 12 months. Ethical approval for this study was granted by the Ethics Committee of our institution. All participants provided informed consent for the analysis of their clinical data.
Surgical technique
All anterior fusions were performed using the Smith-Robinson technique and a right-sided approach by the same surgeon. All patients underwent preoperative tracheoesophageal advancement training to prevent postoperative sputum and swallowing difficulties. After confirming and exposing the appropriate vertebra level, a Caspar retractor was used, and the disc material was removed. The endplate cartilage was scraped using a spatula or high-speed electric drill to prepare the endplate for bone grafting. The posterior longitudinal ligament, osteophytes, and other compressed elements were removed to ensure adequate dural and neural decompression. After measuring intervertebral height and width, an appropriate tricalcium phosphate-filled Zero-P or Zero-P VA implant was inserted with an implant scaffold/targeting device. C-arm fluoroscopy was performed to verify the correct position of the implant (Fig. 2). Finally, the incision was closed after insertion of the drainage tube.
Data collection
The data were collected at 1 week, 3 months, 6 months, and 12 months postoperatively as well as at the final follow-up. Perioperative parameters, including the gender, age, BMI, operative segment, operative time and blood loss, were collected.
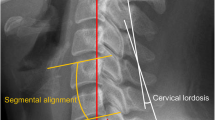
Radiological evaluation
Cervical parameters were measured on lateral radiographs. All images were transferred to a picture archiving and communication system (PACS), and they were measured directly using the built-in tools of the PACS workstations. The following cervical parameters were evaluated: (1) vertebral cross-sectional area (CSA); (2) wedge angle (WA); (3) anterior vertebral height (AH); (4) posterior vertebral height (PH); (5) upper anterior–posterior vertebral diameter (UD); and (6) lower anterior–posterior vertebral diameter (LD).
CSA and WA were defined as the areas enclosed by the upper and lower endplates as well as the anterior and posterior edge of the vertebra and the angle of the tangent line connecting the upper and lower endplates of the vertebra, respectively. For WA, positive values represent lordosis, whereas negative values indicate kyphosis. Vertebral height was defined as the linear distance from the upper endplate of the vertebra to the lower endplate of the vertebra, and it was divided into AH and PH. Anterior–posterior vertebral diameter was defined as the linear distance from the anterior edge of the vertebra to the posterior edge of the vertebra, and it was divided into UD and LD. By measuring the height of the anterior edge of the vertebra in the OVB group at the final follow-up and 1 week postoperatively, the degree of vertebral height loss was classified as < 1/5, 1/5–1/3, or > 1/3 [14]. The wedge ratio (WR) was calculated using the following formula: WR = AH/PH × 100%. The extent of vertebral deformity (V-deformity) was presented as WR and graded from 0 to 3 according the grading presented by Genant et al. [15]: grade 0, normal (WR, ≥ 80%); grade 1, mildly deformed (WR, 75% – < 80%); grade 2, moderately deformed (WR, 60 to < 75%); and grade 3, severely deformed (WR, < 60%) (Fig. 3).
Schematic diagram of the parameters. X-rays show several parameters measured in this investigation. CSA Vertebral cross-sectional area, AH Anterior vertebral height, PH Posterior vertebral height, UD Upper anterior–posterior vertebral diameter, LD Lower anterior–posterior vertebral diameter, WA Wedge angle
Statistical analysis
All statistical analyses were performed using SPSS (version 24.0, SPSS, Chicago, IL, USA). Continuous variables are presented as the mean ± standard deviation (SD), and categorical variables are presented as the number of cases. A paired t test was used to compare the cervical parameters after surgery. Student’s t test or the Mann‒Whitney U test was used to compare continuous variables depending on the normality of the data. A chi-square test or Fisher’s exact test was used to analyze categorical data. Statistical significance was defined as p < 0.01.
