Abstract
Objective
Use of surgical energy is integral to laparoscopic surgery (LS). Energized dissection (ED) has a potential to impact the biomolecular expression of inflammation due to ED-induced collateral inflammation. We did this triple-blind randomized controlled (RCT) study to assess this biomolecular footprint in an index LS, i.e., laparoscopic cholecystectomy (LC).
Methods and procedures
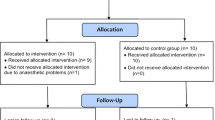
This RCT was conducted in collaboration with tertiary-level institutions, from January 2014 to December 2014 with institutional review board clearance. Consecutive, unselected, consenting candidates for LC were randomized (after anesthesia induction) into group I (ED) and group II (non-ED). They were managed with compliance to universal protocols for ethics, informed consent, anesthesia, drug usage and clinical pathway with blinded observers. Biomolecular inflammatory markers, i.e., interleukin 6 (IL-6), tumor necrosis factor-alpha (TNF-α) and highly sensitive CRP (HS-CRP), were measured with blood drawn juxta-preoperatively (H0), at 4 h (H4) and at 24 h (H24). The quantitative changes induced by ED on IL-6, TNF-α and HS-CRP at H0, H4 and H24 with their kinetic behavior were the study endpoint. Prospective data were analyzed statistically with a p value of <0.05 being significant.
Results
Two cases from the ED group had biliary injury and hence were withdrawn from analysis. The ED (n = 49) and non-ED (n = 51) groups had similar demographic, clinical and H0 biomolecular variables. There was a significant increase in IL-6, TNF-α and HS-CRP from H0 to H4 in both the groups (p values <0.001). From H4 to H24, all three cytokines showed significant increase in ED group (p < 0.05), whereas in the non-ED group, IL-6 showed significant fall (p = 0.004) and TNF-α showed no significant change (p = 0.063). Both the groups showed H4–H24 elevation of HS-CRP (p = 0.000).
Conclusion
Energized dissection adds to the cytokine-mediated postoperative inflammation. The additional ED-induced inflammation can be measured objectively by IL-6 and TNF-α levels.
Clinical trials registry
Clinical Trials Registry, India (REF/2014/06/007153).



Similar content being viewed by others
References
Agarwal BB, Agarwal S (2007) The man–machine interface, a paradox of technology. Is the black box (BB) concept an angel or a demon? Surg Endosc 21:1680
Sankaranarayanan G, Resapu RR, Jones DB, Schwaitzberg S, De S (2013) Common uses and cited complications of energy in surgery. Surg Endosc 27:3056–3072
Fuchshuber PR, Robinson TN, Feldman LS, Jones DB, Schwaitzberg SD (2014) The SAGES FUSE program: bridging a patient safety gap. Bull Am Coll Surg 99:18–27
Feldman LS, Fuchshuber P, Jones DB, Mischna J, Schwaitzberg SD, Force FT (2012) Surgeons don’t know what they don’t know about the safe use of energy in surgery. Surg Endosc 26:2735–2739
Madani A, Jones DB, Fuchshuber P, Robinson TN, Feldman LS (2014) Fundamental use of surgical energy™ (FUSE): a curriculum on surgical energy-based devices. Surg Endosc 28:2509–2512
Madani A, Watanabe Y, Vassiliou MC, Fuchshuber P, Jones DB, Schwaitzberg SD, Fried GM, Feldman LS (2014) Impact of a hands-on component on learning in the fundamental use of surgical energy™ (FUSE) curriculum: a randomized-controlled trial in surgical trainees. Surg Endosc 28:2772–2782
Chegini N (2002) Peritoneal molecular environment, adhesion formation and clinical implication. Front Biosci 1(7):e91–e115
Hildebrand F, Pape HC, Krettek C (2005) The importance of cytokines in the posttraumatic inflammatory reaction. Unfallchirurg 108(10):793–794, 796–803
