Abstract
Background
Laparoscopic left lateral sectionectomy (LLS) has gained popularity in its use for benign and malignant tumors. This report describes the evolution of the authors’ experience using laparoscopic LLS for different indications including living liver donation.
Methods
Between January 2004 and January 2009, 37 consecutive patients underwent laparoscopic LLS for benign, primary, and metastatic liver diseases, and for one case of living liver donation. Resection of malignant tumors was indicated for 19 (51%) of the 37 patients.
Results
All but three patients (deceased due to metastatic cancer disease) are alive and well after a median follow-up period of 20 months (range, 8–46 months). Liver cell adenomas (72%) were the main indication among benign tumors, and colorectal liver metastases (84%) were the first indication of malignancy. One case of live liver donation was performed. Whereas 16 patients (43%) had undergone a previous abdominal surgery, 3 patients (8%) had LLS combined with bowel resection. The median operation time was of 195 min (range, 115–300 min), and the median blood loss was of 50 ml (range, 0–500 ml). Mild to severe steatosis was noted in 7 patients (19%) and aspecific portal inflammation in 11 patients (30%). A median free margin of 5 mm (range, 5–27 mm) was achieved for all cancer patients. The overall recurrence rate for colorectal liver metastases was of 44% (7 patients), but none recurred at the surgical margin. No conversion to laparotomy was recorded, and the overall morbidity rate was 8.1% (1 grade 1 and 2 grade 2 complications). The median hospital stay was 6 days (range, 2–10 days).
Conclusions
Laparoscopic LLS without portal clamping can be performed safely for cases of benign and malignant liver disease with minimal blood loss and overall morbidity, free resection margins, and a favorable outcome. As the ultimate step of the learning curve, laparoscopic LLS could be routinely proposed, potentially increasing the donor pool for living-related liver transplantation.
Similar content being viewed by others
The laparoscopic surgical approach to the liver has developed more slowly than laparoscopy used for other organs due to several factors including the risk of bleeding, gas embolism, doubts about the possibility of performing oncologic resections, and the risks of cell seeding. Lack of manual palpation (hand feedback), difficulty reproducing the standard maneuvers, and the control of unattended hemorrhage as in open surgery are the factors influencing worldwide diffusion of a laparoscopic approach to the liver. However, with the improvements in surgical instrumentation, many reports are describing a wide interest and acceptance of this technique claimed to be feasible and safe that yields decreased postoperative pain and disability, reduces hospital stay, and shortens patient recovery time.
Since its first successful description in 1996, left lateral sectionectomy (LLS) is one of the most anatomic resections in liver surgery and probably the most standardized laparoscopic approach to the liver [1–16]. Indeed, different pathologies are currently treated with this technique. In specialist centers, laparoscopic LLS is considered the gold standard approach for lesions in segments 2 and 3. It is proposed even for cirrhotic patients with portal hypertension.
A look at the literature shows that the major laparoscopic LLS series are in most cases retrospective and case–control studies. In these studies, the morbidity rate usually ranges from 0% to 22%. The conversion rate ranges from 0% and 11% (with higher rates in early experiences), and the mortality rate is approximately 0% (Table 1).
This study aimed to describe a single-center evolution of laparoscopic LLS performed in recent years without portal triad clamping and for different indications including live liver donation for pediatric transplantation. Assessment of morbidity and mortality, perioperative parameters, pathology reporting, and outcome analysis, especially for metastatic colorectal disease, are fully provided.
Patients and methods
Between January 2004 and January 2009, 622 liver resections were performed at the Ghent University Hospital. The laparoscopic approach was used for 110 cases (17.7%). Laparoscopic resection of Couinaud’s segments 2 and 3 (LLS) was performed for 37 (34%) of 110 patients. The mean patient age was of 53 ± 15 years (range, 29–77 years), and the male/female ratio was of 10/27. The American Society of Anesthesiology (ASA) score was 1 for 20 patients, 2 for 12 patients, and 3 for 5 patients.