Results
Demographic and surgical data
A total of 55 patients were included in the analysis according to the inclusion and exclusion criteria, including 110 vertebrae in the OVB group and 110 vertebrae in the non-OVB group. The mean age of the 55 patients was 58.87 years ± 11.00 years, and the mean follow-up time was 26.78 months ± 16.76 months. The study details are shown in Table 1.
Radiological outcomes
Compared to the non-OVB group, the CSA was significantly lower in the OVB group at 3, 6, and 12 months after surgery as well as at the final follow-up (p < 0.01). In the OVB group, the CSA was significantly lower at 3, 6, and 12 months after surgery as well as at the final follow-up compared to 1 week after surgery (p < 0.01). The WA was significantly lower in the OVB group than in the non-OVB group at 3, 6, and 12 months after surgery as well as at the final follow-up (p < 0.01). The WA was significantly lower in the non-OVB and OVB groups at 3 months and 12 months after surgery as well as at the final follow-up compared to at 1 week after surgery (p < 0.01). Compared to 1 week after surgery, the WA was significantly lower in the OVB group at 6 months after surgery (p < 0.01). In addition, there was a significant reduction in the CSA and WA in the OVB group compared to the non-OVB group at the final follow-up (Table 2 and Fig. 4).
Compared to the non-OVB group, the AH and PH were significantly decreased at 1 week, 3 months, 6 months, and 12 months after surgery as well as at the final follow-up in the OVB group (p < 0.01). Compared to the immediate postoperative period (1 week after surgery), a decrease in AH was observed at all subsequent follow-ups (3 months, 6 months, and 12 months after surgery as well as at the final follow-up) in the OVB group (p < 0.01). Compared to 1 week after surgery, the PH was significantly higher at 6 months and 12 months after surgery as well as at the final follow-up in the OVB and non-OVB groups (p < 0.01). In addition, there was a statistically significant increase in the UD and LD only at 12 months after surgery compared to 1 week after surgery in the OVB and non-OVB groups (Tables 3 and 4, Fig. 4).
Radiological analysis of vertebral cross-sectional area, wedge angle, anterior vertebral height, posterior vertebral height, upper anterior–posterior vertebral diameter, and lower anterior–posterior vertebral diameter in patients. OVB Overloaded vertebral body, CSA Vertebral cross-sectional area, WA Wedge angle, AH Anterior vertebral height, PH Posterior vertebral height, UD Upper anterior–posterior vertebral diameter, LD Lower anterior–posterior vertebral diameter. *Significance on parameters between Non-OVB and OVB (p < 0.01). # Significance on parameters between Po-1w (p < 0.01)
According to vertebral height loss, there were 93 cases (84.5%) with < 1/5 height loss, 15 cases (13.6%) with 1/5–1/3 height loss, and 2 case (1.8%) with > 1/3 height loss at 3 months after surgery, while there were 68 cases (61.8%) with < 1/5 height loss, 32 cases (29.1%) with 1/5–1/3 height loss, and 10 cases (9.1%) with a height loss > 1/3 at the final follow-up. The number of vertebrae with a severe degree of height loss at the final follow-up was higher than that at 1 week after surgery. Similar results were obtained for the V-deformity as follows: there were 96 cases (87.3%) with grade 0, 11 cases (10.0%) with grade 1, 3 case (2.7%) with grade 2, and 0 cases (0.0%) with grade 3 at 1 week after surgery; and there were 26 cases (23.6%) with grade 0, 21 cases (19.1%) with grade 1, 51 cases (46.4%) with grade 2, and 12 cases (10.9%) with grade 3 at the final follow-up (Table 5).
