Abstract
Purpose
Distress is a factor that can adversely affect quality of life in breast cancer patients. A rapid and non-invasive tool to accurately detect distress is therefore important. The aims of the study were (1) to describe the women’s experiences after having received a breast cancer diagnosis and while awaiting primary surgery, in terms of anxiety and depression, (2) to evaluate the use of the Distress Thermometer (DT) in newly diagnosed breast cancer patients, and (3) to define an optimal cutoff score for the DT for this population.
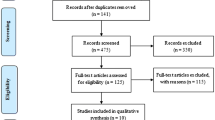
Method
This study involved 436 newly diagnosed patients in the pre-surgery phase. Consent forms and questionnaires were delivered by nurses during the pre-surgery check-ups, in the time between the 4 weeks post-diagnosis and the 2 weeks before surgery. Receiver operating characteristic analysis was used to evaluate the diagnostic accuracy of the DT compared to the Hospital Anxiety and Depression Scale (HADS) and to define an optimal cutoff score for the DT in this specific population.
Results
The results showed that the DT is a fast, easy, and well-accepted screening tool in the Italian context of women newly diagnosed with breast cancer, performing well in relation to the HADS. The proposed cutoff score for DT screening in the clinical setting is 4 versus 5.
Conclusion
The DT is recommended as a first step in screening, always followed by a more detailed evaluation of psychological functioning.


Similar content being viewed by others
References
IARC’s Global Cancer Observatory (2018). The online GLOBOCAN 2018 database. http://gco.iarc.fr/. Accessed 23 August 2019
AIRTUM Working Group (2018) I numeri del cancro 2018. Il Pensiero Scientifico Editore, Roma
Cordova MJ, Giese-Davis J, Golant M, Kronenwetter C, Chang V, Spiegel D (2007) Breast cancer as trauma: posttraumatic stress and posttraumatic growth. J Clin Psychol Med Settings 14(4):308–319
Nakatani Y, Iwamitsu Y, Kuranami M, Okazaki S, Yamamoto K, Watanabe M, Miyaoka H (2012) Emotional suppression and psychological responses to a diagnosis of breast cancer. Shinrigaku kenkyu: Jpn J Psychol 83(2):126–134. https://doi.org/10.4992/jjpsy.83.126
Wang HH, Chung UL (2012) Healthy lifestyle changes during the period before and after cancer diagnosis among breast cancer survivors. Asian Pac J Cancer Prev 13(9):4769–4772. https://doi.org/10.7314/APJCP.2012.13.9.4769
Mehnert A, Koch U (2007) Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: a prospective study. Psycho-Oncology: J Psychol Soc Behav Dimens Cancer 16(3):181–188. https://doi.org/10.1002/pon.1057
Rabin C, Pinto B (2006) Cancer-related beliefs and health behavior change among breast cancer survivors and their first-degree relatives. Psycho-Oncology: J Psychol Soc and Behav Dimens Cancer 15(8):701–712. https://doi.org/10.1002/pon.1000
Loeffler S, Poehlmann K, Hornemann B (2018) Finding meaning in suffering?—meaning making and psychological adjustment over the course of a breast cancer disease. Eur J Cancer Care 27(3):e12841. https://doi.org/10.1111/ecc.12841
Little M, Sayers E (2004) While there’s life…: hope and the experience of cancer. Soc Sci Med 59(6):1329–1337. https://doi.org/10.1016/j.socscimed.2004.01.014
Khan F, Amatya B, Pallant JF, Rajapaksa I (2012) Factors associated with long-term functional outcomes and psychological sequelae in women after breast cancer. Breast 21(3):314–320. https://doi.org/10.1016/j.breast.2012.01.013
Mehnert A, Hartung TJ, Friedrich M, Vehling S, Braehler E, Haerter M, Faller H (2017) One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psycho-Oncology 27:75–82. https://doi.org/10.1002/pon.4464
Morel N, Dayan J, Piolino P, Viard A, Allouache D, Noal S, Levy C, Joly F, Eustache F, Giffard B (2015) Emotional specificities of autobiographical memory after breast cancer diagnosis. Conscious Cogn 35:42–52. https://doi.org/10.1016/j.concog.2015.04.016