Grande M, Tucci GF, Adorisio O, Barini A, Rulli F, Neri A, Franchi F, Farinon AM (2002) Systemic acute-phase response after laparoscopic and open cholecystectomy. Surg Endosc 16:313–316
Agarwal BB, Chintamani C (2011) Reminder of the metrics of endosurgical innovation. Arch Surg 146:1108
Brokelman WJ, Lensvelt M, Borel Rinkes IH, Klinkenbijl JH, Reijnen MM (2011) Peritoneal changes due to laparoscopic surgery. Surg Endosc 25:1–9
Agarwal BB, Agarwal N, Agarwal KA, Goyal K, Nanvati JD, Manish K, Pandey H, Sharma S, Ali K, Mustafa ST, Gupta MK, Saluja S, Agarwal S (2014) Outcomes of laparoscopic cholecystectomy done with surgical energy versus done without surgical energy: a prospective-randomized control study. Surg Endosc 28:3059–3067
Agarwal BB (2008) Outcomes in laparoscopic cholecystectomy (LS) done with or without using energy sources (ES): results of a prospective randomized controlled study. 2008 Scientific Session of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Philadelphia, Pennsylvania, USA, 9–12 April 2008. Surg Endosc 22:S224
Agarwal BB, Mahajan KC (2010) Laparoscopic biliary tract injury prevention: zero tolerance, error free performance. Surg Endosc 24:728–729
Agarwal KA, Tripathi CD, Agarwal BB, Saluja S (2011) Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surg Endosc 25:3805–3810
Agarwal BB (2010) Energized dissection, energized hemostasis. Arch Surg 145:1021
Agarwal BB (2007) Are energy sources required in laparoscopic cholecystectomy? Or should they be standby? Surg Endosc 21:1042
Agarwal BB, Gupta M, Agarwal S, Mahajan K (2007) Anatomical footprint for safe laparoscopic cholecystectomy without using any energy source: a modified technique. Surg Endosc 21:2154–2158
Agarwal BB, Gupta M, Agarwal S, Mahajan KC (2007) Laparoscopic cholecystectomy without using any energy source. J Laparoendosc Adv Surg Tech A 17:296–301
Agarwal BB (2010) Results of laparoscopic cholecystectomy without energized dissection: a prospective study. Int J Surg 8:167–172
Agarwal BB, Sinha B, Mahajan KC (2010) Double blind randomized control study-outcomes of laparoscopic cholecystectomy (without using energy source) performed by a trainee or a consultant. 17th International Congress of the European association for endoscopic surgery (EAES) Prague, Czech Republic, 17–20 June 2009. Surg Endosc 24:S37
Agarwal BB, Jayaraman L, Mishra A, Sarangi R, Mahajan KC (2010) Clinical outcomes of laparoscopic cholecystectomy (without energised dissection) performed by a basic surgical trainee or a consultant-double blind randomized control study. 2010 Scientific session of the society of American gastrointestinal and endoscopic surgeons (SAGES) National Harbor, Maryland, USA, 14–17 April 2010. Surg Endosc 24:S580
Agarwal BB, Gupta MK, Agarwal S, Mahajan KC (2007) Avoiding any energy source for a safe and better laparoscopic cholecystectomy. 2007 Scientific session of the society of American gastrointestinal and endoscopic surgeons (SAGES) Las Vegas, Nevada, USA, 18–22 April 2007. Surg Endosc 21:S443
Agarwal BB, Agarwal S, Gupta MK, Agarwal N, Agarwal D, Goyal K, Saluja S, Mahajan KC, Agarwal KA, Pandey H (2013) Evaluation of avascular ‘‘holy plane’’ based cold dissection technique in consecutive unselected laparoscopic cholecystectomies: results of 7 year experience. 2013 Scientific session of the society of American gastrointestinal and endoscopic surgeons (SAGES) Baltimore, Maryland, USA, 17–20 April 2013. Surg Endosc 27:S396
Agarwal BB (2008) Journey of the carbon-literate and climate conscious endosurgeon having a head, heart, hands, and holistic sense of responsibility. Surg Endosc 22:2539–2540