The indications for resection were benign solid liver tumor (n = 17, 46%) and malignant tumor (n = 19, 54%) for patients represented primarily by colorectal liver metastases (CRLM). The evolution of the indication over time is depicted in Fig. 1. Previous abdominal surgery or liver resection was not considered an exclusion criterion for the laparoscopic approach. The details are summarized in Table 2. As the ultimate evolution of the surgical technique, we performed a laparoscopic living donor liver resection in a young mother to provide a transplant for her child with acute liver decompensation during the wait for a deceased donor liver graft.
After approval of the local institutional review board, all data were collected from a prospective liver resection database. The variables considered were sex, age, ASA score, indication for liver resection, histology of the native liver, number and size of the nodules, free margins on the cutting edge, operation time, blood loss, morbidity, and hospital stay. Tumor pathology was assessed together with the underlying liver tissue. Tumor-free margins, tumor size, and percentage of cell necrosis were prospectively recorded.
All procedures were performed under the direction of the same attending surgeon (R.T.). The indication for surgical treatment was determined during a multidisciplinary conference. The preoperative workup consisted of ultrasound liver evaluation for 30 patients (81%), angiography and computed tomography (CT) for 19 patients (51%), magnetic resonance imaging (MRI) for 32 patients (86%), and positron emission tomography (PET) and CT for 18 patients (49%).
Surgical technique
Laparoscopic LLS was performed with the patient in supine and 30° anti-Trendelenburg position, with the surgeon standing between the patient’s legs (French position). Basically, four trocars (one 5 mm, one 10 mm, and two 12 mm trocars) were inserted in the upper abdominal quadrant. Both 12-mm trocars were placed to allow insertion of a 30° optical device and the linear stapler. The 10-mm trocar was inserted for the harmonic scissors or surgical aspirator. The 5-mm (subxyphoidal) trocar was placed to allow irrigation and aspiration during surgery, and eventually to hang the liver when necessary (Fig. 2).
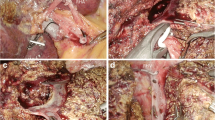
Carbon dioxide pneumoperitoneum was kept at about 10 mmHg. Assessment of the liver surface and surgical margins were performed routinely under intraoperative ultrasonographic guidance using the Aloka SSD 4000 (Aloka Co. Ltd., Tokyo, Japan). Laparoscopic LLS was performed without preparation of the liver hilum for portal triad clamping. The Harmonic scalpel (Ultracision; Ethicon Endosurgery, Cincinnati OH, USA) and surgical aspirator (CUSA Excel; Integra Life Science Ltd., IDA Business and Technology Park, Ireland) were used for parenchymal dissection (Fig. 3).
The operation started after dissection of eventual adhesions in the upper abdominal quadrant. Division of the round and falciform ligament toward the inferior vena cava was seldom performed and only to allow careful intraoperative ultrasonography guidance for lesions near Rex’s recessus or the left hepatic vein to assess surgical margins. The left triangular ligament was freed before parenchymal dissection was started, and the liver was transected on a line just left of the falciform ligament. Manipulation of tumoral lesions was systematically avoided in case of malignancy, and no cholecystectomy was required.
Once the intrahepatic portal pedicles were visualized, one or two vascular 45-mm linear staplers (EndoGIA; Ethicon) were applied. The final stage of the hepatectomy was performed without exposure of the left hepatic vein, which was stapled with a slim amount of surrounding parenchyma to avoid unnecessary injury. Hemostasis was performed through a combination technique including bipolar cautery and an argon beamer coagulator. In a few cases, titanium clips secured a hepatic vein draining a part of segment 2 through the middle hepatic vein.
The surgical specimen was extracted through a Pfannenstiel incision or a previous laparotomy incision using a plastic sterile bag. Drainage of the operative field was performed with a silastic drain (removed within 48–72 h) in all cases.