Pierrisnard C, Baciuchka M, Mancini J, Rathelot P, Vanelle P, Montana M (2018) Body image and psychological distress in women with breast cancer: a French online survey on patients’ perceptions and expectations. Breast Cancer 25(3):303–308. https://doi.org/10.1007/s12282-017-0828-2
Faretta E, Civilotti C (2016) EMDR therapy in psycho-oncology: a bridge between mind and body. J EMDR Pract Res 10(3):138–152. https://doi.org/10.1891/1933-3196.10.3.138
Basak F, Hasbahceci M, Guner S, Sisik A, Acar A, Yucel M, Kilic A, Bas G (2015) Prediction of anxiety and depression in general surgery inpatients: a prospective cohort study of 200 consecutive patients. Int J Surg 23:18–22. https://doi.org/10.1016/j.ijsu.2015.09.040
Miller SJ, Schnur JB, Weinberger-Litman SL, Montgomery GH (2014) The relationship between body image, age, and distress in women facing breast cancer surgery. Palliat Supportive Care 12(5):363–367. https://doi.org/10.1017/S1478951513000321
Drageset S, Lindstrøm TC, Giske T, Underlid K (2011) Being in suspense: women’s experiences awaiting breast cancer surgery. J Adv Nurs 67(9):1941–1951. https://doi.org/10.1111/j.1365-2648.2011.05638.x
Drageset S, Lindstrøm TC, Giske T, Underlid K (2012) “The support I need”: women’s experiences of social support after having received breast cancer diagnosis and awaiting surgery. Cancer Nurs 35(6):E39–E47. https://doi.org/10.1097/NCC.0b013e31823634aa
Boehmke MM, Dickerson SS (2006) The diagnosis of breast cancer: transition from health to illness. Oncol Nurs Forum 33:1121–1127
van't Spijker A, Trijsburg RW, Duivenvoorden HJ (1997) Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosom Med 59(3):280–293
Drageset S, Lindstrøm TC, Giske T, Underlid K (2016) Women’s experiences of social support during the first year following primary breast cancer surgery. Scand J Caring Sci 30(2):340–348. https://doi.org/10.1111/scs.12250
Ghirardello D, Munari J, Testa S, Torta R, Veglia F, Civilotti C (2018) Italian adaptation of the brief modified experiences in close relationships scale in a sample of cancer patients: factor analysis and clinical implications. Res Psychother: Psychopathol Process Outcome 21:209–217. https://doi.org/10.4081/ripppo.2018.319
Bultz BD, Groff SL, Fitch M, Blais MC, Howes J, Levy K, Mayer C (2011) Implementing screening for distress, the 6th vital sign: a Canadian strategy for changing practice. Psycho-Oncology 20(5):463–469. https://doi.org/10.1002/pon.1932
Absolom K, Holch P, Pini S, Hill K, Liu A, Sharpe M, Richardson A, Velikova G, Supportive NCRICOMPASS, Collaborative PCR (2011) The detection and management of emotional distress in cancer patients: the views of health-care professionals. Psycho-oncology 20(6):601–608. https://doi.org/10.1002/pon.1916
Testa S, Civilotti C, Di Fini G, Rossetto C, Boncinelli V, Veglia F (2016) Development of two equivalent short forms of the psychological general well-being index: PGWBI-A and PGWBI-B. TPM Testing, Psychometr, Methodol Appl Psychol 23:149–166
Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC (1998) Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer: Interdiscipl Int J Am Cancer Soc 82(10):1904–1908. https://doi.org/10.1002/(SICI)1097-0142
Grassi L, Johansen C, Annunziata MA, Capovilla E, Costantini A, Gritti P, Torta R, Bellani M, Italian Society of Psycho-Oncology Distress Thermometer Study Group (2013) Screening for distress in cancer patients: a multicenter, nationwide study in Italy. Cancer 119(9):1714–1721. https://doi.org/10.1002/cncr.27902
Cormio C, Caporale F, Spatuzzi R, Lagattolla F, Lisi A, Graziano G (2019) Psychosocial distress in oncology: using the distress thermometer for assessing risk classes. Support Care Cancer 20:1–7. https://doi.org/10.1007/s00520-019-04694-4
Donovan KA, Grassi L, McGinty HL, Jacobsen PB (2014) Validation of the distress thermometer worldwide: state of the science. Psycho-oncology 23(3):241–250. https://doi.org/10.1002/pon.3430
Schellekens MP, van den Hurk DG, Prins JB, Molema J, van der Drift MA, Speckens AE (2016) The suitability of the Hospital Anxiety and Depression Scale, Distress Thermometer and other instruments to screen for psychiatric disorders in both lung cancer patients and their partners. J Affect Disord 203:176–183. https://doi.org/10.1016/j.jad.2016.05.044
