Abstract
Background
In patients presenting with acute diverticulitis (AD) and signs of acute peritonitis, the presence of extradigestive air (EDA) on a computer tomography (CT) scan is often considered to indicate the need for emergency surgery. Although the traditional management of “perforated” AD is open sigmoidectomy, more recently, laparoscopic drainage/lavage (usually followed by delayed elective sigmoidectomy) has been reported. The aim of this retrospective study is to evaluate the results of nonoperative management of emergency patients presenting with AD and EDA.
Methods
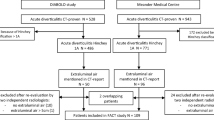
The outcomes of 39 consecutive hemodynamically stable patients (23 men, mean age = 54.7 years) who were admitted with AD and EDA and were managed nonoperatively (antibiotic and supportive treatment) at a tertiary-care university hospital between January 2001 and June 2010 were retrospectively collected and analyzed. These included morbidity (Clavien-Dindo) and treatment failure (need for emergency surgery or death). A univariate analysis of clinical, radiological, and laboratory criteria with respect to treatment failure was performed. Results of delayed elective laparoscopic sigmoidectomy were also analyzed.
Results
There was no mortality. Thirty-six of the 39 patients (92.3%) did not need surgery (7 patients required CT-guided abscess drainage). Mean hospital stay was 8.1 days. Duration of symptoms, previous antibiotic administration, severe sepsis, PCR level, WBC concentration, and the presence of abdominal collection were associated with treatment failure, whereas “distant” location of EDA and free abdominal fluid were not. Five patients had recurrence of AD and were treated medically. Seventeen patients (47.2%) underwent elective laparoscopic sigmoidectomy for which mean operative time was 246 min (range = 100–450) and the conversion rate was 11.8%. Mortality was nil and the morbidity rate was 41.2%. Mean postoperative stay was 7.1 days (range = 4–23).
Conclusions
Nonoperative management is a viable option in most emergency patients presenting with AD and EDA, even in the presence of symptoms of peritonitis or altered laboratory tests. Delayed laparoscopic sigmoidectomy may be useless in certain cases and its results poorer than expected.



Similar content being viewed by others
References
Wong WD, Wexner SD, Lowry A, Vernava A 3rd, Burnstein M, Denstman F, Fazio V, Kerner B, Moore R, Oliver G, Peters W, Ross T, Senatore P, Simmang C (2000) Practice parameters for the treatment of sigmoid diverticulitis—supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons. Dis Colon Rectum 43:290–297
Etzioni DA, Chiu VY, Cannom RR, Burchette RJ, Haigh PI, Abbas MA (2010) Outpatient treatment of acute diverticulitis: rates and predictors of failure. Dis Colon Rectum 53:861–865
Welch CE, Allen AW, Donaldson GA (1953) An appraisal of resection of the colon for diverticulitis of the sigmoid. Ann Surg 138:332–343
Roberts P, Abel M, Rosen L, Cirocco W, Fleshman J, Leff E, Levien D, Pritchard T, Wexner S, Hicks T (1995) Practice parameters for sigmoid diverticulitis. The Standards Task Force American Society of Colon and Rectal Surgeons. Dis Colon Rectum 38:125–132
Kozak LJ, DeFrances CJ, Hall MJ (2006) National hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat 13(162):1–209
Chapman J, Davies M, Wolff B, Dozois E, Tessier D, Harrington J, Larson D (2005) Complicated diverticulitis: is it time to rethink the rules? Ann Surg 242:576–581
Schwesinger WH, Page CP, Gaskill HV 3rd, Steward RM, Chopra S, Strodel WE, Sirinek KR (2000) Operative management of diverticular emergencies: strategies and outcomes. Arch Surg 135:558–562
Biondo S, Ramos E, Deiros M, Ragué JM, De Oca J, Moreno P, Farran L, Jaurrieta E (2000) Prognostic factors for mortality in left colonic peritonitis: a new scoring system. J Am Coll Surg 191:635–642
Chandra V, Nelson H, Larson DR, Harrington JR (2004) Impact of primary resection on the outcome of patients with perforated diverticulitis. Arch Surg 139:1221–1224
Schilling MK, Maurer CA, Kollmar O, Büchler MW (2001) Primary vs. secondary anastomosis after sigmoid colon resection for perforated diverticulitis (Hinchey Stage III and IV): a prospective outcome and cost analysis. Dis Colon Rectum 44:699–703
Salem L, Flum DR (2004) Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Dis Colon Rectum 47:1953–1964
Belmonte C, Klas JV, Perez JJ, Wong WD, Rothenberger DA, Goldberg SM, Madoff RD (1996) The Hartmann procedure. First choice or last resort in diverticular disease? Arch Surg 131:612–615