Agarwal BB, Chintamani AK, Goyal K, Mahajan KC (2012) Innovations in Endosurgery: journey into the past of the future. To ride the sils bandwagon or not? Indian J Surg 74:234–241
Agarwal BB (2009) Patient safety in laparoscopic cholecystectomy. Arch Surg 144:979
Agarwal BB, Agarwal S, Gupta M, Mahajan K (2008) Transaxillary endoscopic excision of benign breast lumps: a new technique. Surg Endosc 22:407–410
Park K (2013) Park’s textbook of preventive and social medicine, 22nd edn. M/s Banarsidas Bhanot Publishers, Jabalpur
Fingerhut A, Dziri C, Garden OJ, Gouma D, Millat B, Neugebauer E, Paganini A, Targarona E (2013) ATOM, the all-inclusive, nominal EAES classification of bile duct injuries during cholecystectomy. Surg Endosc 27:4608–4619
Feldman LS, Delaney CP (2014) Laparoscopy plus enhanced recovery: optimizing the benefits of MIS through SAGES ‘SMART’ program. Surg Endosc 28:1403–1406
Agarwal BB (2009) Informed consent-‘da Vinci code’ for our safety in empowered patient’s safety. Surg Endosc 23:1158–1160
Agarwal BB (2011) Do dietary spices impair the patient-reported outcomes for stapled hemorrhoidopexy? A randomized controlled study. Surg Endosc 25:1535–1540
Mascher B, Schlenke P, Seyfarth M (1999) Expression and kinetics of cytokines determined by intracellular staining using flow cytometry. J Immunol Methods 223:115–121
Oliver JC, Bland LA, Oettinger CW, Arduino MJ, McAllister SK, Aguero SM, Favero MS (1993) Cytokine kinetics in an in vitro whole blood model following an endotoxin challenge. Lymphokine Cytokine Res 12:115–120
Sendt W, Amberg R, Schöffel U, Hassan A, von Specht BU, Farthmann EH (1999) Local inflammatory peritoneal response to operative trauma: studies on cell activity, cytokine expression, and adhesion molecules. Eur J Surg 165:1024–1030
Rohleder N, Aringer M, Boentert M (2012) Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci 1261:88–96
Choileain NN, Redmond HP (2006) Cell response to surgery. Arch Surg 141:1132–1140
Benedict C, Scheller J, Rose-John S, Born J, Marshall L (2009) Enhancing influence of intranasal interleukin-6 on slow-wave activity and memory consolidation during sleep. FASEB J 23:3629–3636
Agarwal KA, Agarwal BB, Mahajan KC (2010) Carbon footprint of laparoscopic cholecystectomy performed with or without energized dissection: a case controlled study. 2010 Scientific Session of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) National Harbor, Maryland, USA, 14–17 April 2010. Surg Endosc 24:S590
Acknowledgments
This work was a continuation of our earlier studies. This started with blessings and guidance of Prof. Krishan C Mahajan. He was the founder chairman of our institution and the discipline of surgery in North India after Indian independence. He was very keen to see the conclusion of this study but left us at age 92 in January 2015 after continuously monitoring the present study till his last days. We dedicate this work to his memory. We thank Dr. Manoj Modi, a neonatologist in our institution for helping us with statistics. We are grateful to Ms Pooja and Ms Ramneek for preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Brij B. Agarwal, Juhil D. Nanavati, Nayan Agarwal, Naveen Sharma, Krishna A. Agarwal, Kumar Manish, Satish Saluja and Sneh Agarwal have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Agarwal, B.B., Nanavati, J.D., Agarwal, N. et al. Biomolecular inflammatory response to surgical energy usage in laparoscopic surgery: results of a randomized study. Surg Endosc 30, 1733–1741 (2016). https://doi.org/10.1007/s00464-015-4408-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4408-2