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Annunziata MA, Muzzatti B, Bidoli E, Flaiban C, Bomben F, Piccinin M, Gipponi KM, Mariutti G, Busato S, Mella S (2019) Hospital anxiety and depression scale (HADS) accuracy in cancer patients. Support Care Cancer:1–6. https://doi.org/10.1007/s00520-019-05244-8
Reuter K, Härter M (2001) Screening for mental disorders in cancer patients–discriminant validity of HADS and GHQ-12 assessed by standardized clinical interview. Int J Methods Psychiatr Res 10(2):86–96. https://doi.org/10.1002/mpr.103
Bener A, Alsulaiman R, Doodson LG, El Ayoubi HR (2016) Comparison of reliability and validity of the breast cancer Depression Anxiety Stress Scales (DASS-21) with the Beck Depression Inventory-(BDI-II) and Hospital Anxiety and Depression Scale (HADS). Int J Behav Res Psychol 4(4):197–203. https://doi.org/10.19070/2332-3000-1600035
Castelli L, Binaschi L, Caldera P, Torta R (2009) Depression in lung cancer patients: is the HADS an effective screening tool? Support Care Cancer 17(8):1129–1132. https://doi.org/10.1007/s00520-009-0604-8
Norton S, Cosco T, Doyle F, Done J, Sacker A (2013) The hospital anxiety and depression scale: a meta confirmatory factor analysis. J Psychosom Res 74(1):74–81. https://doi.org/10.1016/j.jpsychores.2012.10.010
Bidstrup PE, Mertz BG, Dalton SO, Deltour I, Kroman N, Kehlet H, Rottmann N, Gärtner R, Mitchell AJ, Johansen C (2012) Accuracy of the Danish version of the ‘distress thermometer’. Psycho-Oncology 21(4):436–443. https://doi.org/10.1002/pon.1917
Baken DM, Woolley C (2011) Validation of the distress thermometer, impact thermometer and combinations of these in screening for distress. Psycho-oncology 20(6):609–614. https://doi.org/10.1002/pon.1934
Shim EJ, Shin YW, Jeon HJ, Hahm BJ (2008) Distress and its correlates in Korean cancer patients: pilot use of the distress thermometer and the problem list. Psycho-Oncology: J Psychol Soc Behav Dimens Cancer 17(6):548–555. https://doi.org/10.1002/pon.1320
Ransom S, Jacobsen PB, Booth-Jones M (2006) Validation of the distress thermometer with bone marrow transplant patients. Psycho-Oncology: J Psychol Soc and Behav Dimens Cancer 15(7):604–612. https://doi.org/10.1002/pon.993
Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem 39(4):561–577
Grassi L, Travado L, Moncayo FL, Sabato S, Rossi E, SEPOS group (2004) Psychosocial morbidity and its correlates in cancer patients of the Mediterranean area: findings from the southern European psycho-oncology study. J Affect Disord 83(2–3):243–248. https://doi.org/10.1016/j.jad.2004.07.004
Annunziata MA, Giovannini L, Muzzatti B (2012) Assessing the body image: relevance, application and instruments for oncological settings. Supportive Care Cancer 20(5):901–907. https://doi.org/10.1007/s00520-011-1339-x
Scaruffi E, Franzoi IG, Civilotti C, Guglielmucci F, La Marca L, Tomelini M, Veglia F, Granieri A (2018) Body image, personality profiles and alexithymia in patients with polycystic ovary syndrome (PCOS). J Psychosom Obstet Gynecol 31:1–10. https://doi.org/10.1080/0167482X.2018.1530210
Ministero della Salute (2018).Tumore della mammella. http://www.salute.gov.it/portale/salute/p1_5.jsp?lingua=italiano&id=152&area=Tumori. Accessed 30 July 2019
Grassi L, Holland JC, Johansen C, Koch U, Fawzy F (2005) Psychiatric concomitants of cancer, screening procedures, and training of health-care professionals in oncology: the paradigms of psycho-oncology in the psychiatry field. Advances in psychiatry 2:59–66
Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, Elias AD, Farrar WB, Forero A, Giordano SH, Goetz MP, Goldstein LJ, Isakoff SJ, Lyons J, Marcom PK, Mayer IA, McCormick B, Moran MS, O'Regan RM, Patel SA, Pierce LJ, Reed EC, Salerno KE, Schwartzberg LS, Sitapati A, Smith KL, Smith ML, Soliman H, Somlo G, Telli M, Ward JH, Shead DA, Kumar R (2017) NCCN Guidelines Insights: Breast Cancer, Version 1.2017. J Natl Compr Canc Netw 15(4):433–451
