Abstract
Many modern “paediatric” mechanical ventilators have in-built features for estimation of respiratory mechanics which could be useful in the management of ventilated infants and children. The aim of this study was to determine if such measurements were reproducible and accurate. Ventilator (Draeger Evita 4) displayed compliance (Cvent) and resistance (Rvent) values were assessed and compared to the results of respiratory system mechanics (respiratory system compliance (Crs) and resistance (Rrs)) measurements obtained using a single breath occlusion technique. Seventeen children (median age 5.1; range 0.3 to 16 yrs) were studied on 24 occasions. The mean coefficients of variations for the techniques were similar (Cvent 13%; Crs 11%; Rvent 16%; Rrs 14%). The mean (SD) Crs (22.8 (12.3) ml/cmH2O) did not differ significantly from Cvent (22.1 (12.7) ml/cm H2O) but the mean Rrs 21.0 (12.7) cmH2O/l/s was significantly higher than the mean Rvent 32.0 (32.0) cmH2O/l/s (p = 0.03). Bland and Altman analysis demonstrated a mean difference of −10.94 cmH2O/l/s (SD 24.1) between Rrs and Rvent; the agreement between Rrs and Rvent decreased as Rrs increased (p = 0.008). Conclusions: Ventilator assessment of compliance, but not resistance, using the Evita 4 is reproducible and reliable.
Similar content being viewed by others
Introduction
The respiratory system status of ventilated paediatric patients is usually monitored by clinical assessment and blood gas measurements. Measurement of respiratory mechanics in ventilated children, however, could provide useful information about the physiological status of the respiratory system, the course of disease and response to treatment interventions [15]. Specialised equipment and expertise have been required to make such measurements, which may explain why a survey of paediatric intensive care units in the UK [11] revealed that only two of the 22 responding units used lung function measurements. Modern mechanical ventilators now available, however, have in-built features for estimation of respiratory mechanics, which may mean more widespread use of lung function measurements in the PICU. As a consequence, it is important (and the aim of this study) to determine if such measurements are reproducible and if they are accurate by assessing their relationship to the results of standard techniques of assessing respiratory mechanics.
Materials and methods
Children who were mechanically ventilated for more than 24 hours were eligible for entry into this study. The study was approved by the Research Ethics Committee of King’s College Hospital NHS Trust and parents gave informed written consent for their children to take part.
Measurements were performed in the recovery stage of the subjects’ illnesses with the subjects mechanically ventilated at the settings determined by the medical team. All the children were receiving sedation, but not muscle relaxants and all were making spontaneous respiratory efforts. Measurements were performed with the patient supine and haemodynamically stable with stable blood gases. Endotracheal tubes were suctioned 15 to 20 minutes prior to performing the study.
All the children were supported by the Draeger Evita 4 ventilator in a pressure control mode. The ventilator estimated compliance (Cvent) by dividing the tidal volume by the difference between the PIP and PEEP (ΔP) and resistance (Rvent) by dividing the pressure difference (ΔP) by the expiratory flow. Flow and tidal volume were measured by the ventilator at the expiratory valve and breath-by-breath measurements of compliance and resistance displayed. Ten consecutive breath-to-breath estimates of Cvent and Rvent displayed by the ventilator were recorded and the mean was calculated.
Respiratory system compliance (Crs) and resistance (Rrs) were then measured using the single breath occlusion technique. Flow was measured using a pneumotachograph (4500 series, Hans Rudolf Inc, Kansas, USA) and differential pressure transducer (MP45, Validyne Corporation, Northridge, CA, USA). The pneumotachograph was attached to a manually operated, three-way sliding valve (2820 Series, Hans Rudolf Inc, Kansas, USA) and inserted between the ETT and the ventilator circuit. Airway pressure was measured from a side port on the pneumotachograph using a differential pressure transducer (MP 45, Validyne Corporation, Northridge, CA, USA). The signals from both transducers were amplified (CD280 carrier amplifier, Validyne Corporation, Northridge, CA, USA) and displayed in real time on a computer running Labview software (version 5.1, National Instruments, Austin, TX, USA) with 100 Hz analog to digital sampling (DAQ 16XE-50, National Instruments, Austin, TX, USA). Tidal volume was obtained by digital integration of the respiratory flow signal by the software. The three-way valve was actuated at end inspiration, briefly occluding the airway, evoking the Hering Breuer inflation reflex, and subsequently diverting the resulting passive exhalation to atmosphere. The resulting relaxed expiratory flow volume curve and the pressure time trace were analysed to calculate the expiratory time constant (Trs), Crs and Rrs. Crs was calculated by dividing the change in airway pressure by expired volume. Trs was measured as the slope of a best fit line fitted to the expiratory flow volume curve and Rrs by dividing Crs by Trs. Occlusions were maintained for at least 400 ms. Only those with a pressure plateau of at least 100 ms were used. The flow volume curve was analysed using the software and only those with a linearity of >0.99 for at least 40% of the curve were used. Eight to ten occlusions were recorded and the mean value calculated. At least 10 breaths were allowed between occlusions. The resistances of the pneumotachograph and slide valve were subtracted from the total measured resistance to obtain Rrs.
