Abstract
Background
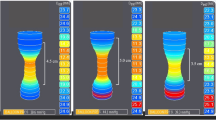
Endoluminal functional lumen imaging probe (EndoFLIP) technology is a tool that can be used to provide intraoperative objective real-time feedback during hiatal hernia repair. We wanted to determine the implication of initial distensibility index (DI) after mobilization of hiatus and final DI after creation of barrier in short-term clinical outcomes.
Methods
We performed a retrospective analysis of prospectively collected data on the intraoperative use of EndoFLIP during hiatal hernia repair at a single institution from 2017 to 2019. We analyzed the initial DI and final DI with the short-term clinical outcomes.
Results
There were 163 patients who had Nissen (n = 16), Toupet (n = 79) or magnetic sphincter augmentation (n = 68) with (n = 158) or without (n = 5) hiatal hernia repair with median initial DI was 3.2 mm2/mmHg. We used 3 mm2/mmHg as the cutoff for low (n = 84) vs. high (n = 79) initial DI group. There was no difference in DeMeester score (p = 0.76), the peristalsis on manometry (p = 0.13), type of hiatal hernia (p = 0.98), and GERD-HRQL score prior to surgery (p = 0.73) between the groups. There was significantly higher final DI in the high initial DI group compared to low initial DI group; however, there was no significant difference in the GERD-HRQL score at 1–3 months (p = 0.28). All of the patients had a final DI > 0.5 mm2/mmHg at the end of the case with median final DI of 1.6 mm2/mmHg. None of these patients required steroids (0%) and only one patient (0.6%) required EGD and dilatation as well as re-operation for dysphagia within 3 months.
Conclusions
The initial DI was associated with final DI, but it did not correlate with improvement in short-term GERD-HRQL score. Final DI maintained above the cutoff value led to most of the patients not to require intervention for dysphagia. Use of the EndoFLIP can provide objective data during the operation and prevent severe dysphagia after repair.





Similar content being viewed by others
References
Jarral OA, Athanasiou T, Hanna GB, Zacharakis E (2012) Is an intra-oesophageal bougie of use during Nissen fundoplication? Interact Cardiovasc Thorac Surg 14(6):828–833
Huttl TP, Hohle M, Wichmann MW, Jauch KW, Meyer G (2005) Techniques and results of laparoscopic antireflux surgery in Germany. Surg Endosc 19(12):1579–1587
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28(3):178–182
Tucker E, Sweis R, Anggiansah A, Wong T, Telakis E, Knowles K, Wright J, Fox M (2013) Measurement of esophago-gastric junction cross-sectional area and distensibility by an endolumenal functional lumen imaging probe for the diagnosis of gastro-esophageal reflux disease. Neurogastroenterol Motil 25(11):904–910
Perretta S, Dallemagne B, McMahon B, Agostino J, Marescaux J (2011) Video Improving functional esophageal surgery with a smart bougie. Endoflip. Surg Endosc. 25(9):3109
Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki MB (2019) Using impedance planimetry (EndoFLIP) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc. https://doi.org/10.1007/s00464-019-06925-5
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31(1):193–198
Turner B, Helm M, Hetzel E, Gould JC (2019) Is that 'floppy' fundoplication tight enough? Surg Endosc. https://doi.org/10.1007/s00464-019-06947-z
Ilczyszyn A, Botha AJ (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27(7):637–644
Lottrup C, McMahon BP, Ejstrud P, Ostapiuk MA, Funch-Jensen P, Drewes AM (2016) Esophagogastric junction distensibility in hiatus hernia. Dis Esophagus 29(5):463–471
Carlson DA, Kou W, Lin Z, Hinchcliff M, Thakrar A, Falmagne S, Prescott J, Dorian E, Kahrilas PJ, Pandolfino JE (2019) Normal values of esophageal distensibility and distension-induced contractility measured by functional luminal imaging probe panometry. Clin Gastroenterol Hepatol. 17(4):674–681
Nathanson LK, Brunott N, Cavallucci D (2012) Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP(R)). Surg Endosc 26(4):1051–1055
Carlson DA, Lin Z, Rogers MC, Lin CY, Kahrilas PJ, Pandolfino JE (2015) Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil 27(7):981–989
Ata-Lawenko RM, Lee YY (2017) Emerging roles of the endolumenal functional lumen imaging probe in gastrointestinal motility disorders. J Neurogastroenterol Motil 23(2):164–170
Chen JW, Rubenstein JH (2017) Esophagogastric junction distensibility assessed using the functional lumen imaging probe. World J Gastroenterol 23(7):1289–1297
Rona KA, Tatum JM, Zehetner J, Schwameis K, Chow C, Samakar K, Dobrowolsky A, Houghton CC, Bildzukewicz N, Lipham JC (2018) Hiatal hernia recurrence following magnetic sphincter augmentation and posterior cruroplasty: intermediate-term outcomes. Surg Endosc 32(7):3374–3379
Ayazi S, Zheng P, Zaidi AH, Chovanec K, Chowdhury N, Salvitti M, Komatsu Y, Omstead AN, Hoppo T, Jobe BA (2020) Magnetic sphincter augmentation and postoperative dysphagia: characterization, clinical risk factors, and management. J Gastrointest Surg 24(1):39–49
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Min P Kim is consultant for Veran, Intuitive Surgical and Medtronic. Edward Chan is consultant for Veran. Ugoeze Nwokedi, Duc T. Nguyen, Leonora M. Meisenbach, Ray Chihara and Edward A. Graviss does not have any conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nwokedi, U., Nguyen, D.T., Meisenbach, L.M. et al. Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc 35, 3840–3849 (2021). https://doi.org/10.1007/s00464-020-07788-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07788-x