Vodermaier A, Linden W, Siu C (2009) Screening for emotional distress in cancer patients: a systematic review of assessment instruments. J Natl Cancer Inst 101(21):1464–1488. https://doi.org/10.1093/jnci/djp336
Che-tuma MM (2018) An educational program for using the Distress Thermometer. Walden Dissertations and Doctoral Studies Collection, Florida
Zebrack B, Kayser K, Bybee D, Padgett L, Sundstrom L, Jobin C, Oktay J (2017) A practice-based evaluation of distress screening protocol adherence and medical service utilization. J Natl Compr Cancer Netw 15(7):903–912. https://doi.org/10.6004/jnccn.2017.0120
Tonsing KN, Vungkhanching M (2018) Assessing psychological distress in cancer patients: the use of distress thermometer in an outpatient cancer/hematology treatment center. Soc Work Health Care 57(2):126–136. https://doi.org/10.1080/00981389.2017.1402844
Grassi L, Sabato S, Rossi E, Marmai L, Biancosino B (2009) Affective syndromes and their screening in cancer patients with early and stable disease: Italian ICD-10 data and performance of the distress thermometer from the Southern European Psycho-oncology Study (SEPOS). J Affect Disord 114(1–3):193–199. https://doi.org/10.1016/j.jad.2008.07.016
Head BA, Schapmire TJ, Keeney CE, Deck SM, Studts JL, Hermann CP, Scharfenberger JA, Pfeifer MP (2012) Use of the distress thermometer to discern clinically relevant quality of life differences in women with breast cancer. Qual Life Res 21(2):215–223. https://doi.org/10.1007/s11136-011-9934-3
Carlson LE, Groff SL, Maciejewski O, Bultz BD (2010) Screening for distress in lung and breast cancer outpatients: a randomized controlled trial. J Clin Oncol 28(33):4884–4891. https://doi.org/10.1200/JCO.2009.27.3698
Akizuki N, Yamawaki S, Akechi NT, Uchitomi Y (2005) Development of an impact thermometer for use in combination with the distress thermometer as a brief screening tool for adjustment disorders and/or major depression in cancer patients. J Pain Symptom Manag 29(1):91–99. https://doi.org/10.1016/j.jpainsymman.2004.04.016
Dabrowski M, Boucher K, Ward JH, Lovell MM, Sandre A, Bloch J, Carlquist L, Porter M, Norman L, Buys SS (2007) Clinical experience with the NCCN distress thermometer in breast cancer patients. J Natl Compr Cancer Netw 5(1):104–111. https://doi.org/10.6004/jnccn.2007.0011
Iskandarsyah A, de Klerk C, Suardi DR, Soemitro MP, Sadarjoen SS, Passchier J (2013) The distress thermometer and its validity: a first psychometric study in Indonesian women with breast cancer. PLoS One 8(2):e56353. https://doi.org/10.1371/journal.pone.0056353
Hegel MT, Collins ED, Kearing S, Gillock KL, Moore CP, Ahles TA (2008) Sensitivity and specificity of the distress thermometer for depression in newly diagnosed breast cancer patients. Psycho-Oncology: J Psychol Soc Behav Dimens Cancer 17(6):556–560. https://doi.org/10.1002/pon.1289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Relevance of the manuscript
In the context of the Italian public health system, screening procedures for psychological problems are fundamental to achieve the goal of providing the best possible holistic care. At the same time, this care must be provided with the best and most efficient use of the human and economic resources available. The DT is a fast, easy, and well-accepted screening tool in the Italian context of women newly diagnosed with breast cancer, performing well in relation to the HADS. The test is recommended as a first step in the screening procedure, always followed by a more detailed evaluation of the psychological functioning of the patient.
Rights and permissions
About this article
Cite this article
Civilotti, C., Acquadro Maran, D., Santagata, F. et al. The use of the Distress Thermometer and the Hospital Anxiety and Depression Scale for screening of anxiety and depression in Italian women newly diagnosed with breast cancer. Support Care Cancer 28, 4997–5004 (2020). https://doi.org/10.1007/s00520-020-05343-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05343-x