Abstract
Purpose
To evaluate the value of blood lactate value in predicting postoperative mortality (primary outcome), duration of ventilation, and length of stay in an intensive care unit (ICU) and hospital (secondary outcomes).
Methods
We performed a prospective observation study on 1,820 consecutive patients undergoing open heart surgery in a tertiary university medical center. Blood lactate levels were obtained from patients on admission to the cardiac surgical ICU and measured serially.
Results
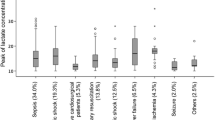
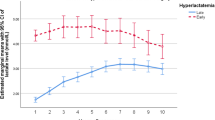
All patients were divided into three groups according to their maximum blood lactate levels: group I (normolactatemia, lactate ≤2.2 mmol/l), 332 patients; group II (mild hyperlactatemia, lactate 2.2–4.1 mmol/l), 1,054 patients; and group III (severe hyperlactatemia, lactate ≥4.4 mmol/l), 434 patients. Maximum blood lactate levels ≥4.4 mmol/l during the first 10 h post admission were associated with prolonged ventilation time, longer ICU stay, and increased mortality (P < 0.001).
Conclusions
Hyperlactatemia is common after cardiac surgery. Maximal lactate threshold ≥4.4 mmol/l in the first 10 h after operation accurately predicts postoperative mortality.
Similar content being viewed by others
Introduction
Hyperlactatemia, a well-recognized marker of hypoperfusion, has been associated with mortality in various clinical settings and is a common metabolic disturbance following cardiac surgery. Postoperative blood lactate levels are associated with outcome after both adult [1, 2] and pediatric cardiac surgery [3, 4]. Postcardiac surgery outcome is determined by the preoperative status of the patient, as well as by technical factors in the operating room and intensive care unit (ICU). The most common methods of preoperative risk stratification are clinical scoring systems such as EuroSCORE [5] and Parsonnet [6] score. However, morbidity and mortality are also influenced by surgical and anesthetic techniques, including time on cardiopulmonary bypass (CPB), completeness of revascularization, efficacy of myocardial protection, hemodynamic management and unforeseen events in the operating room. Patient prognosis upon arrival at the ICU may differ from the preoperative prognosis. We hypothesized that hyperlactatemia after surgery may be connected with intraoperative problems, and therefore decided to evaluate the impact of early postoperative lactate levels on patient outcome.
The aim of our study was to evaluate whether postoperative blood lactate levels are associated with mortality, ventilation time, and prolonged ICU and hospital stay.
Materials and methods
This prospective observational study was approved by the local ethics committee and received a waiver for informed consent. All patients who underwent cardiac surgery during 36 months between 1 August 2009 and 31 July 2011 at our tertiary-care, university-affiliated medical center were enrolled into the study.
Patients undergoing off-pump cardiac surgery and patients with previous liver disease were excluded from the study.
All 1,820 study patients received a standard anesthetic protocol: 5–10 mg diazepam was used for premedication, and anesthesia was induced with 10–15 μg/kg fentanyl and 0.01–0.02 mg/kg midazolam; 0.1 mg/kg pancuronium was given to facilitate endotracheal intubation. The lungs were ventilated with an oxygen/air mixture to maintain normocapnia. Anesthesia was maintained with isoflurane, fentanyl, and midazolam. The total fentanyl and midazolam doses were 25.8 ± 12.9 μg/kg and 0.02 ± 0.03 mg/kg, respectively. Monitoring included a five-lead electrocardiogram, pulse oximetry, nasal temperature, invasive arterial pressure, and central venous pressure. A pulmonary artery catheter was also used in patients with heart failure or pulmonary hypertension. All patients undergoing valve procedures were assessed by transesophageal echocardiography.
Before initializing CPB, systemic heparinization was accomplished with a heparin dose of 400 U/kg. Additional heparin was administered during CPB to maintain an activated coagulation time of >480 s. CPB was maintained at a cardiac index of 2.4 l/min/m2 with a Sarns heart–lung roller pump (Terumo CV Systems, Ann Arbor, MI, USA). Only the membrane oxygenator (Jostra-Bentley, Irvine, CA, USA) was heparin coated; circuit tubing and arterial filter (Jostra-Bentley) were without heparin. The pump prime consisted of 1,000 ml lactated Ringer’s solution and 100 ml 20% mannitol, to which 10,000 U heparin was added. The mean arterial pressure was maintained between 60 and 80 mmHg using boluses of phenylephrine as required. Serum glucose levels were controlled with intermittent administration of insulin. Hematocrit was maintained at 22% with the administration of packed red blood cells as necessary. Epsilon-aminocaproic acid was administered in doses of 50–60 mg/kg to all patients. Cardiac arrest was achieved by anterograde or retrograde blood cardioplegia. Topical cooling was not used, and core temperature was around 34.5°–35°C. Before discontinuation of CPB, patients were warmed to 37°C, and returned to the cardiothoracic ICU while still intubated, where they were managed by an attending intensivist or surgical fellow.