Discussion
ACDF is a widely accepted surgical procedure for the treatment of multilevel CDDD [16,17,18]. Multilevel ACDF is effective in restoring interbody height and physiological curvature of the cervical spine as well as reestablishing stability of the cervical spine, resulting in a lower risk of structural failure and adjacent segment degeneration [19, 20]. With an aging population, the presence of cervical kyphosis, and the recognition of the importance of cervical sagittal alignment and maintaining sagittal balance, the consideration and performance of multilevel ACDF continues to improve. However, with the increasing utilization of multilevel ACDF surgery and the increase in follow-up, complications, such as ASD, dysphagia, subsidence, implant failure, and hoarseness, after the procedure have emerged [21]. Lin et al. [13] reported early postoperative middle cervical vertebral body collapse in 4 out of 27 cases after two-level ACDF, but they did not provide a specific definition of this occurrence nor provide a comprehensive parametric measurement and statistical analysis. In this study, we defined the cervical vertebral body located in the middle of the surgical segments in multilevel anterior cervical spine surgery as the OVB. By comparing radiographic findings between OVB and non-OVB, we identified a new phenomenon of OVB that may impact the prognosis after ACDF surgery using the Zero-P fusion cage (Fig. 5).
Installation according to the severity of vertebral deformity. Yellow arrows indicate vertebrae with significant morphological changes. A A middle-aged female patient with C4/5, C5/6, and C6/7 ACDF had all C4/5, C5/6, and C6/7 fused at the final follow-up. The AH of the superior OVB decreased significantly from 1.60 cm at 1 week postoperatively to 1.41 cm at the final follow-up, and there was significant bone resorption at the anterior edge. B A middle-aged male patient with C4/5, C5/6, and C6/7 ACDF. The AH of the superior OVB decreased significantly from 1.60 cm at 1 week postoperatively to 1.21 cm at the final follow-up; the AH of the inferior OVB decreased significantly from 1.46 cm at 1 week to 1.11 cm at the final follow-up. C A middle-aged female patient with C4/5, C5/6, and C6/7 ACDF had C5/6 and C6/7 fused at the final follow-up. The AH of the inferior OVB decreased significantly from 1.28 cm at 1 week postoperatively to 0.79 cm at the final follow-up
In the present study, three-level ACDF resulted in a significantly lower CSA and WA in the OVB group than in the non-OVB group at the postoperative follow-ups, which indicated that OVB does exist after multilevel ACDF and is mainly manifested by morphological changes in the vertebra. Moreover, the measurement of vertebral imaging parameters showed that the OVB was more likely to suffer with the reduction of vertebral height in multilevel ACDF. For osteoporotic vertebral endplate and cortical fractures, approximately 60–70% showed compression of the cervical anterior edge on imaging, and 11.4% of vertebral fractures had > 1/3 loss of vertebral height [22]. Studies have shown that the anterior vertebral wall is a biomechanically weak site [23]. For the AH, In the OVB group, the AH was significantly lower at 3 months, 6 months, and 12 months after surgery as well as at the final follow-up compared to 1 week after surgery, indicating a significant decrease in AH over time in OVB. In contrast, there were no statistically significant differences in the postoperative follow-up data for the other vertebrae, suggesting that the occurrence of this phenomenon in OVB is concentrated at the anterior edge of the vertebra with physiological weakness. In addition, combining the two classifications of vertebral ratios indicated that a large percentage of vertebral anterior edge reduction was present at the final follow-up in the early postoperative period.
The phenomenon of OVB investigated in the present study was different from the previously studied subsidence and collapse. Lu et al. [24] conducted a meta-analysis that included 626 patients, and they reported that multilevel ACDF with anterior mini-plates has a higher risk of postoperative subsidence than conventional long fixation. Noordhoek et al. [25] showed that the mean incidence of cage subsidence after ACDF surgery with Zero-P fusion cage is 21% (range 0 to 83%). Subsidence and collapse are similar in that they both result in loss of disc height, loss of segmental lordosis, and a decrement of neural foramen dimension after ACDF [26, 27]. Subsidence is mostly the sinking of a body with a higher modulus of elasticity (e.g., graft, cage, and spacer) into a body with a lower modulus of elasticity (e.g., vertebra), and collapse is primarily the compression of a body with a similar or lower modulus of elasticity (e.g., autologous or allograft bone) by a surrounding body with a similar or higher modulus of elasticity (e.g., vertebra), resulting in its own compression [28, 29]. These previous two studies concentrated more on the condition of the intervertebral space and involved fewer morphological changes in the vertebra, indicating that OVB is a new phenomenon that is fundamentally different from subsidence and collapse.