O’Sullivan GC, Murphy D, O’Brien MG, Ireland A (1996) Laparoscopic management of generalized peritonitis due to perforated colonic diverticula. Am J Surg 171:432–434
Myers E, Hurley M, O’Sullivan GC, Kavanagh D, Wilson I, Winter DC (2008) Laparoscopic peritoneal lavage for generalized peritonitis due to perforated diverticulitis. Br J Surg 95:97–101
Karoui M, Champault A, Pautrat K, Valleur P, Cherqui D, Champault G (2009) Laparoscopic peritoneal lavage or primary anastomosis with defunctioning stoma for Hinchey 3 complicated diverticulitis: results of a comparative study. Dis Colon Rectum 52:609–615
Pradel JA, Adell JF, Taourel P, Djafari M, Monnin-Delhom E, Bruel JM (1997) Acute colonic diverticulitis: prospective comparative evaluation with US and CT. Radiology 205:503–512
Ambrosetti P, Jenny A, Becker C, Terrier TF, Morel P (2000) Acute left colonic diverticulitis—compared performance of computed tomography and water-soluble contrast enema: prospective evaluation of 420 patients. Dis Colon Rectum 43:1363–1367
Ritz JP, Lehmann KS, Loddenkemper C, Frericks B, Buhr HJ, Holmer C (2010) Preoperative CT staging in sigmoid diverticulitis—does it correlate with intraoperative and histological findings? Langenbecks Arch Surg 395:1009–1015
Kaiser AM, Jiang JK, Lake JP, Ault G, Artinyan A, Gonzalez-Ruiz C, Essani R, Beart RW Jr (2005) The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol 100:910–917
Schug-Pass C, Geers P, Hügel O, Lippert H, Köckerling F (2010) Prospective randomized trial comparing short-term antibiotic therapy versus standard therapy for acute uncomplicated sigmoid diverticulitis. Int J Colorectal Dis 25:751–759
Pittet O, Kotzampassakis N, Schmidt S, Denys A, Demartines N, Calmes JM (2009) Recurrent left colonic diverticulitis episodes: more severe than the initial diverticulitis? World J Surg 33:547–552
Hachigian MP, Honickman S, Eisenstat TE, Rubin RJ, Salvati EP (1992) Computed tomography in the initial management of acute left-sided diverticulitis. Dis Colon Rectum 35:1123–1129
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Jacobs DO (2007) Clinical practice. Diverticulitis. N Engl J Med 357:2057–2066
Durmishi Y, Gervaz P, Brandt D, Bucher P, Platon A, Morel P, Poletti PA (2006) Results from percutaneous drainage of Hinchey stage II diverticulitis guided by computed tomography scan. Surg Endosc 20:1129–1133
Siewert B, Tye G, Kruskal J, Sosna J, Opelka F, Raptopoulos V, Goldberg SN (2006) Impact of CT-guided drainage in the treatment of diverticular abscesses: size matters. Am J Roentgenol 186:680–686
Tabbara M, Velmahos GC, Butt MU, Chang Y, Spaniolas K, Demoya M, King DR, Alam HB (2010) Missed opportunities for primary repair in complicated acute diverticulitis. Surgery 148:919–924
Heverhagen JT, Sitter H, Zielke A, Klose KJ (2008) Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum 51:1810–1815
Buckley O, Geoghegan T, O’Riordain DS, Lyburn ID, Torreggiani WC (2004) Computed tomography in the imaging of colonic diverticulitis. Clin Radiol 59:977–983
Bosscha K, Reijnders K, Hulstaert PF, Algra A, van der Werken C (1997) Prognostic scoring systems to predict outcome in peritonitis and intra-abdominal sepsis. Br J Surg 84:1532–1534
Franklin ME Jr, Portillo G, Treviño JM, Gonzalez JJ, Glass JL (2008) Long-term experience with the laparoscopic approach to perforated diverticulitis plus generalized peritonitis. World J Surg 32:1507–1511
Hjern F, Josephson T, Altman D, Holmström B, Mellgren A, Pollack J, Johansson C (2007) Conservative treatment of acute colonic diverticulitis: are antibiotics always mandatory? Scand J Gastroenterol 42:41–47
Kaewlai R, Nazinitsky KJ (2007) Acute colonic diverticulitis in a community-based hospital: CT evaluation in 138 patients. Emerg Radiol 13:171–179
Alamili M, Gögenur I, Rosenberg J (2009) Acute complicated diverticulitis managed by laparoscopic lavage. Dis Colon Rectum 52:1345–1349
Taylor CJ, Layani L, Ghusn MA, White SI (2006) Perforated diverticulitis managed by laparoscopic lavage. ANZ J Surg 76:962–965
Disclosures
Doctors Renato Costi, François Cauchy, Alban Le Bian, Jean-François Honart, Nicolas Creuze, and Professor Claude Smadja have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costi, R., Cauchy, F., Le Bian, A. et al. Challenging a classic myth: pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery in hemodynamically stable patients. A 10-year experience with a nonoperative treatment. Surg Endosc 26, 2061–2071 (2012). https://doi.org/10.1007/s00464-012-2157-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2157-z