Abstract
Objective
To explore the relationship between lactate:pyruvate ratio, hyperlactataemia, metabolic acidosis, and morbidity.
Design and setting
Prospective observational study in the paediatric intensive care unit (PICU) of a university hospital.
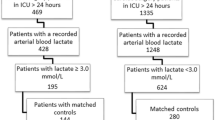
Patients
Ninety-seven children after open cardiac surgery. Most children (94%) fell into low-moderate operative risk categories; observed PICU mortality was 1%.
Interventions
Blood was sampled on admission for acid-base analysis, lactate, and pyruvate. Metabolic acidosis was defined as standard bicarbonate lower than 22 mmol/l, raised lactate as higher than 2 mmol/l, and raised lactate:pyruvate ratio as higher than 20.
Measurements and results
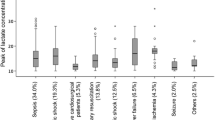
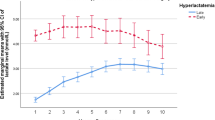
Median cardiopulmonary bypass and aortic cross-clamp times were 80 and 46 min. Metabolic acidosis occurred in 74%, hyperlactataemia in 42%, and raised lactate:pyruvate ratio in 45% of children. In multivariate analysis lactate:pyruvate ratio increased by 6.4 in children receiving epinephrine infusion and by 0.4 per 10 min of aortic cross-clamp. Duration of inotropic support increased by 0.29 days, ventilatory support by 0.27 days, and PICU stay by 0.42 days, for each 1 mmol/l increase in lactate. Neither standard bicarbonate nor lactate:pyruvate ratio were independently associated with prolongation of PICU support.
Conclusions
Elevated lactate:pyruvate ratio was common in children with mild metabolic acidosis and low PICU mortality. Hyperlactataemia, but not elevated lactate:pyruvate ratio or metabolic acidosis, was associated with prolongation of PICU support. Routine measurement of lactate:pyruvate ratio is not warranted for children in low-moderate operative risk categories.

Similar content being viewed by others
References
Duke T, Butt W, South M, Karl TR (1997) Early markers of major adverse events in children after cardiac operations. J Thorac Cardiovasc Surg 114:1042–1052
Siegel LB, Dalton HJ, Hertzog JH, Hopkins RA, Hannan RL, Hauser GJ (1996) Initial postoperative serum lactate levels predict survival in children after open heart surgery. Intensive Care Med 22:1418–1423
Hatherill M, Sajjanhar T, Tibby SM, Champion MP, Anderson D, Marsh MJ, Murdoch IA (1997) Serum lactate as a predictor of mortality after paediatric cardiac surgery. Arch Dis Child 77:235–238
Cheifetz IM, Kern FH, Schulman SR, Greeley WJ, Ungerleider RM, Meliones JN (1997) Serum lactates correlate with mortality after operations for complex congenital heart disease. Ann Thorac Surg 64:735–738
Rossi AF, Khan DM, Hannan R, Bolivar J, Zaidenweber M, Burke R (2005) Goal-directed medical therapy and point-of-care testing improve outcomes after congenital heart surgery. Intensive Care Med 31:98–104
Frey B, Macrae DJ (2005) Goal-directed therapy may improve outcome in complex patients-depending on the chosen treatment end point. Intensive Care Med 31:508–509
Hannan RL, Ybarra MA, White JA, Ojito JW, Rossi AF, Burke RP (2005) Patterns of lactate values after congenital heart surgery and timing of cardiopulmonary support. Ann Thorac Surg 80:1468–1473
Duke T (1999) Dysoxia and lactate. Arch Dis Child 81:343–350
James JH, Luchette FA, McCarter FD, Fischer JE (1999) Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet 354:505–508
Sumpelmann R, Schurholz T, Thorns E, Hausdorfer J (2001) Acid-base, electrolyte and metabolite concentrations in packed red blood cells for major transfusion in infants. Paediatr Anaesth 11:169–173
Toda Y, Duke T, Shekerdemian LS (2005) Influences on lactate levels in children early after cardiac surgery: prime solution and age. Crit Care Resusc 7:87–91
Sandstrom K, Nilsson K, Andreasson S, Larsson LE (1999) Open heart surgery; pump prime effects and cerebral arteriovenous differences in glucose, lactate and ketones. Paediatr Anaesth 9:53–59