Previous studies have reported that increased intraoperative wear on the endplate may lead to higher rates of surgical failure or at least greater subsidence and collapse, especially in patients with osteoporosis and poor bone quality [28]. In contrast, the present findings indicated that it may be mainly due to bone remodeling after microdamage of the endplate bone caused by the surgical grinding of the endplate. This process may have been influenced by the altered biomechanical environment of the operated segment as the cervical spine was in anterior convexity and the anterior edge of the vertebra was under less force. According to Wolff's law, bone resorption occurred. Because the multiplate multiscrew model shares more load compared to the single-plate model, multiple screws will reduce the stress on the anterior plate [20]. The bone portion of the vertebra may have received destructive stresses due to screwing in multiple screws, which led to the collapse of the vertebra. Therefore, the postoperative vertebral morphological changes caused by the different surgical segments are different, and it is crucial to reduce the wear on the endplate and the use of screws during surgery. A biomechanical analysis of customized cages conforming to the endplate morphology may reduce the risk of stress shielding and the occurrence of subsidence [2, 30]. Preoperative customization of the vertebral cage by evaluating and measuring the morphology of the vertebra at different segments may be more consistent with human biomechanics and thus reduce the incidence of morphological change of OVB.
The present study had several limitations. First, the present study was a single-center retrospective study with a small sample size due to the small number of multilevel CDDD cases. Second, the present study did not analyze the clinical outcomes after three-segment ADCF. However, the present study was not designed to understand the efficacy of this procedure, which has been demonstrated in many other studies [31, 32]. Finally, the extended review period raises the possibility of varying vertebral changes among patients who underwent the intervention during this timeframe. Therefore, a multicenter prospective study should be performed to further confirm the present findings.
Conclusions
The present study demonstrated that OVB exists and is defined as the cervical vertebral body located in the middle of the surgical segments in multilevel anterior cervical spine surgery. Statistical analysis of vertebral parameters, including CSA, WA, AH, PH, UD, and LD, showed that OVB occurs mainly at the anterior edge of the vertebra and that its largest radiographic manifestation is the loss of height at the anterior edge of the vertebra at 3, 6 months postoperatively.
Availability of data and materials
Datasets are available from the corresponding author on a reasonable request.
Abbreviations
- CDDD:
-
Cervical degenerative disc disease
- ACDF:
-
Anterior cervical discectomy and fusion
- ROM:
-
Range of motion
- ASD:
-
Adjacent segment degeneration
- SA:
-
Segmental angle
- OV:
-
Overloaded vertebra
- OVB:
-
Overloaded vertebral body
- PACS:
-
Picture archiving and communication system
- CSA:
-
Vertebral cross-sectional area
- WA:
-
Wedge angle
- AH:
-
Anterior vertebral height
- PH:
-
Posterior vertebral height
- UD:
-
Upper anterior–posterior vertebral diameter
- LD:
-
Lower anterior–posterior vertebral diameter
- WR:
-
Wedge ratio
- SD:
-
Standard deviation
- BMI:
-
Body mass index
References
Fehlings MG, et al. The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery. 2015;77(Suppl 4):S1-5. https://doi.org/10.1227/NEU.0000000000000953.
Tsuang FY, Li MJ, Chu PH, Tsou NT, Sun JS. Mechanical performance of porous biomimetic intervertebral body fusion devices: an in vitro biomechanical study. J Orthop Surg Res. 2023;18:71. https://doi.org/10.1186/s13018-023-03556-4.
Tian X, et al. Treatment of three-level cervical spondylotic myelopathy using ACDF or a combination of ACDF and ACCF. Front Surg. 2022;9:1021643. https://doi.org/10.3389/fsurg.2022.1021643.
