Abstract
Background
The relationship between colorectal cancer (CRC) risk and physical activity and dietary habits has been well-established, but less is known about the relationship between these behaviours and quality of life (QOL) post-diagnosis. Moreover, it is unknown whether this relationship is consistent across cancer stage or treatment setting. Thus, the purpose of this study was to assess current diet and physical activity behaviour in CRC survivors receiving systemic chemotherapy, and to examine potential associations between these behaviours and quality of life. A secondary purpose was to examine the association between social support, diet, and physical activity behaviour in this population.
Methods
Using a cross-sectional survey, 67 CRC survivors currently receiving chemotherapy in Calgary, Alberta completed the survey package. Measures included demographic and medical data, physical activity levels, diet behaviour, QOL, and social support.
Results
In a largely metastatic sample (63%), approximately half were meeting national dietary guidelines (58%), less were meeting national physical activity guidelines (26%), and a small number were meeting both (17%). However, only 12.3% (n = 8) reported completely sedentary behaviour, and 7 of these 8 participants were receiving metastatic treatment. Neither behaviour was significantly associated with QOL or perceived social support. Furthermore, there were no significant QOL differences between those treated with palliative intent or adjuvant therapy. Important group differences emerged between those meeting and not meeting the guidelines, and associations between QOL, age, BMI, and provisions of social support.
Conclusion
These findings provide insight into lifestyle behaviours of CRC survivors currently receiving systemic chemotherapy, and the differences in perceived QOL as affected by severity of disease and treatment setting. Prospective studies in a larger sample of CRC survivors on chemotherapy are needed to confirm lifestyle behaviour patterns and identify factors related to QOL that are unique to this population, especially during metastatic treatment.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the second most prevalent cancer in Canada and third in the United States for men and women combined [1, 2]. With increased early detection and effective treatment, as well as an aging population, the number of CRC survivors is growing significantly. Although improvements in treatment regimens have beneficially impacted the prognosis of CRC, several quality of life (QOL) issues result from potential side effects of such aggressive treatment [3]. Consequently, shifting part of our focus in research and program development to address issues of QOL and survivorship has become essential [4].
Physical activity and diet are two lifestyle behaviours shown to significantly impact both QOL and survivorship in cancer populations [5]. Within the CRC population specifically, physical activity and diet behaviour have shown both an independent and combined positive association with QOL [6–10]. Specifically, sufficient levels of physical activity (i.e., meeting published guidelines) or consuming at least five servings of fruits and vegetables per day (i.e., 5-A-Day recommendation) have been associated with significantly higher measures of self-reported QOL. Additionally, health behaviour clusters have been identified (i.e., meeting guidelines for multiple behaviours such as diet, physical activity, and not smoking) which appear to have a cumulative impact on QOL [6, 7]. It has therefore been suggested that targeting multiple behaviours may prove more effective in enhancing QOL than focusing on individual behaviour change in the cancer survivor population [5].
However, not all studies concur with this impression. One recent study in particular found that no lifestyle variable was a significant predictor of domain-specific or overall QOL after CRC [11]. This discrepancy may be due, in part, to the varying QOL and health behaviour measures used, as well as differing sample characteristics. However, more research is warranted to determine whether the relationship between lifestyle and QOL persists across stages of CRC, treatment type (i.e., surgery, chemotherapy, radiation), or setting (i.e., adjuvant or metastatic). For example, physical activity trials during treatment in the general cancer literature have shown mixed results on impacting QOL. Findings have ranged from negative trends on QOL subscales, to positive statistically nonsignificant trends, to moderately significant beneficial effects (i.e, mental health, role and emotional functioning) [12–16].
Furthermore, despite the established link between lifestyle and CRC, several reports indicate that adherence to suggested guidelines for either behaviour is low. For example, recent studies have reported 25 to 54% of CRC survivors meeting varied published activity guidelines [7–10, 17], and 16 to 47% achieving the 5-A-Day diet recommendations [7, 8]. However, it is unknown whether the variance in adherence to both behaviours is consistent across all stages of CRC, or treatment setting. A greater understanding of factors underlying adherence to either behaviour would provide important insight into whether current guidelines are appropriate for all CRC survivors regardless of stage or treatment, and in turn guide future behavioural interventions in this population. Since these behaviours are linked to decreased recurrence risk and increased survival rates in CRC [18–20], as well as improved QOL [7], promotion of healthy lifestyle changes in this population is imperative.