Statistical analysis
Data were tested (Shapiro-Wilk) and shown to be normally distributed; hence, differences were assessed for statistical significance using a paired t-test. The level of agreement between the techniques was assessed using Bland and Altman analysis [3] and Spearman rank analysis was used to further assess this relationship.
Results
Seventeen infants and children (mean (SD) age 6.3 (6.0) years (Table 1)) measured on 24 separate occasions are reported. Their mean (SD) duration of ventilator days was 4.3 (1.8). Fifteen patients were intubated using cuffed ETT and had no leak, i.e. no difference between inspiratory and expiratory tidal volumes measured from the pneumotachograph. The other two children had less than 5% difference between inspiratory and expiratory tidal volumes as measured from the pneumotachograph.
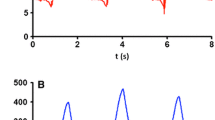
The mean intra-subject coefficients of variation were similar for both techniques for compliance (Cvent 13% and CRS 11%) and resistance (Rvent 16% and Rrs 14%). There was no statistically significant difference between the mean (SD) Cvent 22.1 (12.7) ml/cmH2O and Crs 22.8 (12.3) ml/cmH2O (p = 0.4), but there was a statistically significant difference between the mean Rvent 32.0 (32.0) cmH2O/l/s and Rrs 21.0 ((SD) 12.7) cmH2O/l/s (p = 0.03) (Table 2). There was a mean difference of 0.7 ml/cmH2O (SD 4.2) between the Crs and Cvent (Fig. 1) and −10.94 cmH2O/l/s (SD 24.1) between the Rrs and Rvent results. The agreement between Rrs and Rvent tended to decrease as Rrs increased (Fig. 1) with a significant association between the mean of Rvent and Rrs and mean difference between Rvent and Rrs (r=−0.53, p = 0.008).
Discussion
We have demonstrated that the compliance and resistance results estimated by the ventilator were reproducible, but only the compliance results were similar to those determined by single breath mechanics. We used the single breath occlusion technique, as this can be easily applied in ventilated infants and does not require passage of balloon catheters. The key to obtaining accurate measurements using this technique is achieving relaxed expiration. In the current study, all the children were receiving sedation. Careful examination of the resulting flow volume loop using the criteria defined above was performed to ensure relaxed expirations had been obtained following airway occlusions. Other techniques have been employed to evaluate the respiratory mechanics of ventilated infants and children, including passive expiration to PEEP [17] and the modified Mead-Whittenbereger technique [13]. We have previously shown [12] that measures of compliance and resistance were similar for all techniques.
The patients studied had a variety of diagnoses. Thirty percent had a primary lung disease but others had lung involvement due to generalised sepsis, chest wall oedema, ascites or increased post operative intra abdominal pressure affecting their respiratory status. Thus we were able to study children with a range of lung function abnormalities and hence our results are generalisable.
Respiratory diseases were the primary or admitting diagnosis in only 30% of subjects, but respiratory system involvement was present in the majority of our patients. Most children were studied in the recovery stage of their illness, that is, shortly before extubation and as a consequence few had very abnormal Crs and Rrs results (Table 2). It is important to note, however, that the children had a range of Crs and Rrs results and we were able to demonstrate that the difference between Rrs and Rvent increased as resistance increased, indicating that in patients in the acute phase with greater degrees of underlying lung disease a greater discrepancy between measurements would exist.
The patients studied in the current study had little or no leak around the endotracheal tube. Endotracheal tube leak, however, can occur in ventilated neonates and children, especially when straight, uncuffed ETTs are used [2, 10]. The influence of the ETT leak on Crs and Rrs has been investigated [8–10, 16], demonstrating the presence of a leak around the endotracheal tube leads to volume loss and higher airflow which in turn affect the accuracy of measurements of compliance and resistance, respectively. The ventilatory mode compounds the errors produced by endotracheal tube leak [8–10, 16]. Under such circumstances the accuracy, and hence reliability, of ventilator derived measurements would be further affected.
Care was taken to avoid changing the physiological status of the patients during the study. The three-way sliding valve and pneumotachograph were inserted into the ventilator circuit quickly and with minimal disruption to the patient’s ventilatory support. Similarly, end inspiratory airway occlusions were brief, approximately 400 ms, and the valve returned to its standby position immediately at the end of expiration. No changes in blood pressure, respiratory rate or blood gas levels were observed during equipment insertion or airway occlusion. In addition, the close agreement between Crs and Cvent suggest Crs measurement had minimal influence on patient status.
Single breath occlusion involves passive measurements, whereas the ventilator makes dynamic measurements, thus we did not expect to see the same results, but, if the ventilator assessments were reliable then the results should have been similar to those of single breath mechanics. Although CRS and Cvent results were similar, there was a highly significant difference between the Rvent and RRS results and most importantly the differences increased at higher resistance values, reflecting inaccuracy of the ventilator measurements.