Nunna RS, et al. Anterior vs posterior approach in multilevel cervical spondylotic myelopathy: a nationwide propensity-matched analysis of complications, outcomes, and narcotic use. Int J Spine Surg. 2022;16:88–94. https://doi.org/10.14444/8198.
Shen Y, Du W, Wang LF, Dong Z, Wang F. Comparison of zero-profile device versus plate-and-cage implant in the treatment of symptomatic adjacent segment disease after anterior cervical discectomy and fusion: a minimum 2-year follow-up study. World Neurosurg. 2018;115:e226–32. https://doi.org/10.1016/j.wneu.2018.04.019.
Hua W, et al. Adjacent segment biomechanical changes after one- or two-level anterior cervical discectomy and fusion using either a zero-profile device or cage plus plate: a finite element analysis. Comput Biol Med. 2020;120: 103760. https://doi.org/10.1016/j.compbiomed.2020.103760.
Wewel JT, et al. Fusion rate following three- and four-level ACDF using allograft and segmental instrumentation: a radiographic study. J Clin Neurosci. 2019;62:142–6. https://doi.org/10.1016/j.jocn.2018.11.040.
Azimi P, Yazdanian T, Benzel EC, Hai Y, Montazeri A. Sagittal balance of the cervical spine: a systematic review and meta-analysis. Eur Spine J. 2021;30:1411–39. https://doi.org/10.1007/s00586-021-06825-0.
Scheer JK, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013;19:141–59. https://doi.org/10.3171/2013.4.SPINE12838.
Michalopoulos GD, et al. Hybrid surgery: a comparison of early postoperative outcomes between anterior cervical discectomy and fusion and cervical disc arthroplasty. J Neurosurg Spine. 2022;36:575–84. https://doi.org/10.3171/2021.7.SPINE21478.
Huang K, et al. Classification of three-level hybrid surgery for the treatment of cervical degenerative disc disease: a retrospective study of 108 patients. BMC Surg. 2022;22:179. https://doi.org/10.1186/s12893-022-01627-7.
Li T, et al. Can zero-profile cage maintain the cervical curvature similar to plate-cage construct for single-level anterior cervical diskectomy and fusion? World Neurosurg. 2020;135:e300–6. https://doi.org/10.1016/j.wneu.2019.11.153.
Lin H, et al. A new potential complication in 2-level anterior cervical discectomy and fusion with zero-profile devices: collapse of the middle cervical vertebra. World Neurosurg. 2022;165:e175–90. https://doi.org/10.1016/j.wneu.2022.05.139.
Wang YXJ. A modified semi-quantitative (mSQ) grading scheme for osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg. 2019;9:146–50. https://doi.org/10.21037/qims.2019.02.04.
Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–48. https://doi.org/10.1002/jbmr.5650080915.
Buttermann GR. Anterior cervical discectomy and fusion outcomes over 10 years: a prospective study. Spine. 2018;43:207–14. https://doi.org/10.1097/BRS.0000000000002273.
Vleggeert-Lankamp CLA, et al. The NECK trial: effectiveness of anterior cervical discectomy with or without interbody fusion and arthroplasty in the treatment of cervical disc herniation; a double-blinded randomized controlled trial. Spine J. 2019;19:965–75. https://doi.org/10.1016/j.spinee.2018.12.013.
Epstein NE. A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int. 2019;10:100. https://doi.org/10.25259/SNI-191-2019.
Pereira BA, Heller JE, Lehrman JN, Sawa AGU, Kelly BP. Biomechanics of circumferential cervical fixation using posterior facet cages: a cadaveric study. Neurospine. 2021;18:188–96. https://doi.org/10.14245/ns.2040552.276.
Huang W, et al. Comparative analysis of the biomechanics of anterior cervical discectomy and fusion with multiple segmental plates fixation versus single multilevel plate fixation: a finite element study. BMC Musculoskelet Disord. 2022;23:848. https://doi.org/10.1186/s12891-022-05796-7.
