Abstract
Introduction
Hiatal hernia recurrence following surgical repair is common. We sought to define the most common anatomic location and mechanism for hiatal failure to inform technical strategies to decrease recurrence rates.
Methods
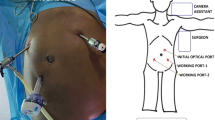
Retrospective chart review and video analysis were performed for all recurrent hiatal hernia operations performed by a single surgeon between January 2013 and April 2020. Hiatal recurrences were defined by anatomic quadrants. Recurrences on both left and right on either the anterior or posterior portion of the hiatus were simply classified as ‘anterior’ or ‘posterior’, respectively. Three or more quadrants were defined as circumferential. Mechanism of recurrence was defined as disruption of the previous repair or dilation of the hiatus.
Results
There were 130 patients to meet criteria. Median time to reoperation from previous hiatal repair was 60 months (IQR19.5–132). First-time recurrent repairs accounted for 74%, second time 18%, and three or more previous repairs for 8% of analyzed procedures. Mesh had been placed at the hiatus in a previous operation in 16%. All reoperative cases were completed laparoscopically. Video analysis revealed anterior recurrences were most common (67%), followed by circumferential (29%). There were two with left-anterior recurrence (1.5%), two posterior recurrence (1.5%), and one right-sided recurrence. The mechanism of recurrence was dilation in 74% and disruption in 26%. Disruption as a mechanism was most common in circumferential hiatal failures. Neither the prior number of hiatal surgeries nor the presence of mesh at the time of reoperation correlated with anatomic recurrence location or mechanism. Reoperations in patients with hiatal disruption occurred after a shorter interval when compared to hiatal dilation.
Conclusion
The most common location and mechanism for hiatal hernia recurrence is anterior dilation of the hiatus. Outcomes following techniques designed to reinforce the anterior hiatus and perhaps to prevent hiatal dilation should be explored.


Similar content being viewed by others
References
Luketich JD, Nason KS, Christie NA, Pennathur A, Jobe BA, Landreneau RJ, Schuchert MJ (2010) Outcomes after a decade of laparoscopic giant paraesophageal hernia repair. J Thorac Cardiovasc Surg 139(2):395–404
Dallemange B, Kohnen L, Perretta S, Weerts J, Markiewicz S, Jehaes C (2011) Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg 253(2):291–296
Saad A, Velanovich V (2020) Anatomic observation of recurrent hiatal hernia: recurrence or disease progression? J Am Coll Surg 230(6):999–1007
Zhou T, Harnsberger C, Broderick R, Fuchs H, Talamini M, Jacobsen G, Horgan S, Chang D, Sandler B (2015) Reoperation rates after laparoscopic fundoplication. Surg Endosc 29:510–514
Obeid N, Altieri M, Yang J, Park J, Price K, Bates A, Pryor AD (2018) Patterns of reoperation after failed fundoplication: an analysis of 9462 patients. Surg Endosc 32:345–350
Kanani Z, Gould JC (2021) Laparoscopic fundoplication for refractory GERD: a procedure worth repeating if needed. Surg Endosc 35(1):298–302
Funk LM, Kanji A, Scott Melvin W, Perry KA (2014) Elective antireflux surgery in the US: an analysis of national trends in utilization and inpatient outcomes from 2005 to 2010. Surg Endosc 28:1712–1719
Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD (2007) Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc 21(11):1978–1984
Iqbal A, Kakarlapudi GV, Awad ZT, Haynatzki G, Turaga KK, Karu A, Fritz K, Haider M, Mittal SK, Filipi CJ (2006) Assessment of diaphragmatic stressors as risk factors for symptomatic failure of laparoscopic Nissen fundoplication. J Gastrointest Surg 10(1):12–21
Kunio NR, Dolan JP, Hunter JG (2015) Short esophagus. Surg Clin North Am 95(3):641–652
Asling B, Jirholt J, Hammond P, Knutsson M, Walentinsson A, Davidson G, Agreus L, Lehmann A, Lagerstrom-Fermer M (2009) Collagen type III alpha I is a gastro-oesophageal reflux disease susceptibility gene and a male risk factor for hiatus hernia. Gut 58(8):1063–1069
Suppiah A, Sirimanna P, Vivian SJ, O’Donnell H, Lee G, Falk GL (2017) Temporal patterns of hiatus hernia recurrence and hiatal failure: quality of life and recurrence after revisional surgery. Dis Esophagus 30(4):1–8
Parker M, Bowers SP, Bray JM, Harris AS, Belli EV, Pfluke JM, Preissler S, Asbun HJ, Smith CD (2010) Hiatal mesh is associated with major resection at revisional operation. Surg Endosc 24:3095–3101
Nadipati K, Bye M, Yamamoto SR, Pallati P, Lee T, Mittal SK (2013) Reoperative intervention in patients with mesh at the hiatus is associated with high incidence of esophageal resection–a single-center experience. J Gastrointest Surg 17:2039–2044
Oelschlager BK, Peterson RF, Brunt LM, Soper NJ, Sheppard BC, Mitsumori L, Rohrmann C, Swanstrom LL, Pellegrini CA (2012) Laparoscopic paraesophageal hernia repair: defining long-term clinical and anatomic outcomes. J Gastrointest Surg 16:453–459
Memon MA, Memon B, Yunus RM, Khan S (2016) Suture cruroplasty versus prosthetic hiatal herniorrhaphy for large hiatal hernia: a meta-analysis and systematic review of randomized controlled trials. Ann Surg 263(2):258–266
Obeid NM, Velanovich V (2013) The choice of primary repair or mesh repair for paraesophageal hernia: a decision analysis based on utility scores. Ann Surg 257:655–664
Pfluke JM, Parker M, Bowers SP, Asbun HJ, Smith CD (2012) Use of mesh for hiatal hernia repair: a survey of SAGES members. Surg Endosc 26:1843–1848
Frantzides CT, Madan AK, Carlson MA, Stavropoulos GP (2002) A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair versus simple cruroplasty for large hiatal hernia. Arch Surg 137(6):649–652
Granderath FA, Granderath UM, Pointer R (2008) Laparoscopic revisional fundoplication with circular hiatal mesh prosthesis: the long-term results. World J Surg 32(6):999–1007
Fisichella PM (2013) A synopsis of techniques for paraesophageal hernia repair: different approaches to current controversies. Surg Laparosc Endosc Percutan Tech 23(5):423–424
Zeljka J, Louie BE (2013) Laparoscopic paraesophageal hernia repair. Surg Laparosc Endosc Percutan Tech 23(5):436–441
Nwokedi U, Nguyen DT, MeisenBach LM, Chihara R, Chan EY, Graviss EA, Kim MP (2021) Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc 35(7):3840–3849
Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki M (2020) Using impedance planimetry (EndoFLIP™) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 34(4):1761–1768
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
AG and ML have no conflict of interest. Dr. Gould reports relationships with Ethicon/J&J (preceptor, honorarium) and BD (speaker, honorarium).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Linnaus, M.E., Garren, A. & Gould, J.C. Anatomic location and mechanism of hiatal hernia recurrence: a video-based assessment. Surg Endosc 36, 5451–5455 (2022). https://doi.org/10.1007/s00464-021-08887-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08887-z