The purpose of this study was to assess current physical activity and diet behaviour in CRC survivors undergoing chemotherapy, and examine how these behaviours may be related to QOL. Based on previous research in CRC, we hypothesized that adherence to either behaviour guideline would be low. However, we did predict that meeting physical activity and diet guidelines would correspond with higher self-reported QOL scores. A secondary purpose was to examine the association between social support, diet, and physical activity behaviour in this population. It has been suggested that social support may be a key factor in explaining some of the variance in healthy behaviours [21–23]. It was hypothesized that those with greater provisions of social support would report greater adherence to both behaviour guidelines.
Methods
This study was a cross-sectional survey design using a convenience sample of CRC patients currently receiving chemotherapy. Participants included CRC patients of the gastrointestinal (GI) tumour group at the Tom Baker Cancer Centre (Calgary, AB, Canada). Upon ethical approval from the Conjoint Health Research Ethics Board, University of Calgary, participants were recruited on-site during clinic visits in which the medical oncologist first obtained patient permission to be approached by the researcher. Eligibility criteria included: a) primary diagnosis of colon or rectal cancer, b) receiving chemotherapy (adjuvant or metastatic) not concurrent with radiotherapy, c) at least 18 years of age, and d) ability to read and write in English. By definition, adjuvant therapy is given with curative intent after the resection of all detectable disease, whereas metastatic treatment is given with palliative intent when the disease has spread to other parts of the body and is no longer modifiable. Of note, patients receiving radiotherapy were excluded based on the nutritional implications associated with this treatment regimen. A total of 112 patients were eligible for the study over a 6-month period, and 108 consented to complete the survey package and receive one reminder phone call to return the completed package.
Measures
The survey package was comprised of demographic and medical questions, physical activity and diet behaviour assessments, QOL and social support. Medical data was obtained through patient records to ensure accuracy. Specific measures included the following.
Physical Activity Behaviour
Physical activity was assessed using Godin's leisure score index (LSI) of the GLTEQ (Godin Leisure Time Exercise Questionnaire) [24]. The LSI is a 3-item measure assessing the frequency and duration of mild, moderate and strenuous bouts of physical activity performed during free time in a typical week. In this study, participants were asked to recall their physical activity levels over the past month. The LSI was then computed into MET hours, which included only moderate and strenuous activity in the present study to reflect the Canadian guidelines outlined in the questionnaire: "At least 30 minutes of moderate activity 4 or more times per week" [25]. Thus, participants needed to perform at least 10 MET hours per week to meet the guideline. The LSI has been successfully used with adult cancer patients and survivors [26, 27], and an independent evaluation of its reliability and validity compares favourably to nine other self-report measures of exercise [28].
Diet Behaviour
Diet was assessed using a 3-day diet record. This dietary measure is said to be the most accurate for mean macronutrient content and appropriate for use in studies where subjects may consume a wide variety of foods [29]. Participants were instructed to record their daily consumption over a period of three days, one of which must be a weekend day. From the diet records, percent of total recommended daily energy and macronutrient intake (i.e., fat, carbohydrates, and protein) were assessed based on individual height, weight, age, and gender. Servings of fruit and vegetables were also assessed. Participants were then classified as meeting or not meeting Canadian diet recommendations based on meeting the appropriate range for each macronutrient, the appropriate energy intake, and fruit and vegetable consumption. Specifically, participants had to be within the acceptable daily macronutrient distribution ranges for adults: carbohydrates = 45–65% of total energy intake, proteins = 10–35% of total energy intake, and fats = 20–35% of total energy intake [30]. These ranges reflect recommended daily servings in Canada's Food Guide [31].
Quality of Life
QOL was assessed using the Functional Assessment of Cancer Therapy – Colorectal module (FACT-C). This tool contains five subscales including physical, social-family, emotional, functional, and a CRC specific concerns subscale. It has been shown to be reliable and valid for assessing QOL within the CRC population [32, 33].
Social Support
Perceived social support was assessed using the Social Provisions Scale (SPS), which provides both a global social support score, and six relational provisions: attachment, social integration, reassurance of worth, reliable alliance, guidance, and opportunity to nurture [34]. Scores from this instrument have been shown to be reliable and valid within both healthy and cancer populations [22, 35].
