Abstract
Background
Intrathoracic wrap migration is the most frequent morphological anatomic reason for failure of laparoscopic antireflux surgery (LARS). This study investigates whether the size of the esophageal hiatus is a factor in reherniation after LARS with mesh hiatoplasty and after primary failed hiatal closure.
Methods
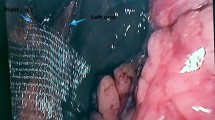
Fifty-four patients who underwent a laparoscopic 270° Toupet fundoplication with simple sutured crura and posterior onlay of ParietexTM mesh prosthesis between October 2003 and June 2008 were evaluated with respect to the occurrence of postoperative intrathoracic wrap migration/reherniation. Indication for mesh hiatoplasty was a hiatus with a hiatal surface area (HSA) of at least 5.60 cm2 or slippage after the first LARS. The integrity of repair was assessed using a barium swallow test. Cinematography was performed at a median of 25.6 months (3–63 months after operation) and was completed in 49 of 54 patients (90%). Follow-up was completed in 24 patients who underwent primary LARS (group A) and 25 patients who underwent a laparoscopic refundoplication (group B).
Results
In group A, the occurrence of postoperative wrap reherniation was diagnosed in 20.8% of the patients, compared to 40% in group B. In both groups only one patient with recurrent hiatal hernia was symptomatic. In group A, patients who developed a recurrent hernia had a larger HSA than patients without postoperative reherniation. There was a huge difference in the size of the HSA between symptomatic and asymptomatic patients with reherniation. In comparison, group B patients had HSA of similar size in all described cases.
Conclusion
In primary intervention, recurrence of hiatal hernia is more likely the larger the HSA is. The size of the hiatus is a major contributing factor to the possibility of reherniation. After failed primary hiatal closure, the size of the hiatal defect is no marker for the possibility of reherniation.








Similar content being viewed by others
References
Terry M, Smith CD, Branum GD, Galloway K, Waring JP, Hunter JG (2001) Outcomes of laparoscopic fundoplication for gastroesophageal reflux disease and paraesophageal hernia: experience with 1000 consecutive cases. Surg Endosc 15:691–699
Lafullarde T, Watson DI, Jamieson GG, Myers JC, Game PA, Devitt PG (2001) Laparoscopic Nissen fundoplication; five year result and beyond. Arch Surg 136:180–184
Granderath FA, Kamolz T, Schweiger UM, Pointner R (2002) Quality of life, surgical outcome and patient satisfaction three years after laparoscopic Nissen fundoplication. World J Surg 26:1234–1238
Kamolz T, Granderath FA, Bammer T, Pasiut M, Wykypiel H Jr, Herrmann R, Pointner R (2002) Mid- and long term quality of life assessments after laparoscopic fundoplication and refundoplication: a prospective single unit review of 500 antireflux procedures. Dig Liver Dis 34:470–476
Rieger NA, Jamieson GG, Britten-Jones R, Tew S (1994) Reoperation after failed antireflux surgery. Br J Surg 81:1159–1161
Soper NJ, Dunnegan D (1999) Anatomic fundoplication failure after laparoscopic antireflux surgery. Ann Surg 229:669–677
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10, 735 reported cases. J Am Coll Surg 193:428–439
Pointner R, Granderath FA (2008) Laparoscopic fundoplication: when, how and what to do if it fails? Eur Surg 40:261–269
Basso N, De Leo A, Genco A, Rosato P, Rea S, Spaziani E, Primavera A (2000) 360° laparoscopic fundoplication with tension-free hiatoplasty in treatment of symptomatic gastroesophageal reflux disease. Surg Endosc 14:164–169
Carlson MA, Richards CG, Franzides CT (1999) Laparoscopic prosthetic reinforcement of hiatal herniorrhaphy. Dig Surg 16:407–410
Frantzides CT, Richards CG, Carlson MA (1999) Laparoscopic repair of large hiatal hernia with polytetrafluoroethylene. Surg Endosc 13:906–908
Champion JK, Rock D (2003) Laparoscopic mesh cruroplasty for large paraesophageal hernias. Surg Endosc 17:551–553
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, Bremner CG (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190:553–560
Johnson JM, Carbonell AM, Carmody BJ, Jamal MK, Maher JW, Kellum JM, DeMaria EJ (2006) Laparoscopic mesh hiatoplasty for paraesophageal hernias and fundoplications: a critical analysis of available literature. Surg Endosc 20:362–366
Granderath FA, Carlson MA, Champion JK, Szold A, Basso N, Pointner R, Frantzides CT (2006) Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20:367–379
