Abstract
Background
The repetitive and forceful motions used by operating surgeons increase the risk of developing musculoskeletal disorders. Most ergonomists consider the surgical environment to be incredibly harsh for its workers. Traditional Laparoscopic Surgery (TLS) in particular has a number of physical and mental challenges associated with it, and while Robotic-Assisted Laparoscopic Surgery (RALS) provides several features that improve upon TLS, some surgeons have still reported musculoskeletal symptoms they attribute to RALS. In this paper, we endeavored to systematically review muscle activation for both TLS and RALS, to compare the modalities and present the results as a meta-analysis.
Methods
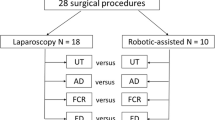
A literature search was conducted using Pubmed, Embase, and Cochrane databases in November 2018 with the following inclusion criteria: full text was available in English, the paper contained original data, EMG was one of the primary measurement techniques, and the paper included EMG data for both TLS and RALS. Results from studies were compared using standardized mean difference analysis.
Results
A total of 379 papers were found, and through screening ten were selected for inclusion. Sample populations ranged from 1 to 31 surgeons, and a variety of study designs and metrics were used between studies. The biceps were the only muscle group that consistently and significantly demonstrated lower muscle activation for RALS for all included studies.
Conclusions
The results may support the belief that RALS is ergonomically superior to TLS, shown through generally lower muscle activation scores. However, these results must be interpreted with caution due to the heterogeneity between the studies and multiple potential sources for bias within studies. This analysis would be strengthened with a higher number of homogenous, high-quality studies examining larger sample sizes.


Similar content being viewed by others
References
Epstein S, Sparer EH, Tran BN, Ruan QZ, Dennerlein JT, Singhal D, Lee BT (2018) Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg 153(2):e174947
Davis WT, Fletcher SA, Guillamondegui OD (2014) Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res 189(2):207–212 e6
Quinn D, Moohan J (2015) Optimal laparoscopic ergonomics in gynaecology. Obstet Gynecol 17:77–82
Sari V, Nieboer TE, Vierhout ME, Stegeman DF, Kluivers KB (2010) The operation room as a hostile environment for surgeons: physical complaints during and after laparoscopy. Minim Invasive Ther Allied Technol 19(2):105–109
Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D (2010) Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 210(3):306–313
Gutierrez-Diez MC, Benito-Gonzalez MA, Sancibrian R, Gandarillas-Gonzalez MA, Redondo-Figuero C, Manuel-Palazuelos JC (2018) A study of the prevalence of musculoskeletal disorders in surgeons performing minimally invasive surgery. Int J Occup Saf Ergon 24(1):111–117
van’t Hullenaar CDP, Hermans B, Broeders IA (2017) Ergonomic assessment of the da Vinci console in robot-assisted surgery. Innov Surg Sci 2(2):97–104
Franasiak J, Craven R, Mosaly P, Gehrig PA (2014) Feasibility and acceptance of a robotic surgery ergonomic training program. JSLS 18(4):e2014.00166
Giberti C, Gallo F, Francini L, Signori A, Testa M (2014) Musculoskeletal disorders among robotic surgeons: a questionnaire analysis. Arch Ital Urol Androl 86(2):95–98
Halim I, Omar AR, Saman AM, Othman I (2012) Assessment of muscle fatigue associated with prolonged standing in the workplace. Saf Health Work 3(1):31–42
Thorn S, Søgaard K, Kallenberg L, Sandsjö L, Sjøgaard G, Hermens H, Kadefors R, Forsman M (2007) Trapezius muscle rest time during standardised computer work—a comparison of female computer users with and without self-reported neck/shoulder complaints. J Electromyogr Kinesiol 17(4):420–427
Lee G, Lee T, Dexter D, Klein R, Park A (2007) Methodological infrastructure in surgical ergonomics: a review of tasks, models, and measurement systems. Surg Innov 14(3):153–167
Emam TA, Frank TG, Hanna GB, Cuschieri A (2001) Influence of handle design on the surgeon’s upper limb movements, muscle recruitment, and fatigue during endoscopic suturing. Surg Endosc 15(7):667–672
Konrad P (2005) The ABC of EMG: a practical introduction to kinesiological electromyography. Noraxon, United States