Analysis
The raw data was analysed using SPSS Version 15.0. The 3-day diet records were first analysed by a registered Dietician using Diet Analysis Plus software (Thomson, Wadsworth, Toronto, ON) to provide total daily energy intake, and macro and micro-nutrient intake for each participant. Reports were specific to participants' age, gender, self-reported height, and weight. Percentage of recommended daily amounts and macronutrient intake was then added to the SPSS database for statistical analyses. After data input and cleaning, the normality of the data was analyzed (i.e., skewness and kurtosis). The data was within the requirements of normal distribution, thus no data transformations were necessary. Descriptive statistics included means, ranges and standard deviations on all demographics, medical variables, physical activity and diet behaviour, QOL, and social support. Individual t-tests and chi-squares were performed as appropriate to test differences between those meeting and not meeting the guidelines for both behaviours. Correlations and analyses of variance examined the relationship between behaviour, social support and QOL.
Results
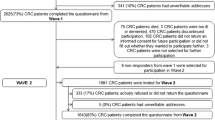
Of the 112 eligible participants seen in clinic over a six-month period, 108 (96%) consented to participate in the study. A total of 67 packages were returned (response rate = 62%), of which 63 were completed in full (i.e., both the questionnaire and 3-day diet record were returned). There were no statistically significant differences in medical data between those who completed and those who did not complete the survey. Sociodemographic data was only available for those who completed and returned the survey package.
Sample Characteristics
Complete demographics and medical information for the study sample (n = 67) is presented in Tables 1 and 2. In summary, the sample was reflective of national statistics for CRC. Participants' ages ranged from 29 to 84 years (M = 60.4), 52.2% were male, the majority were Caucasian (90.8%), married or common law (81.5%), many had a university or college education (35.9%), and 30.5% had an annual income greater or equal to $80,000. The medical data shows the mean time since diagnosis for the entire sample was 13.9 months (SD = 14.1). A small number of participants had an ostomy appliance (n = 15), and all participants were currently receiving chemotherapy with a mean time on active treatment of 5.9 months (SD = 7.7). More than two thirds were being treated for metastatic disease (62.7%), and the majority were initial diagnoses receiving Capecitabine in either treatment setting.
Physical Activity and Diet Behaviour
Descriptive statistics for physical activity and diet behaviour can be seen in Table 3. For physical activity behaviour, participants (n = 65) had an average of 5.5 MET hours per week (SD = 9.9). With 10 or more MET hours needed to satisfy the public activity guidelines, only 26.2% (n = 17) of participants were currently meeting the minimum amount of weekly physical activity. Reviewing the average weekly duration and frequency of mild, moderate and strenuous activity, participants were performing mild activity most often (M = 32.2 minutes; M = 3.1 times/week), followed by moderate activity (M = 11.7 minutes; M = 1.1 times/week), and strenuous activity (M = 5.4 minutes; M = 0.3 times/week). Of interest, only 12.3% (n = 8) reported sedentary behaviour (i.e., zero minutes of activity for all three intensities), of which 87.5 (n = 7) were being treated with palliative intent.
With regards to dietary behaviour, the majority of participants (58.5%) were meeting the national guidelines examined in this study. Looking at each macronutrient, participants fell within the acceptable range for carbohydrate (50.6%; acceptable range = 45–65%), protein (17.3%; acceptable range = 10–35%) and fat intake (31.3%; acceptable range = 20–35%). Furthermore, despite being on active treatment, on average participants were meeting more than their individual daily energy requirements (106.3%). Additionally, for comparison to previous studies assessing fruit and vegetable intake, 85.2% were achieving their recommended daily servings. Of note, only 17.5% of all participants met both physical activity and dietary guidelines.
Quality of Life and Social Support
Social support and QOL scores can be viewed in Table 4. In summary, mean scores for the SPS were high for our sample and comparable to healthy population means [34]. Specifically, reliable alliance (assurance that others can be counted on in times of stress) was reported as the highest relational provision (M = 14.7, SD = 1.6), with opportunity for nurturance (providing assistance to others) being the lowest (M = 12.1, SD = 2.2). The FACT-C scores indicated relatively high overall QOL in our sample (M = 95.6, SD = 15.7). Social/family well-being was the highest reported QOL domain (M = 22.6, SD = 4.1), and physical well-being was the poorest domain (M = 16.7, SD = 6.1).