For laparoscopic living liver donation, modification of the technique essentially involved dissection behind the hilum to expose, free, and tape the left hepatic artery and the left portal vein. Small branches going to the caudate lobe were cut and secured by Hem-o-lock clips (TFX Medical Ltd., RTP Durham, NC, USA) to maximize the length of the left portal vein. When the dissection reached the hilar plate, the left biliary duct was cut with a straight scissors, and the proximal end was secured by a running suture (PDS 5/0).
After a Pfannestiel incision, a Gelport laparoscopic system (Applied Medical, Rancho Santa Margarita, CA, USA) was inserted to allow hand extraction of the graft. When 5,000 U of heparin had been given intravenously, the graft was procured as follows. With double Hem-o-lock clips on both hepatic arteries (Endo TA, 30 mm; Tyco Healthcare, Gosport PO130AS, UK) and on the left portal vein, the EndoGIA (45 mm) was used to secure and cut the left hepatic vein [17].
Statistical analysis
Results were expressed as median or mean ± standard deviation. Student’s t-test, the chi-square test, and the Mann–Whitney U test were used when appropriate. The statistical significance level was set at an alpha of 0.05. Statistical analysis was performed using SPSS 15.0 for the Windows program (SPSS, Chicago, IL, USA).
Results
The patient demographics and perioperative data are summarized on Table 2. At this writing, all patients but three are alive and well after a median follow-up period of 20 months (range, 8–46 months). Benign tumors were represented primarily by liver cell adenomas, whereas colorectal liver metastases (multiple in 36% of cases) were the main indication for malignancy. A history of abdominal surgery was recorded for 16 patients (43%), and laparoscopic LLS was proposed as a repeat hepatectomy for 7 patients (19%).
The overall median operation time (including anesthesia) was 195 min (range, 115–300 min). However, for three patients (8%) undergoing combined liver and bowel resection, the operation time was, as expected, longer (300 vs. 185 min; p = 0.0001). The calculated median blood loss was of 50 ml (range, 0–500 ml), and no transfusions were required after surgery. Therefore, the results of the learning curve comparing the first 10 LLS procedures with the remaining procedures (living donation excepted) showed that the median operation time was statistically shorter for the last 26 LLS procedures (232 vs 163 min; p = 0.002). Similarly, there was a trend for decreased blood loss in this group (150 ml; range, 0–350 ml vs. 50 ml; range, 0–500 ml; p = 0.109), but it did not reach statistical significance (Fig. 4).
The operative time was shown to be slightly longer for malignancies (which became the first indication for laparoscopic LLS in the second part of our learning curve), and the blood loss was significantly less than with benign tumors (Table 4). The Pfannenstiel incision was used for 26 patients (70%). Neither conversion to laparotomy nor heterologous blood transfusion was recorded in this series. Postoperative morbidity consisted of one grade 1 complication (postoperative ileus) and two grade 2 complications (urinary tract infection and a germ-free hemorrhagic fluid collection drained percutaneously).
The median hospital stay was of 6 days (range, 2–10 days). However, this was longer for LLS procedures combined with bowel resection (median stay, 8 days; range, 7–10 days; p = 0.007) than for isolated LLS procedures (median stay, 5 days; range, 2–8 days).
The living liver donor successfully underwent the laparoscopic donation without any adverse event. At this writing, she is in excellent clinical condition.
Histology assessment
Final assessment showed that 2 of 13 liver cell adenomas were focal nodular hyperplasia. The overall mean number of lesions was 2 ± 1, and the mean lesion size was 55 ± 30 mm. However, benign resected nodules were statistically larger than malignant resected nodules (p = 0.01). The underlying liver parenchyma was found to be normal in 13 patients (35%), steatotic in 7 patients (19%; range, 5–60%), cirrhotic in 2 patients (5%), and characterized by some degree of fibrosis (F1–2) in 4 patients (10%) and by portal inflammation (A1-2) in another 11 patients (30%). No toxicity related to chemotherapy was described. These details are listed in Table 3.