Seth D (2016) Contribution to the evaluation of muscle fatigue model and recovery model. Ecole Centrale de Nantes (ECN), France
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
National Heart, Lung, and Blood Institute (NHLBI) (2017) Quality assessment tool for observational cohort and cross-sectional studies. National Institute of Health
WebPlotDigitizer, Version 4.1, 2018, Ankit Rohagti, San Francisco
Review Manager (RevMan), Version 5.3, 2014, The Cochrane Collaboration, Copenhagen
Armijo PR, Huang CK, High R, Leon M, Siu KC, Oleynikov D (2018) Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc. https://doi.org/10.1007/s00464-018-6515-3
Berguer R, Smith W (2006) An ergonomic comparison of robotic and laparoscopic technique: the influence of surgeon experience and task complexity. J Surg Res 134:87–92
Dalsgaard T, Jensen MD, Hartwell D, Mosgaard BJ, Jorgensen A, Jensen BR (2018) Robotic surgery is less physically demanding than laparoscopic surgery: paired cross sectional study. Ann Surg. https://doi.org/10.1097/SLA.0000000000002845
González-Sánchez M, González-Poveda I, Mera-Velasco S, Cuesta-Vargas AI (2017) Comparison of fatigue accumulated during and after prolonged robotic and laparoscopic surgical methods: a cross-sectional study. Surg Endosc 31(3):1119–1135
Hubert N, Gilles M, Desbrosses K, Meyer JP, Felblinger J, Hubert J (2013) Ergonomic assessment of the surgeon’s physical workload during standard and robotic assisted laparoscopic procedures. Int J Med Robot 9(2):142–147
Lee GI, Lee MR, Clanton T, Sutton E, Park AE, Marohn MR (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28(2):456–465
Szeto GP, Poon JT, Law WL (2013) A comparison of surgeon’s postural muscle activity during robotic-assisted and laparoscopic rectal surgery. J Robot Surg 7(3):305–308
Zárate Rodriguez JG, Zihni AM, Ohu I, Cavallo JA, Ray S, Cho S, Awad MM (2018) Ergonomic analysis of laparoscopic and robotic surgical task performance at various experience levels. Surg Endosc. https://doi.org/10.1007/s00464-018-6478-4
Zihni AM, Ohu I, Cavallo JA, Ousley J, Cho S, Awad MM (2014) FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc 28(8):2459–2465
Zihni AM, Ohu I, Cavallo JA, Cho S, Awad MM (2014) Ergonomic analysis of robot-assisted and traditional laparoscopic procedures. Surg Endosc 28(12):3379–3384
Freschi C, Ferrari V, Melfi F, Ferrari M, Mosca F, Cuschieri A (2013) Technical review of the da Vinci surgical telemanipulator. Int J Med Robot 9(4):396–406
Dalager T, Søgaard K, Bech KT, Mogensen O, Jensen PT (2017) Musculoskeletal pain among surgeons performing minimally invasive surgery: a systematic review. Surg Endosc 31(2):516–526
Hallbeck MS, Lowndes BR, Bingener J, Abdelrahman AM, Yu D, Bartley A, Park AE (2017) The impact of intraoperative microbreaks with exercises on surgeons: a multi-center cohort study. Appl Ergon 60:334–341
Matern U, Kuttler G, Giebmeyer C, Waller P, Faist M (2004) Ergonomic aspects of five different types of laparoscopic instrument handles under dynamic conditions with respect to specific laparoscopic tasks: an electromyographic-based study. Surg Endosc 18(8):1231–1241
Bosma J, Boeken Kruger A, Jaspers J (2015) A novel, intuitive instrument positioner for endoscopy, involving surgeons in design and feasibility. Minim Invasiv Ther 24(6):326–333
von Hippel PT (2015) The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Med Res Methodol 15:35
Borenstein M, Hedges LV, Higgins JP, Rothstein HR (2011) Introduction to meta-analysis. Wiley, United States
Marín-Martínez F, Sánchez-Meca J (1999) Averaging dependent effect sizes in meta-analysis: a cautionary note about procedures. Span J Psychol 2:32–38
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
J Hislop has received Grant funding from Mulgrave Private Hospital and Healthe Care during the course of this study. Dr. Isaksson reports grants from IR Robotics Pty Ltd, for unrelated studies. Authors Dr. Tirosh, Dr. McCormick, Prof. Nagarajah, and Mr. Hensman have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hislop, J., Tirosh, O., McCormick, J. et al. Muscle activation during traditional laparoscopic surgery compared with robot-assisted laparoscopic surgery: a meta-analysis. Surg Endosc 34, 31–38 (2020). https://doi.org/10.1007/s00464-019-07161-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07161-7