Behavioural Associations with Quality of Life
Bivariate correlations were performed between each behaviour and quality of life for the entire sample. The only significant findings were that the social/family well-being subscale was negatively correlated with meeting the physical activity guidelines (r = -0.301, p = 0.016), and the CRC-specific concerns subscale was negatively correlated with meeting the dietary guidelines (r = -0.255, p = 0.044). That is, higher scores on either QOL subscale correlated to the participants not meeting the corresponding behaviour guideline. Analyses of variance were used to further explore this relationship. Results from these tests confirm findings from our correlations, as significant between group differences on QOL measures were only found for physical activity and social/family well-being [F(1,62) = 6.20, p = 0.016], and diet and CRC-specific concerns [F(1,61) = 4.23, p = 0.044].
Given the limited associations between either behaviour and QOL, we also performed bivariate correlations to examine potential significant relationships with medical, demographic, or social support variables (see Table 5). The data revealed that BMI was negatively correlated with QOL (p = 0.033), and age (p = 0.001), total social support (p = 0.017), attachment (p = 0.010), social integration (p = 0.001), reliable alliance (p = 0.024), and guidance (p = 0.021) were positively associated with QOL. Of note, there were no significant differences in QOL scores for either treatment setting (i.e., adjuvant or metastatic).
Group Differences
Individual t-tests were used to determine the significance between groups (i.e., those meeting or not meeting the stated guidelines) for continuous variables, and chi-square tests were used for categorical variables. Non-parametric Mann-U Whitney tests were also performed on ordinal measures and corresponded with t-test results; thus, t-tests have been reported. No significant differences were found in demographics, medical information or social support scores between those meeting and not meeting the guidelines for either behaviour.
Discussion
The primary objective of this study was to assess current physical activity and diet behaviour in CRC survivors currently receiving systemic chemotherapy, and to examine associations between these behaviours and QOL. Of importance, the majority (63%) had significant burden of disease and were being treated with palliative intent. In light of these sample characteristics, the percentage of participants engaging in sufficient levels of activity and following the public dietary guidelines is impressive, although only 17% were meeting both behaviour guidelines.
Specifically, meeting dietary guidelines, broadly defined as meeting energy needs, appropriate macronutrient intakes, and fruit and vegetable intake, was better achieved in this sample than physical activity when benchmarked against current public health guidelines for both behaviours. Approximately half of the participants (58%) were achieving the appropriate range of daily calories from each macronutrient (i.e., carbohydrate, protein, and fat). On average, participants were also meeting or slightly exceeding their daily energy requirements (106.3%), which is consistent with intakes observed in breast cancer survivors [36]. Although previous reports indicate poor adherence to dietary recommendations in the CRC population, this has been based on assessing fruit and vegetable intake as part of the American Cancer Society's 5-A-Day campaign [7, 8]. While direct comparisons cannot be made due to different diet assessment tools and sample characteristics, it should be noted that 85% of the current sample was meeting individually recommended servings of fruits and vegetables, which is considerably higher than previous reports. This may speak to the effectiveness of diet-specific health promotion strategies in the cancer population at large.
The public physical activity guidelines used in the current study call for at least 30 minutes of moderate activity, four or more times per week. Few were meeting these guidelines (26%), although this is comparable to other Canadian cancer survivors [37]. In comparison, a large number of our sample reported weekly mild activity (duration: M = 32.2 minutes; frequency: M = 3.1 times per week), and few (12%) reported no activity at all. This is positive, given the known risks of sedentary behaviour for survivors includes the development of comorbid conditions and cancer recurrence. Additionally, with the known potential side-effects from such aggressive treatment (i.e., neuropathy, hand and foot syndrome, diarrhoea, and nausea), achieving even mild activity (i.e., below the public activity guidelines) may be a more realistic goal for those with significant burden of disease undergoing treatment, and may still provide some benefits reported in the general cancer literature [38, 39]. For example, preliminary physical activity and palliation research found that a 50-minute physical activity intervention twice a week for six weeks was feasible in a sample of 34 palliative cancer patients, in which nine were receiving chemotherapy [40]. Specifically, circuit training with strength, aerobic, and flexibility components was successful for improving fitness measures, symptom management (fatigue), and well-being. Of importance, intensity of exercise activity was not specified to the participants.