Chen Z, et al. Use of zero-profile device for contiguous three-level anterior cervical discectomy and fusion: comparison with cage and plate construct. J Neurosurg Spine. 2021. https://doi.org/10.3171/2020.11.SPINE201319.
Wang XR, Xu FR, Huang QL, Wang YXJ. Radiological features of traumatic vertebral endplate fracture: an analysis of 194 cases with 263 vertebral fractures. Chin Med J (Engl). 2020;133:2696–702. https://doi.org/10.1097/CM9.0000000000000919.
Deng M, et al. Osteoporotic vertebral fracture prevalence in elderly Chinese men and women: a comparison of endplate/cortex fracture-based and morphometrical deformity-based methods. J Clin Densitom. 2019;22:409–19. https://doi.org/10.1016/j.jocd.2017.11.004.
Lu Y, et al. Does zero-profile anchored cage accompanied by a higher postoperative subsidence compared with cage-plate construct? A meta-analysis. J Orthop Surg Res. 2020;15:189. https://doi.org/10.1186/s13018-020-01711-9.
Noordhoek I, Koning MT, Jacobs WCH, Vleggeert-Lankamp CLA. Incidence and clinical relevance of cage subsidence in anterior cervical discectomy and fusion: a systematic review. Acta Neurochir (Wien). 2018;160:873–80. https://doi.org/10.1007/s00701-018-3490-3.
Woo JB, et al. Risk factors of allogenous bone graft collapse in two-level anterior cervical discectomy and fusion. J Korean Neurosurg Soc. 2019;62:450–7. https://doi.org/10.3340/jkns.2019.0008.
Kim C, et al. Two-year clinical and radiographic outcomes of expandable interbody spacers following minimally invasive transforaminal lumbar interbody fusion: a prospective study. Int J Spine Surg. 2020;14:518–26. https://doi.org/10.14444/7068.
Karikari IO, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech. 2014;27:1–10. https://doi.org/10.1097/BSD.0b013e31825bd26d.
Pinter ZW, et al. Risk factors for allograft subsidence following anterior cervical discectomy and fusion. World Neurosurg. 2023;170:e700–11. https://doi.org/10.1016/j.wneu.2022.11.109.
Sun B, et al. Biomechanical analysis of customized cage conforming to the endplate morphology in anterior cervical discectomy fusion: a finite element analysis. Heliyon. 2023;9:e12923. https://doi.org/10.1016/j.heliyon.2023.e12923.
Joo PY, et al. Clinical outcomes following one-, two-, three-, and four-level anterior cervical discectomy and fusion: a national database study. Spine J. 2022;22:542–8. https://doi.org/10.1016/j.spinee.2021.11.002.
Li W, et al. A randomized controlled study of two different fixations in anterior cervical discectomy of multilevel cervical spondylotic myelopathy. J Orthop Surg (Hong Kong). 2022;30:10225536221118600. https://doi.org/10.1177/10225536221118601.
Acknowledgements
We thank the editors and reviewers for helping to process our manuscript.
Funding
National Natural Science Foundation of China (81902190), the Foundation of Science and Technology Department of Sichuan Province (2023NSFSC1741), the Foundation Health Commission of Sichuan Province (21PJ039), and 1.3.5 project for Postdoctoral Foundation of West China Hospital of Sichuan University (2023HXBH080). There were no relevant financial activities outside the submitted work.
Author information
Authors and Affiliations
Contributions
SC wrote the original draft. BW contributed in the conceptualization, methodology, validation, and investigation; provided the resources; reviewed and edited the manuscript; and did the supervision. KH took part in the conceptualization, formal analysis, and validation and provided the resources. HL and TW provided the resources and did the supervision and funding acquisition. MY and JH provided the resources and did the supervision. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (No. 2019-567) and was conducted following the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, S., Huang, K., Liu, H. et al. Overloaded vertebral body: a unique radiographic phenomenon following multilevel anterior cervical discectomy and fusion. J Orthop Surg Res 18, 879 (2023). https://doi.org/10.1186/s13018-023-04365-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04365-5