Soricelli E, Basso N, Genco A, Cipriano M (2009) Long-term results of hiatal hernia mesh repair and antireflux laparoscopic surgery. Surg Endosc 23(11):2499–2504
Pointner R, Granderath FA (2008) Hiatus hernia and recurrence: the Achilles heel of antireflux surgery? Chirurg 79:974–981
Williamson WA, Ellis FHJ, Streitz JMJ, Shahian DM (1993) Paraesophageal hiatal hernia: is an antireflux procedure necessary? Ann Thorac Surg 56:447–451
Gordon C, Kang JY, Neild PJ, Maxwell JD (2004) The role of the hiatus hernia in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 20:719–732
Granderath FA (2007) Measurement of the esophageal hiatus by calculation of the hiatal surface area (HSA). Why, when and how? Surg Endosc 21:2224–2225
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21:542–548
Granderath FA, Schweiger UM, Kamolz T, Pasiut M, Haas CF, Pointner R (2002) Laparoscopic antireflux surgery with routine mesh hiatoplasty in the treatment of gastroesophageal reflux disease. J Gastrointest Surg 6:347–353
Pointner R, Bammer T, Then P, Kamolz T (1999) Laparoscopic refundoplications after failed antireflux surgery. Am J Surg 178:541–544
Granderath FA, Kamolz T, Schweiger UM, Pointner R (2006) Impact of laparoscopic Nissen fundoplication with hiatal closure on esophageal body motility: results of a prospective randomized trial. Arch Surg 141:625–632
Dodds WJ, Walter B (1977) Cannon lecture: current concepts of esophageal motor function: clinical implications for radiology. AJR Am J Roentgenol 128:549–561
Granderath FA, Granderath UM, Pointner R (2008) Laparoscopic revisional fundoplication with circular hiatal mesh prosthesis: the long-term results. World J Surg 32:999–1007
Carlson MA, Condon RE, Ludwig KA, Schulte WJ (1998) Management of intrathoracic stomach with polypropylene mesh prosthesis reinforced transabdominal hiatus hernia repair. J Am Coll Surg 187:227–230
Edelmann DS (1995) Laparoscopic paraesophageal hernia repair with mesh. Surg Laparosc Endosc 5:32–37
Trus TL, Bax T, Richardson WS, Branum GD, Mauren SJ, Swanstrom LL, Hunter JG (1997) Complications of laparoscopic paraesophageal hernia repair. J Gastrointest Surg 1:221–228
Casabella F, Sinanan M, Horgan S, Pellegrini CA (1996) Systematic use of gastric fundoplication in laparoscopic repair of paraesophageal hernias. Am J Surg 171:485–489
Shamiyeh A, Szabo K, Granderath FA (2010) The esophageal hiatus: what is the normal size? Surg Endosc 24(5):988–991
Lenglinger J, Izay B, Eisler M, Wrba F, Zacherl J, Prager G, Riegler FM (2009) Barrett’s esophagus: size of the problem and diagnostic value of a novel histopathology classification. Eur Surg 41:26–39
Lenglinger J, Riegler FM (2009) Selected commentary to “The position of the acid pocket as a major risk factor for acidic reflux in healthy subjects and GERD patients”. Eur Surg 41:234–240
Furnée EJ, Draaisma WA, Broeders IA, Gooszen HG (2009) Surgical reintervention after failed antireflux surgery: a systematic review of the literature. J Gastrointest Surg 13:1539–1549
Granderath FA, Kamolz T, Schweiger UM, Pointner R (2003) Laparoscopic refundoplication with prosthetic hiatal closure for recurrent hiatal hernia after primary failed antireflux surgery. Arch Surg 138:902–907
Swanstrom LL, Marcus DR, Galloway GQ (1996) Laparoscopic collis gastroplasty is the treatment of choice for the shortened esophagus. Am J Surg 171:477–481
Gastral OL, Hagen JA, Peters JH, Campos GM, Hashemi M, Theisen J, Bremner CG, DeMeester TR (1999) Short esophagus: analysis of predictors and clinical implications. Arch Surg 134:633–636
Mitiek MO, Andrade RS (2010) Giant hiatal hernia. Ann Thorac Surg 89:2168–2173
Fei L, del Genio G, Rossetti G, Sampaolo S, Moccia F, Trapani V, Cimmino M, del Genio A (2009) Hiatal hernia recurrence: surgical complication or disease? Electron microscope findings of the diaphragmatic pillars. J Gastrointest Surg 13:459–464
Jobe BA, Aye RW, Deveney CW, Domreis JS, Hill LD (2002) Laparoscopic management of giant type III hiatal hernia and short esophagus. Objective follow-up at three years. J Gastrointest Surg 6:181–188
Disclosures
Oliver Owen Koch, Kai Uwe Asche, Johannes Berger, Eva Weber, Frank Alexander Granderath, and Rudolph Pointner have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koch, O.O., Asche, K.U., Berger, J. et al. Influence of the size of the hiatus on the rate of reherniation after laparoscopic fundoplication and refundopilication with mesh hiatoplasty. Surg Endosc 25, 1024–1030 (2011). https://doi.org/10.1007/s00464-010-1308-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1308-3