It is not unexpected that activity levels would be below recommended levels in this population. Peddle at al. found that only 9% of a large sample of CRC survivors (60% Stage III or IV disease) reported sufficient activity levels during treatment, which increased to only 25% post-adjuvant therapy [10]. Similarly, recent American and Australian studies have reported that only 32–54% of CRC survivors meet physical activity guidelines (both during and post-treatment survivor samples) [7–9, 17]. While these studies used slightly different guidelines for minimum activity levels (i.e., >150 minutes of moderate activity per week) than the present study, it is apparent that activity levels are consistently reported as insufficient in CRC survivors. As there is a consistent call for establishing specific dose-response relationships (i.e., per different cancer type, stage, and treatment status) in the physical activity and cancer literature, future research should determine if lower levels of activity than the current guidelines suggest will still provide clinically meaningful health benefits for CRC survivors on chemotherapy, especially those with metastatic disease. For example, Spence et al. have reported their protocol for examining the health benefits of a supervised exercise program for CRC survivors immediately following adjuvant chemotherapy [41]. Such interventions are valuable for determining pertinent differences in achievable activity goals at specific stages of the cancer continuum and treatment settings.
An unexpected finding and contrary to our hypothesis, was that neither diet nor physical activity behaviour was significantly related to global QOL. Physical activity was negatively correlated to the social/family well-being subscale, and diet was negatively correlated to the CRC-specific concerns subscale (i.e., treatment-related side effects). Engaging in physical activity may be seen as taking away from important social/family interaction and thereby contribute to the observed negative association between activity and this subscale. The negative correlation between disease-specific concerns and following the dietary guidelines is not illogical, however, as the majority of the items on this subscale are directly related to the digestive process and those experiencing more symptoms are likely to adjust their diet to counter this.
The lack of associations between diet, physical activity and QOL may be due to the small sample of those actually meeting the physical activity guidelines (n = 17), dietary guidelines (n = 38), or both (n = 11), thereby making it difficult to detect significant relationships. Another potential explanation for this may be that 63% of the current sample was receiving chemotherapy for metastatic disease. Thus, this poor prognosis may significantly impact factors associated with QOL. As this was the first study to examine the association between lifestyle behaviours and QOL in a largely metastatic sample receiving systemic chemotherapy, these findings are important and need to be replicated.
With regards to QOL levels in the current study, both global and domain-specific QOL scores were lower than those reported in two previous CRC studies using the same measure. Specifically, the current sample reported a mean global QOL score of 95.9 (out of 136), compared to the means of 111.5 and 110 in these two previous studies [9, 10]. Interestingly, the physical well-being domain score was the lowest of the five subscales in the present sample (M = 16.7; out of 28), but highest in the two other studies (M = 23.6 and 24). The lower QOL scores in the present sample likely reflect that the participants were undergoing adjuvant or metastatic treatment. The other two studies included CRC survivors both on and off treatment, and previous studies have reported that global QOL levels tend to increase over time (i.e., after treatment completion) in this population [42]. Understanding the specific domains of QOL most affected in CRC survivors, which appears to vary according to severity of disease and treatment setting, is valuable for tailoring future interventions targeting QOL outcomes.
In a further attempt to understand QOL in the current sample, exploratory analyses examined significant relationships between QOL and demographic, medical, and social support variables. It appears in this sample that BMI, age, and social support provisions have stronger correlations with perceived QOL than do the lifestyle behaviours. Specifically, lower BMI, older age, and greater provisions of attachment, social integration, guidance, and reliable alliance were significantly associated with overall QOL. Interestingly, no significant differences on any QOL scales were found between those treated in the adjuvant or metastatic setting. Contrary to what one might expect, this may imply that QOL is no worse when treated with palliative intent as compared to adjuvant therapy in this population. This needs to be confirmed in future studies.
With respect to age, Arndt et al. also found that younger CRC survivors reported worse QOL in functioning and symptom scales than older survivors [42]. It has been hypothesized from breast cancer studies that younger survivors may have less coping strategies and view their cancer as a greater threat to their lives [43–45]. The BMI and QOL correlation is also consistent with past research, which noted that those with lower BMIs reported higher perceived QOL [46]. A larger sample may replicate these findings, but also suggests that future studies with QOL as the primary endpoint may need to tailor interventions to age-specific needs of the participants.
The relationship between QOL and social support provisions found in this study is supportive of the findings in previous QOL and CRC research. Dunn and colleagues found that participants expressed emotional, instrumental, and spiritual support as most beneficial to their cancer experience [47], and Sultan et al. found that provision of emotional and instrumental support corresponded with improved QOL in survivors [48]. In addition, the recent work of Steginga et al. found social support to be significantly associated with all domains of QOL, and a significant independent predictor of social well-being, functional well-being, and overall QOL [11]. Although varying measures of social support were used in these studies, the culmination of these findings suggest that social support may be more directly related to subjective well-being for CRC survivors, and a key target for future QOL research in this population. However, as stated previously, knowing if this relationship is consistent along the cancer continuum or varies with stage and treatment of CRC needs to be investigated.