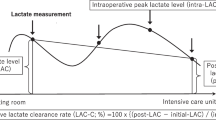
Standard postoperative care consisted of mechanical ventilation in the assist-control mode at 8–10 ml/kg, 10–12 breaths/min, positive end-expiratory pressure of 4–5 cmH2O; warm air heaters maintained normothermia. Sedation was provided with propofol in a dose of 0.5–1.0 mg/kg and analgesia with morphine boluses as required. Cardioactive drugs such as epinephrine, norepinephrine, dobutamine, or milrinone were administered according to the hemodynamic status of the patient. As part of postoperative management, blood lactate concentrations were measured immediately after admission to the ICU and every 1–3 h thereafter during the first 24 postoperative h, or up to ICU discharge, if patients were released early from the ICU. Arterial blood gas analyses and arterial lactate concentrations (normal lactate value, 2.2 mmol/l) were performed using a blood gas analyzer (Rapidlab 864; Chiron Diagnostics, Bayer, Leverkusen, Germany).
Weaning from the ventilator was commenced in the presence of hemodynamic stability (without or decreasing use of cardioactive drugs), absence of significant bleeding (100 ml/h), absence of significant arrhythmias, adequate urine output (1 ml/kg/h), and oxygen saturation of 95% with FiO2 0.50.
Data collection
The following perioperative variables were obtained: sex, presence of congestive heart failure [New York Heart Association (NYHA) class III–IV], need for intraaortic balloon pump, presence of diabetes mellitus, presence of chronic obstructive pulmonary disease, presence of renal failure, left ventricular function, priority of surgery (elective or urgent), type of surgery, and duration of cross-clamping and CPB. Renal failure was defined as creatinine level >1.4 mg/dl. Postoperative variables included the duration of mechanical ventilation, duration of initial ICU stay, volume of bleeding, need for revision, inotropic support (epinephrine, norepinephrine, dobutamine) during the initial 24-h period, postoperative renal failure, and hospital mortality.
Statistical analysis
Values are expressed as number of patients (percentage) or mean ± 1 SD. Numeric variables were analyzed with analysis of variance (ANOVA) and post hoc tests. We compared preoperative, operative, and postoperative parameters. Analysis was performed for each parameter in each of the three groups, and patients were divided by their peak postoperative lactate values. Following, we performed uni- and multivariate analyses based on the Cox proportional hazards regressions model. The univariate parameters with P < 0.05 were used in the multivariate analyses using backward selection. The variables were tested for interaction and the assumption for proportional hazards was verified. P < 0.05 was considered statistically significant. Statistical analyses were performed with SPSS version 16.0 (SPSS, Chicago, IL, USA).
Results
The study comprised 1,820 consecutive patients undergoing open heart surgery. Analysis of postoperative lactate values revealed two major patterns: 1,488 (81.8%) patients with elevated postoperative lactate levels and 332 (18.2%) patients demonstrating lactate levels within normal range. Postoperative peak lactate levels were seen after 3.36 ± 3.13 h; 7.34 ± 6.56 h elapsed before lactate values returned to within normal range after reaching peak levels.
All patients were divided into three groups according to peak blood lactate levels: group I (normolactatemia, lactate ≤2.2 mmol/l), 332 patients; group II (mild hyperlactatemia, lactate 2.21–4.4 mmol/l, 1,054 patients; and group III (severe hyperlactatemia, lactate ≥4.4 mmol/l), 434 patients. Preoperative and intraoperative data are presented in Table 1. Postoperative data are presented in Table 2. There were no significant statistical differences between the groups in the following parameters: diabetes, chronic obstructive pulmonary disease, number of active smokers, preoperative functional capacity as average and in each NYHA class, preoperative renal failure, priority for surgery (elective, during hospitalization, urgent, or emergent) and hospital stay (days), during the postoperative period.
There was a significant statistical difference in the following parameters: sex, logistic and standard EuroSCORE, type of surgery, cardiopulmonary bypass time (min), cross-clamp time (min), bleeding (ml), use of β-agonist (epinephrine, norepinephrine, dobutamine), postoperative renal failure, ICU length of stay (days), ventilation time (h), and hospital mortality rate between groups I and II compared with group III. Overall, postoperative mortality was 2.36% (43 patients). At proportional hazards regressions analysis, the following parameters were univariate predictors of in-hospital mortality (Table 3): lactate >4.4 mmol/l, congestive heart failure (NYHA III–IV), severe left ventricular (LV) dysfunction [ejection fraction (EF) <30%), and preoperative renal failure (serum creatinine >1.4 mg/dl). At multivariate analysis (Table 4) only lactate >4.4 mmol/l and congestive heart failure (NYHA III–IV) were still independent predictors of in-hospital mortality.
