Abstract
Background
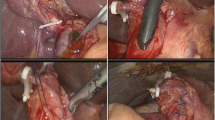
Although laparoscopic common bile duct exploration (LCBDE) has shown many obvious advantages compared with open surgery in the treatment of common bile duct (CBD) stones, it remains unclear regarding risk factors of conversion from LCBDE to open surgery and whether conversion will counteract the advantages of LCBDE. The purpose of this study was to explore risk factors and consequences of conversion from LCBDE to open surgery.
Methods
A retrospective study was conducted, using a database of 644 patients with LCBDE between 2011 and 2017. Risk factors for conversion to open surgery were determined based on univariable and multivariable analysis. The consequences of conversion to open surgery in LCBDE were analyzed.
Results
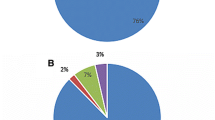
Conversion was required in 27 (4.2%) of 644 patients undergoing LCBDE. Independent risk factors for conversion were as follows: the max diameter of stones in CBD (odds ratio (OR) 2.234, 95%CI 1.031–4.842; p = 0.042), edema of CBD (OR 12.530, 95%CI 4.633–33.887; p < 0.001), and multiple stones in CBD (OR 3.438, 95%CI: 1.133–10.428; p = 0.029). These risk factors and their combined were good predictors for conversion in LCBDE. More blood loss, longer operative time, longer postoperative hospital stay, and higher incision infection were identified in patients with conversion than those without conversion. However, no significant differences were observed regarding mortality, readmission within 30 days, reoperation, bile leakage, and intra-abdominal fluid collection.
Conclusion
Conversion to open surgery in LCBDE was associated with acute edematous CBD with large and multiple stones. Conversion can offset the advantages of LCBDE.



Similar content being viewed by others
Abbreviations
- LCBDE:
-
Laparoscopic common bile duct exploration
- LCBDE-PC:
-
Laparoscopic common bile duct exploration with primary closure
- LTCBDE:
-
Laparoscopic transcystic common bile duct exploration
- LC:
-
Laparoscopic cholecystectomy
- PC:
-
Primary closure
- PS:
-
Propensity score
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- EST:
-
Endoscopic sphincterotomy
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- MD:
-
Mean difference
- CBD:
-
Common bile duct
- ROC:
-
Receiver operating characteristic
References
Gupta N (2016) Role of laparoscopic common bile duct exploration in the management of choledocholithiasis. World J Gastrointest Surg 8:376–381
Wen SQ, Hu QH, Wan M, Tai S, Xie XY, Wu Q, Yang SL, Liao GQ (2017) Appropriate patient selection is essential for the success of primary closure after laparoscopic common bile duct exploration. Dig Dis Sci
Lee HM, Min SK, Lee HK (2014) Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center. Ann Surg Treat Res 86:1–6
Zhu HY, Xu M, Shen HJ, Yang C, Li F, Li KW, Shi WJ, Ji F (2015) A meta-analysis of single-stage versus two-stage management for concomitant gallstones and common bile duct stones. Clin Res Hepatol Gastroenterol 39:584–593
Mattila A, Mrena J, Kellokumpu I (2017) Cost-analysis and effectiveness of one-stage laparoscopic versus two-stage endolaparoscopic management of cholecystocholedocholithiasis: a retrospective cohort study. BMC Surg 17:79
Tranter SE, Thompson MH (2002) Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg 89:1495–1504
Savita KS, Bhartia VK (2010) Laparoscopic CBD Exploration. Indian J Surg 72:395–399
Goonawardena J, Gunnarsson R, de Costa A (2015) Predicting conversion from laparoscopic to open cholecystectomy presented as a probability nomogram based on preoperative patient risk factors. Am J Surg 210:492–500
Sutcliffe RP, Hollyman M, Hodson J, Bonney G, Vohra RS, Griffiths EA, CholeS study group WMRC (2016) Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective U.K. database of 8820 patients. HPB 18:922–928
Vivek MA, Augustine AJ, Rao R (2014) A comprehensive predictive scoring method for difficult laparoscopic cholecystectomy. J Minimal Access Surg 10:62–67
Hua J, Lin S, Qian D, He Z, Zhang T, Song Z (2015) Primary closure and rate of bile leak following laparoscopic common bile duct exploration via choledochotomy. Dig Surg 32:1–8
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Buchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, Hunter JG (2003) Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg 237:460–469
Tazuma S, Unno M, Igarashi Y, Inui K, Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, Ryozawa S, Nimura Y, Fujita N, Kubota K, Shoda J, Tabata M, Mine T, Sugano K, Watanabe M, Shimosegawa T (2017) Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol 52:276–300
Prasson P, Bai X, Zhang Q, Liang T (2016) One-stage laproendoscopic procedure versus two-stage procedure in the management for gallstone disease and biliary duct calculi: a systemic review and meta-analysis. Surgical endoscopy 30:3582–3590
Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC (2004) A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg 239:28–33
Noble H, Whitley E, Norton S, Thompson M (2011) A study of preoperative factors associated with a poor outcome following laparoscopic bile duct exploration. Surg Endosc 25:130–139
Sippey M, Grzybowski M, Manwaring ML, Kasten KR, Chapman WH, Pofahl WE, Pories WJ, Spaniolas K (2015) Acute cholecystitis: risk factors for conversion to an open procedure. J Surg Res 199:357–361
Randhawa JS, Pujahari AK (2009) Preoperative prediction of difficult lap chole: a scoring method. Indian J Surg 71:198–201
Kaafarani HM, Smith TS, Neumayer L, Berger DH, Depalma RG, Itani KM (2010) Trends, outcomes, and predictors of open and conversion to open cholecystectomy in Veterans Health Administration hospitals. Am J Surg 200:32–40
Yang TF, Guo L, Wang Q (2014) Evaluation of preoperative risk factor for converting laparoscopic to open cholecystectomy: a meta-analysis. Hepato-Gastroenterol 61:958–965
Terho PM, Leppaniemi AK, Mentula PJ (2016) Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World J Emerg Surg WJES 11:54
Lee A, Min SK, Park JJ, Lee HK (2011) Laparoscopic common bile duct exploration for elderly patients: as a first treatment strategy for common bile duct stones. J Korean Surg Soc 81:128–133
Acknowledgements
This work was supported by the Scientific Research Foundation for the Returned Overseas Chinese Scholars, Chinese Ministry of Education, Shanghai Tenth Hospital’s improvement plan for NSFC (SYGZRPY2017004), and Natural Science Foundation of Shanghai (18ZR1429600).
Author information
Authors and Affiliations
Contributions
BX, Y-XW, and Y-XQ contributed equally to this work; XB, WZ, and Z-SS designed the research; BX, Y-XW, Y-XQ, H-BM, JG, WS, BZ, JH, TZ, Z-SS performed the research; BX, Y-XW, Y-XQ, and WZ collected and analyzed the data; BX, Y-XW, Z-SS, and Y-XQ wrote the paper.
Corresponding authors
Ethics declarations
Disclosures
Bin Xu, Yu-Xiang Wang, Yong-Xin Qiu, Hong-Bo Meng, Jian Gong, Wei sun, Bo Zhou, Jian He, Ti Zhang, Wen-Yan Zheng, and Zhen-Shun Song have no conflict of interests or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Xu, B., Wang, YX., Qiu, YX. et al. Risk factors and consequences of conversion to open surgery in laparoscopic common bile duct exploration. Surg Endosc 32, 4990–4998 (2018). https://doi.org/10.1007/s00464-018-6263-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6263-4