Although the present study was the first to look at both physical activity and diet behaviour exclusively in CRC survivors receiving chemotherapy, and the association between these behaviours and QOL, there are limitations to be noted. Primarily, the small and convenience sample limits the generalizability of the findings and ability to detect statistically meaningful relationships. Furthermore, the self-report nature of behaviour and the potential for social desirability may have influenced reporting for either behaviour. Using objective measures of behaviour in a larger sample to replicate these findings is important for providing the baseline data to effectively design future lifestyle trials in this population.
Conclusion
In summary, this study found novel and important baseline information on current dietary and physical activity behaviour in the CRC population undergoing systemic chemotherapy. In light of our sample characteristics, especially the significant burden of disease in the majority of participants, the number who are engaging in physical activity is positive, and the high percentage following healthy food guidelines even more so. Moreover, the largely metastatic sample presents an understudied and important area for future research. Having these baseline measures are essential for future lifestyle research initiatives in this population, which are likely to vary with cancer stage and the different phases of the cancer experience. As well, our findings provide insight into the differences in perceived QOL as affected by treatment setting and severity of disease, compared with existing literature reporting QOL post-treatment and into survivorship in samples with less advanced disease. Evidence-based interventions are warranted in this population, especially to determine appropriate dose-response relationships between activity or diet and meaningful health benefits for survivors being treated with adjuvant or metastatic chemotherapy. Furthermore, the role of social support and other potential variables more highly associated with QOL should be explored to effectively target QOL outcomes specific to diagnosis and treatment.
References
Colorectal Cancer Stats. [http://www.cancer.ca/canada-wide/about%20cancer/cancer%20statistics/stats%20at%20a%20glance/colorectal%20cancer.aspx?sc_lang=en]
How Many People Get Colorectal Cancer?. [http://www.cancer.org/docroot/CRI/content/CRI_2_2_1X_How_Many_People_Get_Colorectal_Cancer.asp?sitearea=]
DeCosse JJ, Cennerazzo WJ: Quality-of-Life management of patients with colorectal cancer. CA Cancer J Clin. 1997, 47: 198-206. 10.3322/canjclin.47.4.198.
Baker F, Denniston M, Smith T, West MM: Adult cancer survivors: how are they faring?. Cancer. 2005, 104 (Suppl 11): 2565-2576. 10.1002/cncr.21488.
Demark-Wahnfried W, Jones LW: Promoting a healthy lifestyle among cancer survivors. Hematol Oncol Clin N Am. 2008, 22: 319-342. 10.1016/j.hoc.2008.01.012.
Blanchard CM, Stein KD, Baker F, Dent MF, Denniston MM, Courneya KS, Nehl E: Association between current lifestyle behaviors and health-related quality of life in breast, colorectal, and prostate cancer survivors. Psychol Health. 2004, 19: 1-13. 10.1080/08870440310001606507.
Blanchard CM, Courneya KS, Stein K: Cancer survivors' adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society's SCS-II. J Clin Oncol. 2008, 26: 2198-2204. 10.1200/JCO.2007.14.6217.
James AS, Campbell MK, DeVellis B, Reedy J, Carr C, Sandler RS: Health behavior correlates among colon cancer survivors: NC STRIDES baseline results. Am J Health Behav. 2006, 30: 720-730.
Lynch BM, Cerin E, Owen N, Aitken JF: Associations of leisure-time physical activity with quality of life in a large, population-based sample of colorectal cancer survivors. Cancer Causes Control. 2007, 18: 735-742. 10.1007/s10552-007-9016-6.
Peddle CJ, Au HJ, Courneya KS: Associations between exercise, quality of life, and fatigue in colorectal cancer survivors. Dis Colon Rectum. 2008, 51: 1242-1248. 10.1007/s10350-008-9324-2.
Steginga SK, Lynch BM, Hawkes A, Dunn J, Aitken J: Antecedents of domain-specific quality of life after colorectal cancer. Psychooncology. 2009, 18: 216-220. 10.1002/pon.1388.
Ademsen L, Midtgaard J, Rorth M, et al: Feasibility, physical capacity, and health benefits of a multidimensional exercise program for cancer patients undergoing chemotherapy. Support Care Cancer. 2003, 11: 707-716. 10.1007/s00520-003-0504-2.