Discussion
Blood lactate levels are simple to obtain, and results are quickly available in most institutions. An increase in blood lactate levels could result from increased production or decreased clearance, or a combination of both processes. The nature of elevated blood lactate levels during and after cardiac surgery is still controversial. Tissue perfusion is at risk during cardiac surgery and in the immediate postoperative period. Takala et al. [7] suggest that hyperlactatemia after cardiac surgery is a sign of inadequate tissue perfusion of the hepatosplanchnic region. Perner et al. [8] found that increasing intraluminal lactate in the rectum during CPB indicates metabolic dysfunction of the intestinal mucosa. In contrast, Haisjackl et al. [9] and Braun et al. [10] demonstrated that cardiac surgery was not associated with deterioration in splanchnic oxygen delivery and hyperlactatemia, but a manifestation of systemic inflammatory response to CPB. Dixon et al. [11] found that marked prothrombotic response after CPB is associated with elevated lactate levels. Gasparovic et al. [12] maintain that the lungs are an additional possible source of lactate during CPB. Besides anaerobic glycolysis, increased aerobic glycolysis by catecholamine-stimulated Na+–K+ pump may account for hyperlactatemia after cardiac surgery [13]. However, in our study the number of patients receiving a catecholamine was similar in groups II and III.
Measurement of blood lactate levels is widely used to assess the adequacy of tissue perfusion. Experimental studies have clearly confirmed the relationship between tissue hypoxia and hyperlactatemia. Traditionally, hyperlactatemia in critically ill patients was interpreted as a marker of anaerobic metabolism resulting from inadequate oxygen supply [14]. Maillet et al. [1] found that hyperlactatemia, >3 mmol/l, occurs frequently (17.2–20.6%) after cardiac surgery. In our study, severe hyperlactatemia, >4.4 mmol/l, was observed in 26.6% of patients. Arnold et al. [15] and Shapiro et al. [16] support the employment of lactate levels >4 mmol/l to be a marker for severe tissue hypoperfusion and hence a predictor of mortality. Irrespective of the origin of increased blood lactate levels, hyperlactatemia in septic [17], trauma [18], and emergency department patients [15, 16] is always associated with unfavorable outcome, compared to similar patients with normal blood lactate levels. Several studies have demonstrated that hyperlactatemia in the early postoperative period following pediatric cardiac surgery [3, 4, 19–22] and adult cardiac surgery [1] is associated with an increased risk of mortality and morbidity. The link between tissue hypoperfusion and hyperlactatemia is evident. Studies of acute myocardial infarction, trauma, sepsis, and stroke have been translated into improved outcomes by earlier diagnosis and early treatment [23]. Recognition of abnormally high blood lactate levels might facilitate earlier and more effective intervention in the immediate postoperative period. Jones et al. [24] shows that among patients with septic shock, lactate-directed management is equivalent to management directed to normalize central venous oxygen saturation (ScvO2). Pölönen et al. [25] found that goal-oriented (lactate and ScvO2) therapy during the immediate postoperative period after cardiac surgery could decrease morbidity and reduce length of hospital stay. In our study, peak lactate values were seen after 3.4 ± 2.8 h postoperatively and decreased to normal range during the following 6.4 ± 5.7 h.
A serious limitation of our study was the lack of a specific goal-oriented protocol in our department. Patients were treated according to hemodynamic parameters and urine output, regardless of blood lactate levels.
Our results support the need for a large multicenter study using lactate-directed therapy in early postoperative hours after adult cardiac surgery.
Conclusions
Hyperlactatemia is common after cardiac surgery and may be a useful early-warning signal for further investigation. A maximal lactate threshold ≥4.4 mmol/l accurately predicts postoperative mortality in adult patients undergoing cardiac surgery with CPB. Hyperlactatemia is also significantly associated with prolonged ICU and hospital stay. Initial lactate levels, however, are poor predictors of mortality. Further studies are needed to establish a lactate-directed treatment protocol.
References
Maillet JM, Le Besnerais P, Cantoni M, Nataf P, Ruffenach A, Lessana A, Brodaty D. Frequency, risk factors, and outcome of hyperlactatemia after cardiac surgery. Chest. 2003;123:1361–6.