Cancer patients
Neoadjuvant chemotherapy (Folfox or Folfiri plus bevacizumab) was administered to 8 (50%) of 16 patients with CRLM, leading to 50% average cell necrosis. Malignant lesions were resected with a minimal free margin of 5 mm (median, 5 mm; range 5–27 mm). After a median follow-up period of 21.5 months, two patients (12%) died of tumoral disease progression (at 23 and 38 months of follow-up evaluation, respectively), and seven patients (44%) experienced relapse of their cancer. For six patients (37%), CRLM led to a second hepatectomy, three of which involved an iterative laparoscopic resection.
The overall survival rates were 87% at both 1 and 3 years. The disease-free survival was 81% at 1 year and 41% at 3 years. The patient with a metastatic uveal melanoma experienced a relapse 3 months after LLS with disseminated intrahepatic disease and died within the following 9 months. The patient with a gastrointestinal stromal tumor (GIST) had a relapse under treatment with tyrosine-kinase inhibitors (Glivec) and underwent a second hepatectomy 30 months after the first resection. At this writing, no cancer at the level of the cutting edge, port sites, or surgical incision have been observed.
Discussion
Since the publication of the first nonanatomic liver resection and the first left lateral lobectomy, laparoscopic liver resection has been widely and increasingly performed for a variety of benign and malignant diseases [18, 19]. The development of this technique has been limited during this time due to difficulty reproducing basic open liver surgery maneuvers, risks of bleeding and pulmonary embolism, and fear of compromising oncologic resection by tumoral cell seeding [20, 21].
Laparoscopic LLS occupies a privileged position in laparoscopic liver surgery since it gained rapid popularity (as witnessed by several published series) for its well-defined anatomic surgical landmarks and relatively standardized technique. The overall results from five published case-control studies and six retrospective case series show that LLS is feasible and safe and that it is associated with low blood loss and has no liver-specific morbidity [2–4, 10, 12, 13].
Out of 36 patients, a clear learning curve was demonstrated in terms of operative time and use of the Pringle maneuver, with hospital stay reduced by the last 18 patients [10]. This also was observed in our series, confirming that this approach has an important teaching value, especially for beginners in laparoscopic resectional surgery. The Pringle maneuver actually is used in a minority of cases if not abandoned altogether, even for cirrhotic patients, as recently shown by other authors [22, 23]. Safe hemostasis can be achieved with different hemostatic devices (e.g., clips, argon beamer, or vascular stapler).
We share the opinion of others that a careful dissection of deep venous structures by the Harmonic scalpel or the Cavitron Ultrasonic Surgical Aspirator (CUSA) is preferable to avoid uncontrolled bleeding or pitfalls during liver dissection [16]. However, limitation of bleeding during dissection of cirrhotic patients probably could be better achieved by the use of vascular staplers [22, 24]. In our experience, there was a trend toward decreased bleeding within the learning curve. However, we recorded significantly more blood loss with benign lesions than with malignant tumors (Table 4, p = 0.01). This could be explained not only as a learning curve effect but also by the fact that severe steatosis was mostly predominant in benign solid tumors, which were the first indication for laparoscopic LLS during the period 2004 to 2006 (Fig. 1).
Some series have reported an increase in postoperative morbidity among patients with steatosis, particularly infective complications and postoperative gastrointestinal dysmotility [25, 26]. On the other hand, laparoscopic LLS in the second group of procedures was performed almost exclusively for patients with colorectal metastases and neoadjuvant bevacizumab-based chemotherapy. Findings have shown that this treatment can lead to an increase in chemotherapy-associated steatosis and steatohepatitis [27, 28]. Moreover, bevacizumab may enhance the risk of bleeding, imposing an interval after the last administration before liver resection is performed [29].