Ademsen L, Quist M, Midtgaard J, et al: The effect of a multidimensional exercise intervention on physical capacity, well-being, and quality of life in cancer patients undergoing chemotherapy. Support Care Cancer. 2006, 14: 116-127. 10.1007/s00520-005-0864-x.
Losito JM, Murphy SO, Thomas ML: The effects of group exercise on fatigue and quality of life during cancer treatment. Oncol Nurs Forum. 2006, 33: 821-825. 10.1188/06.ONF.821-825.
Midtgaard J, Rorth M, Stelter R, Adamsen L: The group matters: an explorative study of group cohesion and quality of life in cancer patients participating in physical exercise intervention during treatment. Eur J Cancer Care (Engl). 2006, 15: 25-33. 10.1111/j.1365-2354.2005.00616.x.
Wilson RW, Taliaferro LA, Jacobsen PB: Pilot study of a self-administered stress management and exercise intervention during chemotherapy for cancer. Support Care Cancer. 2006, 14: 928-935. 10.1007/s00520-006-0021-1.
Hawkes AL, Lynch BM, Youlden DR, Owen N, Aitken JF: Health behaviors of Australian colorectal cancer survivors, compared with noncancer population controls. Support Care Cancer. 2008, 16: 1097-1104. 10.1007/s00520-008-0421-5.
Meyerhardt JA, Giovannucci EL, Holmes MD, et al: Physical activity and survival after colorectal cancer diagnosis. J Clin Oncol. 2006, 24: 3527-3534. 10.1200/JCO.2006.06.0855.
Meyerhardt JA, Heseltine D, Niedzwiecki D, et al: Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol. 2006, 24: 3535-3541. 10.1200/JCO.2006.06.0863.
Meyerhardt JA, Niedzwiecki D, Hollis D, et al: Association of dietary patterns with cancer recurrence and survival in patients with stage III colon cancer. JAMA. 2007, 298: 754-764. 10.1001/jama.298.7.754.
Courneya KS, Plotnikoff RC, Hotz SP, Birkett NJ: Social support and the theory of planned behavior in the exercise domain. Am J Health Behav. 2000, 24: 300-308.
Rhodes RE, Jones LW, Courneya KS: Extending the theory of planned behavior in the exercise domain: a comparison of social support and subjective norm. Res Q Exerc Sport. 2002, 73: 193-199.
Povey R, Conner M, Sparks P, James R, Shepherd R: The theory of planned behaviour and healthy eating: Examining additive and moderating effects of social influence variables. Psychol Health. 2000, 14: 991-1006. 10.1080/08870440008407363.
Godin G, Sheppard RJ: A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985, 10: 141-146.
Canada's Physical Activity Guide for Active Living. [http://www.phac-aspc.gc.ca/pau-uap/paguide/index.html]
Courneya KS, Friedenreich CM: Determinants of exercise during colorectal cancer treatment: an application of the theory of planned behavior. Oncol Nurs Forum. 1997, 24: 1715-1723.
Courneya KS, Friedenreich CM: Relationship between exercise pattern across the cancer experience and current quality of life in colorectal cancer survivors. J Altern Complement Med. 1997, 3: 215-226. 10.1089/acm.1997.3.215.
Jacobs DR, Ainsworth BE, Hartman TJ, Leon AS: A simultaneous evaluation of ten commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993, 25: 81-91. 10.1249/00005768-199301000-00012.
American Dietetic Association, Dietitians of Canada: Manual of Clinical Dietetics. 2000, Chicago: American Dietetic Association, 6
Institute of Medicine: Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Protein and Amino Acids (Macronutrients). 2002, Washington: National Academies Press
Canada's Food Guide to Healthy Eating. [http://www.hc-sc.gc.ca/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/fg_rainbow_bw-arc_en_ciel_ga_nb_e.pdf]
Ward WL, Hahn EA, Mo F, Hernandez L, Tulsky DS, Cella D: Reliability and validity of the Functional Assessment of Cancer Therapy-Colorectal (FACT-C) quality of life instrument. Qual Life Res. 1999, 8: 181-95. 10.1023/A:1008821826499.
Yost K, Eton D, Cella D, Ayanian J, Zaslavsky A, West D: Minimal important differences on the Functional Assessment of Cancer Therapy – Colorectal. Qual Life Res. 2002, 77: 629-
Russell D, Cutrona CE: The provisions of social relationships and adaptation to stress. Advances in Personal Relationships. 1987, 1: 37-67.