Li J, Schulze-Neick I, Lincoln C, Shore D, Scallan M, Bush A, Redington AN, Penny DJ (2000) Oxygen consumption after cardiopulmonary bypass surgery in children: determinants and implications. J Thorac Cardiovasc Surg 119:525–533
Ganushchak YM, Maessen JG, de Jong DS (2002) The oxygen debt during routine cardiac surgery: illusion or reality? Perfusion 17:167–173
Durward A, Tibby SM, Skellett S, Austin C, Anderson D, Murdoch IA (2005) The strong ion gap predicts mortality in children following cardiopulmonary bypass surgery. Pediatr Crit Care Med 6:281–285
Murray DM, Olhsson V, Fraser JI (2004) Defining acidosis in postoperative cardiac patients using Stewart's method of strong ion difference. Pediatr Crit Care Med 5:240–245
Hatherill M, Salie S, Waggie Z, Lawrenson J, Hewitson J, Reynolds L, Argent A (2005) Hyperchloraemic metabolic acidosis following open cardiac surgery. Arch Dis Child 90:1288–1292
Levy B, Bollaert PE, Charpentier C, Nace L, Audibert G, Bauer P, Nabet P, Larcan A (1997) Comparison of norepinephrine and dobutamine to epinephrine for hemodynamics, lactate metabolism, and gastric tonometric variables in septic shock: a prospective, randomized study. Intensive Care Med 23:282–287
Levy B, Sadoune LO, Gelot AM, Bollaert PE, Nabet P, Larcan A (2000) Evolution of lactate/pyruvate and arterial ketone body ratios in the early course of catecholamine-treated septic shock. Crit Care Med 28:114–119
Gallet D, Goudable J, Vedrinne JM, Viale JP, Annat G (1997) Increased lactate/pyruvate ratio with normal beta-hydroxybutyrate/acetoacetate ratio and lack of oxygen supply dependency in a patient with fatal septic shock. Intensive Care Med 23:114–116
Suistomaa M, Ruokonen E, Kari A, Takala J (2000) Time-pattern of lactate and lactate to pyruvate ratio in the first 24 hours of intensive care emergency admissions. Shock 14:8–12
Weil MH, Afifi AA (1970) Experimental and Clinical Studies on Lactate and Pyruvate as Indicators of the Severity of Acute Circulatory Failure (Shock). Circulation 41:989–1001
De Pinieux G, Chariot P, Ammi-Said M, Louarn F, Lejonc JL, Astier A, Jacotot B, Gherardi R (1996) Lipid-lowering drugs and mitochondrial function: effects of HMG-CoA reductase inhibitors on serum ubiquinone and blood lactate/pyruvate ratio. Br J Clin Pharmacol 42:333–337
Jenkins KJ, Newburger JW, Lock JE, Davis RB, Coffman GA, Iezzoni LI (1995) In-hospital mortality for surgical repair of congenital heart defects: preliminary observations of variation by hospital caseload. Pediatrics 95:323–330
Shann F, Pearson G, Slater A, Wilkinson K (1997) Paediatric index of mortality (PIM): a mortality prediction model for children in intensive care. Intensive Care Med 23:201–207
Hatherill M, Waggie Z, Purves L, Reynolds L, Argent A (2002) Correction of the anion gap for albumin in order to detect occult tissue anions in shock. Arch Dis Child 87:526–529
Druml W, Grimm G, Laggner AN, Lenz K, Schneeweiss B (1991) Lactic acid kinetics in respiratory alkalosis. Crit Care Med 19:1120–1124
Dugas MA, Proulx F, de Jaeger A, Lacroix J, Lambert M (2000) Markers of tissue hypoperfusion in pediatric septic shock. Intensive Care Med 26:75–83
Jenkins KJ, Gauvreau K (2002) Center-specific differences in mortality: preliminary analyses using the Risk Adjustment in Congenital Heart Surgery (RACHS-1) method. J Thorac Cardiovasc Surg 124:97–104
Acknowledgements
This manuscript comprises a partial fulfilment of the requirements for an M.D. thesis (M.H.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Funded in part by a grant from the Institute of Child Health, University of Cape Town (M.H.)
Rights and permissions
About this article
Cite this article
Hatherill, M., Salie, S., Waggie, Z. et al. The lactate:pyruvate ratio following open cardiac surgery in children. Intensive Care Med 33, 822–829 (2007). https://doi.org/10.1007/s00134-007-0593-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0593-3