As our results show, we were not in a tight spot when performing laparoscopic LLS for CRLM, as witnessed by the significantly decreased operative time and the identical length of hospital stay (LOS) between the two groups, confirming the results of others [7]. In our experience, the length of hospital stay did not change during this time. However, for patients undergoing combined procedures (bowel–liver resection), a statistically significant LOS was recorded (as intuitively expected), related primarily to differences in intestinal transit time associated with the healing of reconstructive colon surgery. Indeed, overall complications were minimal, and no conversion to open procedure was needed [5, 7, 12, 13]. Actually, LOS was shorter than that recorded for open procedures and has decreased as much as 3 to 5 days in the more recent series compared with earlier experiences [12, 13].
Our acquired experience led us to propose laparoscopic LLS also for patients with a history of hepatic resection for CRLM. A total of 19 patients underwent laparoscopic LLS as a second hepatectomy for this indication of cancer relapse, whereas an iterative laparoscopic procedure was performed for the remaining 3 patients. Adequate intraoperative tumor assessment was provided by laparoscopy, resulting in free margins confirmed at the pathology report, without port-site metastases at follow-up evaluation. Indeed, 81% and 41% disease-free survivals at 1 and 3 years, respectively, after a median follow-up of 20 months with a 44% recurrence rate are in line with similar published experiences [6, 30].
The most recent data have shown that the oncologic outcomes for selected patients undergoing laparoscopic surgery are equivalent to those for open surgery [9, 12, 30, 31]. The use of biologic drugs (e.g., bevacizumab) did not further increase bleeding in either open or laparoscopic liver surgery [32, 33]. The favorable outcome we recorded for iterative laparoscopic resection in a very few cases could reflect some improvement in stress tolerance for repeated hepatectomy when the laparoscopic technique was used [31, 34]. The reduced overall morbidity observed with laparoscopic LLS is the main reason leading to the application of this technique for live liver donation at experienced hepatobiliary centers with the opportunity and knowledge to perform pediatric or adult liver transplantation [8, 11]. According to this published experience, the overall medical complication rate was higher for open than for laparoscopic procedures, with one retransplantation required in each of the recipient groups.
No morbidity was recorded for our first case in either the donor or the recipient. Although no stronger evidence exists that this technique is superior to the standardized live donor resection, data available from new experiences certainly are encouraging, leading us to continue further on this way [35]. Indeed, the difficulty obtaining randomized controlled trials to prove the superiority of minimally invasive techniques with respect to the standards is represented primarily by the small numbers of cases at each center and the limited expertise in laparoscopic hepatobiliary surgery for pediatric and adult liver transplantation groups. This is balanced by the possibility of overcoming the pediatric organ shortage by increasing splitting liver procedures [36].
Beyond the setting of laparoscopic live donation, the major obstacle to showing significant differences between open and laparoscopic liver resection procedures is the limited number of cases that can be randomized to an open versus a laparoscopic approach as well as the small number of experienced worldwide centers.
In conclusion, our experience reinforces the value of laparoscopic LLS for different indications and demonstrates that it can be performed safely with very low morbidity, minimal blood loss, and a short hospital stay for both normal and diseased liver parenchyma patients. For cancer patients, radical resection could be achieved with the potential to facilitate tolerance for a second hepatectomy to manage cancer relapses (e.g., colorectal metastases) during the follow-up period. The greatest advantage of this surgical technique is indeed its reproducibility and teaching value for hepatobiliary and laparoscopic surgeons willing to approach laparoscopic liver resection.
Laparoscopic LLS currently is considered primarily as a laparoscopic procedure for cancer surgery performed in very experienced centers for living donor hepatectomy [8, 17, 35]. We think our case clearly pictures not only the evolution of indications through our experience but also the safety of this option and the needed expertise when it is offered to healthy people such as living donors. In meanwhile, the future will teach us whether laparoscopic LLS will become a routine approach for living donor liver transplantation capable of reducing donor morbidity and enhancing the donor organ pool.