Saunders RP, Motl RW, Dowda M, Dishman RK, Pate RR: Comparison of social variables for understanding physical activity in adolescent girls. Am J Health Behav. 2004, 28: 426-436.
Twiss JJ, Gross GJ, Waltman NL, Ott CD, Lindsey AM: Health behaviors in breast cancer survivors experiencing bone loss. J Am Acad Nurse Pract. 2006, 18: 471-481. 10.1111/j.1745-7599.2006.00165.x.
Courneya KS, Katzmarzyk PT, Bacon E: Physical activity and obesity in Canadian cancer survivors. Cancer. 2008, 112: 2475-2482. 10.1002/cncr.23455.
Irwin ML: Physical activity interventions for cancer survivors. Br J Sports Med. 2009, 43: 32-38. 10.1136/bjsm.2008.053843.
Courneya KS, Friedenreich CM: Physical activity and cancer control. Semin Oncol Nurs. 2007, 23: 242-252. 10.1016/j.soncn.2007.08.002.
Odervoll LM, Loge JH, Paltiel H, et al: The effect of a physical exercise program in Palliative Care: A phase II study. J Pain Symptom Manage. 2006, 31: 421-430. 10.1016/j.jpainsymman.2005.10.004.
Spence RR, Heesch KC, Eakin EG, Brown WJ: Randomised controlled trial of a supervised exercise rehabilitation program for colorectal cancer survivors immediately after chemotherapy: study protocol. BMC Cancer. 2007, 7: 154-10.1186/1471-2407-7-154.
Arndt V, Merx H, Stegmaier C, Ziegler H, Brenner H: Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: a population-based study. J Clin Oncol. 2004, 22: 4829-4836. 10.1200/JCO.2004.02.018.
Ganz PA, Rowland JH, Desmond K, Meyerowitz BE, Wyatt GE: Life after breast cancer: understanding women's health-related quality of life and sexual functioning. J Clin Oncol. 1998, 16: 501-514.
Vinokur AD, Threatt BA, Vinokur-Kaplan D, Satariano WA: The process of recovery from breast cancer for younger and older patients: changes during the first year. Cancer. 1990, 65: 1242-1254. 10.1002/1097-0142(19900301)65:5<1242::AID-CNCR2820650535>3.0.CO;2-1.
Wenzel LB, Fairclough DL, Brady MJ, et al: Age-related differences in the quality of life of breast carcinoma patients after treatment. Cancer. 1999, 86: 1768-1774. 10.1002/(SICI)1097-0142(19991101)86:9<1768::AID-CNCR19>3.0.CO;2-O.
Pakiz B, Flatt SW, Mill KC, Jordan LJ, Carethers JM, Rock CL: Quality of life and diet intervention in individuals at risk for recurrence of colorectal adenomas. Psychooncology. 2005, 14: 85-93. 10.1002/pon.822.
Dunn J, Lynch B, Rinaldis M, et al: Dimensions of quality of life and psychosocial variables most salient to colorectal cancer patients. Psychooncology. 2006, 15: 20-30. 10.1002/pon.919.
Sultan S, Fisher DA, Voils CI, Kinney AY, Sandler RS, Provenzale D: Impact of functional support on health-related quality of life in patients with colorectal cancer. Cancer. 2004, 101: 2737-2743. 10.1002/cncr.20699.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-230X/9/60/prepub
Acknowledgements
LES was funded by the Canadian Institute for Health Research Masters Graduate Award. SNCR is funded by the Alberta Heritage Foundation for Medical Research. DGB is funded by the Leukemia Lymphoma Foundation of Canada, and the Tom Baker Cancer Centre, Alberta Health Services. RAR is funded by the Canadian Institutes of Health Research. A special thanks to the GI Tumour Group at the Tom Baker Cancer Centre for their support of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LES formulated the aims and hypothesis of the study, conducted the research, performed all statistical analysis and drafted the manuscript. SNCR was the formal MSc supervisor of LES, and contributed to and advised all aspects of the study. DGB was a co-investigator on the study and contributed to the research design, data collection, and critical revision of the manuscript. RAR was on the formal supervisory committee of LES, and contributed to interpretation of the findings and critical revision of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Stephenson, L.E., Bebb, D.G., Reimer, R.A. et al. Physical activity and diet behaviour in colorectal cancer patients receiving chemotherapy: associations with quality of life. BMC Gastroenterol 9, 60 (2009). https://doi.org/10.1186/1471-230X-9-60
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-230X-9-60