Abstract
Purpose
The aim of this study was to evaluate whether body weight changes in patients undergoing chemotherapy for epithelial ovarian cancer (EOC) influence progression-free survival (PFS) and overall survival (OS).
Methods
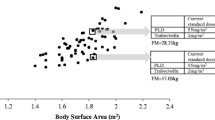
An analysis of 190 patients diagnosed with ovarian cancer after first-line chemotherapy was conducted. Changes in body weight were assessed by comparing measurements at baseline to those of the third and sixth cycles of chemotherapy. PFS and OS were calculated with the Kaplan–Meier method and multivariate Cox model.
Results
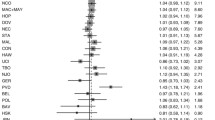
Significant reduction in body weight in advanced EOC was observed with no changes in early EOC. Significant differences in PFS were observed in advanced EOC patients that lost more than 5 % of their body weight (6 months), maintained weight (13 months), or gained more than 5 % of their body weight (15 months). Similarly, significant differences in OS were noted in advanced EOC at the following time points: 24.3, 42.4, and 66.2 months. No effect was reported for early EOC patients. The multivariate Cox analysis showed significant body weight changes from the first to the sixth chemotherapy cycle for PFS (HR = 0.97; 95 % CI 0.95–0.99) and OS (HR = 0.94; 95 % CI 0.91–0.97) as well as from the first to the third chemotherapy cycle for OS (HR = 0.93; 95 % CI 0.88–0.98).
Conclusions
Body weight changes can be recognized as a prognostic factor for PFS and OS in advanced EOC patients undergoing chemotherapy. Weight loss is associated with poorer survival while weight gain improved outcomes.




Similar content being viewed by others
References
Reynolds EA, Moller KA (2006) A review and an update on the screening of epithelial ovarian cancer. Curr Probl Cancer 30:203–232
Kearney N, Miller M, Maguire R, Dolan S, MacDonald R, McLeod J, Maher L, Sinclair L, Norrie J, Wengström Y (2008) WISECARE+: results of a European study of a nursing intervention for the management of chemotherapy-related symptoms. Eur J Oncol Nurs 12(5):443–448
Hall M, Gourley C, McNeish I, Ledermann J, Gore M, Jayson G, Perren T, Rustin G, Kaye S (2013) Targeted anti-vascular therapies for ovarian cancer: current evidence. Br J Cancer 108(2):250–258
Bandera EV, Kushi LH, Rodriguez-Rodriguez L (2009) Nutritional factors in ovarian cancer survival. Nutr Cancer 61:580–586
Collaborative Group on Epidemiological Studies of Ovarian Cancer (2012) Ovarian cancer and body size: individual participant meta-analysis including 25,157 women with ovarian cancer from 47 epidemiological studies. PLoS medicine 9:e1001200
Barrett SV, Paul J, Hay A, Vasey PA, Kaye SB, Glasspool RM, Scottish Gynaecological Cancer Trials Group (2008) Does body mass index affect progression-free or overall survival in patients with ovarian cancer? Results from SCOTROC I trial. Ann Oncol 19:898–902
Hess LM, Barakat R, Tian C, Ozols RF, Alberts DS (2007) Weight change during chemotherapy as a potential prognostic factor for stage III epithelial ovarian carcinoma: a gynecologic oncology group study. Gynecol Oncol 107:260–265
Ataseven B, Harter P, Grimm C, Heitz F, Heikaus S, Traut A, Kahl A, Kurzeder C, Prader S, du Bois A (2016) The revised 2014 FIGO staging system for epithelial ovarian cancer: is a subclassification into FIGO stage IVA and IVB justified? Gynecol Oncol. doi:10.1016/j.ygyno.2016.05.021
WHO (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva: World Health Organization
Protani MM, Nagle CM, Webb PM (2012) Obesity and ovarian cancer survival: a systematic review and meta-analysis. Cancer Prev Res 5:901–910
Zorlini R, Akemi Abe Cairo A, Salete Costa Gurgel M (2008) Nutritional status of patients with gynecologic and breast cancer. Nutr Hosp 23(6):577–583
Laky B, Janda M, Cleghorn G, Obermair (2008) A comparison of different nutritional assessments and body-composition measurements in detecting malnutrition among gynecologic cancer patients. Am J Clin Nutr 87(6):1678–1685
Davies M (2005) Nutritional screening and assessment in cancer-associated malnutrition. Eur J Oncol Nurs Suppl 2:S64–S73
Malihi Z, Kandiah M, Chan YM, Esfandbod M, Vakili M, Hosseinzadeh M, Zarif Yeganeh M (2015) The effect of dietary intake changes on nutritional status in acute leukaemia patients after first induction chemotherapy. Eur J Cancer Care 24(4):542–552