References
Cherqui D, Husson E, Hammoud R, Malassagne B, Stéphan F, Bensaid S, Rotman N, Fagniez PL (2000) Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 232:753–762
Gigot JF, Glineur D, Azagra JS, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L, Descottes B, Valleix D, Lachachi F, Bertrand C, Mansvelt B, Hubens G, Saey JP, Schockmel R (2002) Laparoscopic liver resection for malignant liver tumors. Ann Surg 236:90–97
Lesurtel M, Cherqui D, Laurent A, Tayar C, Fagniez PL (2003) Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg 196:236–242
Descottes B, Glineur D, Lachachi F, Valleix D, Paineau J, Hamy A, Morino M, Bismuth H, Castaing D, Savier E, Honore P, Detry O, Legrand M, Azagra JS, Goergen M, Ceuterick M, Marescaux J, Mutter D, de Hemptinne B, Troisi T, Weerts J, Dallemagne B, Jehaes C, Gelin M, Donckier V, Aerts R, Topal B, Bertrand C, Mansvelt B, Van Krunckelsven L, Herman D, Kint K, Totte E, Schockmel R, Gigot JF (2003) Laparoscopic liver resection of benign liver tumors. Surg Endosc 17:23–30
Morino M, Morra I, Rosso E, Miglietta C, Garrone C (2003) Laparoscopic vs open hepatic resection: a comparative study. Surg Endosc 17:1914–1918
Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Maeda T, Shiba T (2005) Laparoscopic resection of hepatocellular carcinoma. Am J Surg 189:190–194
Belli G, Fantini C, D’agostino A, Belli A, Cioffi L, Russolillo N (2006) Laparoscopic left lateral hepatic lobectomy: a safer and faster technique. J Hepatobiliary Pancreat Surg 13:149–154
Soubrane O, Cherqui D, Scatton O, Stenard F, Bernard D, Branchereau S, Martelli H, Gauthier F (2006) Laparoscopic left lateral sectionectomy in living donors: safety and reproducibility of the technique in a single center. Ann Surg 244:815–820
Vibert E, Perniceni T, Levard H, Denet C, Sharhri NK, Gayet B (2006) Laparoscopic liver resection. Br J Surg 93:67–72
Chang S, Laurent A, Tayar C, Karoui M, Cherqui D (2007) Laparoscopy as routine approach for left lateral sectionectomy. Br J Surg 94:58–63
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246:385–394
Aldrighetti L, Pulitano C, Catena M, Arru M, Guzzetti E, Casati M, Comotti L, Ferla G (2008) A prospective evaluation of laparoscopic versus open left lateral hepatic sectionectomy. J Gastrointest Surg 12:457–462
Abu Hilal M, Pierce NW (2008) Laparoscopic left lateral liver sectionectomy: a safe, efficient, reproducible technique. Dig Surg 25:305–308
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144:32–38
Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, Brock G, McMasters KM (2008) Experience with more than 500 minimally invasive hepatic procedures. Ann Surg 248:475–486
Bryant R, Laurent A, Tayar C, Cherqui D (2009) Laparoscopic liver resection: understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg 250:103–111
Troisi R, Debruyne R, Rogiers X (2009) Laparoscopic living donor hepatectomy for pediatric liver transplantation. Acta Chir Belg 109:559–562
Gagner M, Rheault M, Dubuc J (1992) Laparoscopic partial hepatectomy for liver tumor. Surg Endosc 6:97–98
Azagra JS, Goergen M, Gilbart E, Jacobs D (1996) Laparoscopic anatomical (hepatic) left lateral segmentectomy: technical aspects. Surg Endosc 10:758–761
McPhail MJ, Scibelli T, Abdelaziz M, Titi A, Pearce NW, Abu Hilal M (2009) Laparoscopic versus open left lateral hepatectomy. Expert Rev Gastroenterol Hepatol 4:345–351
Vigano L, Tayar C, Laurent A, Cherqui D (2009) Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg 16:410–421
Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, Russolillo N, Belli A (2007) Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc 21:2004–2011
Pulitanó C, Catena M, Arru M, Guzzetti E, Comotti L, Ferla G, Aldrighetti L (2008) Laparoscopic liver resection without portal clamping: a prospective evaluation. Surg Endosc 22:2196–2200
Gumbs AA, Gayet B, Gagner M (2008) Laparoscopic liver resection: when to use the laparoscopic stapler device. Hepato Pancreato Biliary 10:296–303
Selzner M, Clavien PA (2001) Fatty liver in liver transplantation and surgery. Semin Liver Dis 21:105–113
Kooby DA, Fong Y, Suriawinata A, Gonen M, Allen PJ, Klimstra DS, De Matteo RP, D’Angelica M, Blumgart LH, Jarnagin WR (2003) Impact of steatosis on perioperative outcome following hepatic resection. J Gastrointest Surg 7:1034–1044
Parikh AA, Gentner B, Wu TT, Curley SA, Ellis LM, Vauthey JN (2003) Perioperative complications in patients undergoing major liver resection with or without neoadjuvant chemotherapy. J Gastrointest Surg 7:1082–1088
Fernandez FG, Ritter J, Goodwin JW, Linehan DC, Hawkins WG, Strasberg SM (2005) Effect of steatohepatitis associated with irinotecan or oxaliplatin pretreatment on resectability of hepatic colorectal metastases. J Am Coll Surg 200:845–853
Roche: Bevacizumab (Avastin) Summary of product characteristics. Drugs RD. 2002;3(1):28–30. http://www.roche.com
O’Rourke N, Shaw I, Nathanson L, Martin I, Fielding G (2004) Laparoscopic resection of hepatic colorectal metastases. Hepato Pancreato Biliary 6:230–235
Castaing D, Vibert E, Ricca L, Azoulay D, Adam R, Gayet B (2009) Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg 250:849–856
Gruenberger B, Tamandl D, Schueller J, Scheithauer W, Zielinski C, Herbst F, Gruenberger T (2008) Bevacizumab, capecitabine, and oxaliplatin as neoadjuvant therapy for patients with potentially curable metastatic colorectal cancer. J Clin Oncol 26:1830–1835
Troisi R, Van den Bossche B, Laurent S, Deroo I, Berrevoet F, Libbrecht L, de Hemptinne B (2009) Addition of bevacizumab to neoadjuvant therapy may increase resectability rate without significant morbidity in patients with initially non-resectable colorectal liver metastases. Hepato Pancreato Biliary 11(Suppl 2):1–2
Novitsky YW, Litwin DE, Callery MP (2004) The net immunologic advantage of laparoscopic surgery. Surg Endosc 18:1411–1419
Koffron A, Kung RD, Auffenberg GB, Abecassis M (2007) Laparoscopic liver surgery for everyone: the hybrid method. Surgery 142:463–468
Cardillo M, De Fazio N, Pedotti P, De Feo T, Fassati LR, Mazzaferro V, Colledan M, Gridelli B, Caccamo L, DeCarlis L, Valente U, Andorno E, Cossolini M, Martini C, Antonucci A, Cillo U, Zanus G, Baccarani U, Scalamogna M, NITp Liver Transplantation Working Group (2006) Split and whole liver transplantation outcomes: a comparative cohort study. Liver Transplant 12:402–410
Disclosures
Roberto Ivan Troisi, Jacques Van Huysse, Frederik Berrevoet, Bert Vandenbossche, Mauricio Sainz-Barriga, Alessio Vinci, Salvatore Ricciardi, Tommaso Bocchetti, Xavier Rogiers, and Bernard de Hemptinne have no conflicts of interest or financial ties to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Troisi, R.I., Van Huysse, J., Berrevoet, F. et al. Evolution of laparoscopic left lateral sectionectomy without the Pringle maneuver: through resection of benign and malignant tumors to living liver donation. Surg Endosc 25, 79–87 (2011). https://doi.org/10.1007/s00464-010-1133-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1133-8