Ranucci M, De Toffol B, Isgrò G, Romitti F, Conti D, Vicentini M. Hyperlactatemia during cardiopulmonary bypass: determinants and impact on postoperative outcome. Crit Care. 2006;10(6):R167.
Cheung PY, Chui N, Joffe AR, Rebeyka IM, Robertson CM. Postoperative lactate concentrations predict the outcome of infants aged 6 weeks or less after intracardiac surgery: a cohort follow-up to 18 months. J Thorac Cardiovasc Surg. 2005;130:837–43.
Kalyanaraman M, DeCampli WM, Campbell AI, Bhalala U, Harmon TG, Sandiford P, McMahon CK, Shore S, Yeh TS. Serial blood lactate levels as a predictor of mortality in children after cardiopulmonary bypass surgery. Pediatr Crit Care Med. 2008;9:285–8.
Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16(1):9–131.
Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79(6 pt 2):I3–12.
Takala J, Uusaro A, Parviainen I, Ruokonen E. Lactate metabolism and regional lactate exchange after cardiac surgery. New Horiz. 1996;4:483–92.
Perner A, Jørgensen VL, Poulsen TD, Steinbrüchel D, Larsen B, Andersen LW. Increased concentrations of l-lactate in the rectal lumen in patients undergoing cardiopulmonary bypass. Br J Anaesth. 2000;95(6):764–8.
Haisjackl M, Birnbaum J, Redlin M, Schmutzler M, Waldenberger F, Lochs H, Konertz W, Kox W. Splanchnic oxygen transport and lactate metabolism during normothermic cardiopulmonary bypass in humans. Anesth Analg. 1998;86:22–7.
Braun JP, Schroeder T, Buehner S, Dohmen P, Moshirzadeh M, Grosse J, Streit F, Schlaefke A, Armstrong VW, Oellerich M, Lochs H, Konertz W, Kox WJ, Spies C. Splanchnic oxygen transport, hepatic function and gastrointestinal barrier after normothermic cardiopulmonary bypass. Acta Anaesthesiol Scand. 2004;48:697–703.
Dixon B, Santamaria JD, Campbell DJ. Plasminogen activator inhibitor activity is associated with raised lactate levels after cardiac surgery with cardiopulmonary bypass. Crit Care Med. 2003;31:1053–9.
Gasparovic H, Plestina S, Sutlic Z, Husedzinovic I, Coric V, Ivancan V, Jelic I. Pulmonary lactate release following cardiopulmonary bypass. Eur J Cardiothorac Surg. 2007;32:882–7.
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE. Relation between muscle Na+, K+ ATP activity and raised lactate concentration in septic shock: a prospective study. Lancet. 2005;365:871–5.
Mizock BA, Falk JL. Lactic acidosis in critical illness. Crit Care Med. 1992;20:80–93.
Arnold RC, Shapiro NI, Jones AE, Schorr C, Pope J, Casner E, Parrillo JE, Dellinger RP, Trzeciak S. Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock. 2009;32:35–9.
Shapiro NI, Howell MD, Talmor D, Nathanson LA, Lisbon A, Wolfe RE, Weiss JW. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med. 2005;45:524–8.
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32:1637–42.
Cerović O, Golubović V, Spec-Marn A, Kremzar B, Vidmar G. Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med. 2003;29:1300–5.
Siegel LB, Dalton HJ, Hertzog JH, Hopkins RA, Hannan RL, Hauser GJ. Initial postoperative serum lactate levels predict survival in children after open heart surgery. Intensive Care Med. 1996;22:1418–23.
Cheifetz IM, Kern FH, Schulman SR, Greeley WJ, Ungerleider RM, Meliones JN. Serum lactates correlate with mortality after operations for complex congenital heart disease. Ann Thorac Surg. 1997;64:735–8.
Hatherill M, Salie S, Waggie Z, Lawrenson J, Hewitson J, Reynolds L, Argent A. The lactate:pyruvate ratio following open cardiac surgery in children. Intensive Care Med. 2007;33:822–9.
Basaran M, Sever K, Kafali E, Ugurlucan M, Sayin OA, Tansel T, Alpagut U, Dayioglu E, Onursal E. Serum lactate level has prognostic significance after pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2006;20:43–7.
Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson KJ, Trzeciak S, Sherwin R, Holthaus CV, Osborn T, Rivers EP. Early goal-directed therapy in severe sepsis and septic shock revisited. Chest. 2006;130:1579–95.
Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA. Lactate clearance vs. central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;24:739–46.
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90:1052–9.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kogan, A., Preisman, S., Bar, A. et al. The impact of hyperlactatemia on postoperative outcome after adult cardiac surgery. J Anesth 26, 174–178 (2012). https://doi.org/10.1007/s00540-011-1287-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-011-1287-0