Gil KM, Frasure HE, Hopkins MP, Jenison EL, von Gruenigen VE (2006) Body weight and composition changes in ovarian cancer patients during adjuvant chemotherapy. Gynecol Oncol 103:247–252
Hutton JL, Baracos VE, Wismer WV (2007) Chemosensory dysfunction is a primary factor in the evolution of declining nutritional status and quality of life in patients with advanced cancer. J Pain Symptom Manag 33(2):156–165
Enig B, Petersen HN, Smith DF, Larsen B (1987) Food preferences, nutrient intake and nutritional status in cancer patients. Acta Oncol 26(4):301–315
Dell Antone P (2012) Energy metabolism in cancer cells: how to explain the Warburg and Crabtree effects? Med Hypotheses 79(3):388–392
Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME (2004) Cancer: disease and nutrition are key determinants of patients’ quality of life. Support Care Cancer 12(4):246–252
Ansell SM, Rapoport BL, Falkson G, Raats JI, Moeken CM (1993) Survival determinants in patients with advanced ovarian cancer. Gynecol Oncol 50:215–220
Kim SI, Kim HS, Kim TH, Suh DH, Kim K, No JH, Chung HH, Kim YB, Song YS (2014) Impact of underweight after treatment on prognosis of advanced-stage ovarian cancer. J Immunol Res 349546
Rutten IJ, van Dijk DP, Kruitwagen RF, Beets-Tan RG, Olde Damink SW, van Gorp T (2016) Loss of skeletal muscle during neoadjuvant chemotherapy is related to decreased survival in ovarian cancer patients. J Cachexia Sarcopenia Muscle. doi:10.1002/jcsm.12107
Mardas M, Jamka M, Mądry R, Walkowiak J, Krótkopad M, Stelmach-Mardas M (2015) Dietary habits changes and quality of life in patients undergoing chemotherapy for epithelial ovarian cancer. Support Care Cancer 23:1015–1023
Salminen EK, Lagström HK, Heikkilä S, Salminen S (2000) Does breast cancer change patients’ dietary habits? Eur J Clin Nutr 54:844–848
Van Loon K, Wigler D, Niedzwiecki D, Venook AP, Fuchs C, Blanke C, Saltz L, Goldberg RM, Meyerhardt JA (2013) Comparison of dietary and lifestyle habits among stage III and metastatic colorectal cancer patients: findings from CALGB 89803 and CALGB 80405. Clin Colorectal Cancer 12:95–102
Stephenson LE, Bebb DG, Reimer RA, Culos-Reed SN (2009) Physical activity and diet behaviour in colorectal cancer patients receiving chemotherapy: associations with quality of life. BMC Gastroenterol 9:60–69
Zhou Y, Chlebowski R, LaMonte MJ, Bea JW, Qi L, Wallace R, Lavasani S, Walsh BW, Anderson G, Vitolins M, Sarto G, Irwin ML (2014) Body mass index, physical activity, and mortality in women diagnosed with ovarian cancer: results from the Women’s Health Initiative. Gynecol Oncol 133:4–10
Backes FJ, Nagel CI, Bussewitz E, Donner J, Hade E, Salani R (2011) The impact of body weight on ovarian cancer outcomes. Int J Gynecol Cancer 21:1601–1605
Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME (2005) Dietary counseling improves patient outcomes: a prospective, randomized, controlled trial in colorectal cancer patients undergoing radiotherapy. J Clin Oncol 23(7):1431–1438
Ravasco P, Monteiro Grillo I, Camilo M (2007) Cancer wasting and quality of life react to early individualized nutritional counseling. Clin Nutr 26(1):7–15
Isenring EA, Capra S, Bauer JD (2004) Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer 91(3):447–452
De Waele E, Mattens S, Honoré PM, Spapen H, De Grève J, Pen JJ (2015) Nutrition therapy in cachectic cancer patients. The Tight Caloric Control (TiCaCo) pilot trial. Appetite 91:298–301
Acknowledgments
The authors are grateful to Dr. Robert Tower for the English correction of the manuscript.
Author’s contributions
MM was responsible for the data collection, data analysis, and writing the manuscript. MSM was responsible for the data analysis and writing the manuscript. RM was responsible for the data collection and critically reviewed the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The protocol of the study was approved by the local Bioethical Committee, which is associated with Poznan University of Medical Sciences (nr 399/15).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Mardas, M., Stelmach-Mardas, M. & Madry, R. Body weight changes in patients undergoing chemotherapy for ovarian cancer influence progression-free and overall survival. Support Care Cancer 25, 795–800 (2017). https://doi.org/10.1007/s00520-016-3462-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3462-1