We only assessed one ventilator type, but previous studies have demonstrated the inaccuracy of ventilator derived measurements, particularly with the Servo 300, which also measures tidal volume at the expiratory valve [4, 5, 14]. Castle et al. [5] demonstrated that the expired tidal volume displayed by Servo 300, after correcting for gas compression, underestimated the true expired volume by up to 64% in the smallest infants but overestimated by as much as 29% in older children. We now demonstrate that using the Evita 4 estimates of respiratory resistance is inaccurate.
Randomized controlled studies are required to evaluate whether routine assessment of these measurements of respiratory function improve the quality of treatment and outcome in children receiving mechanical ventilation. The value of such measurements in predicting the outcome of weaning and extubation has been limited [1, 6, 7], but respiratory system compliance and resistance provide information about underlying lung pathology and the load that is imposed on the respiratory muscles. If there are improvements in the accuracy and range of measurements available including common weaning indices and measures of respiratory muscle function, then ventilator derived measurements may become of increasing usefulness.
We conclude compliance estimated by the Draeger Evita 4 mechanical ventilator is reproducible and reliable, and thus could provide a useful alternative to standard measurements in ventilated children. Our results, however, emphasize resistance estimates using this ventilator should be interpreted with caution. Many modern mechanical ventilators provide measures of respiratory mechanics; we would recommend, however, exercising caution before using such information in research and particularly if used in clinical decision making and patient management. Ventilator derived measurements should be compared to those of a standard technique before utilizing such results for research or clinical applications.
Abbreviations
- Crs:
-
respiratory system compliance
- Cvent:
-
ventilator estimated compliance
- PIP:
-
peak inflating pressure
- PEEP:
-
positive end expiratory pressure
- Rvent:
-
ventilator estimated resistance
- Rrs:
-
respiratory system resistance
- Trs:
-
expiratory time constant
References
Baumeister BL, el-Khatib M, Smith PG, Blumer JL (1997) Evaluation of predictors of weaning from mechanical ventilation in pediatric patients. Pediatr Pulmonol 24:344–352
Bernstein G, Knodel E, Heldt GP (1995) Airway leak size in neonates and autocycling of three flow-triggered ventilators. Crit Care Med 23:1739–1744
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Cannon ML, Cornell J, Tripp-Hamel DS, Gentile MA, Hubble CL, Meliones JN, Cheifetz IM (2000) Tidal volumes for ventilated infants should be determined with a pneumotachometer placed at the endotracheal tube. Am J Respir Crit Care Med 162:2109–2112
Castle RA, Dunne CJ, Mok Q, Wade AM, Stocks J (2002) Accuracy of displayed values of tidal volume in the pediatric intensive care unit. Crit Care Med 30:2566–2574
Jubran A, Tobin MJ (1997) Passive mechanics of lung and chest wall in patients who failed or succeeded in trials of weaning. Am J Respir Crit Care Med 155:916–921
Khan N, Brown A, Venkataraman ST (1996) Predictors of extubation success and failure in mechanically ventilated infants and children. Crit Care Med 24:1568–1579
Kondo T, Matsumoto I, Lanteri CJ, Sly PD (1997) Respiratory mechanics during mechanical ventilation: a model study on the effects of leak around a tracheal tube. Pediatr Pulmonol 24:423–428
Kuo CY, Gerhardt T, Bolivar J, Claure N, Bancalari E (1996) Effect of leak around the endotracheal tube on measurements of pulmonary compliance and resistance during mechanical ventilation: a lung model study. Pediatr Pulmonol 22:35–43
Main E, Castle R, Stocks J, James I, Hatch D (2001) The influence of endotracheal tube leak on the assessment of respiratory function in ventilated children. Intensive Care Med 27:1788–1797
Manczur TI, Greenough A, Rafferty GF (2000) Survey of current practices of weaning from mechanical ventilation in paediatric intensive care. Brit J Intens Care 10:114–120
Manczur TI, Greenough A, Rafferty GF, Milner AD (2000) Measurement of pulmonary mechanics in the paediatric intensive care unit: a comparison of techniques during pressure- and volume-limited ventilation. Pediatr Pulmonol 30:265–268
Naik S, Greenough A, Giffin FJ, Baker A (1996) The effect of changes in PEEP pressure on gas exchange-influence of baseline lung function abnormalities. Brit J Intens Care 62:82–88
Neve V, Leclerc F, Noizet O, Vernoux S, Leteurtre S, Forget P, Sadik A, Riou Y (2003) Influence of respiratory system impedance on volume and pressure delivered at the Y piece in ventilated infants. Pediatr Crit Care Med 4:418–425
Newth CJ, Stretton M, Deakers TW, Hammer J (1997) Assessment of pulmonary function in the early phase of ARDS in pediatric patients. Pediatr Pulmonol 23:169–175
Nikischin W, Lange M (2003) Correction of compliance and resistance altered by endotracheal tube leaks. Pediatr Crit Care Med 4:344–352
Storme L, Riou Y, Logier R, Dubos JP, Kacet N, Rousseau S, Lequien P (1994) A new application of an old method for respiratory mechanics measurements: the passive inflation method in newborn infants during pressure-controlled ventilation. Pediatr Pulmonol 18:244–254
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding note: Dr Harikumar was supported by the Wellcome Trust.
Rights and permissions
About this article
Cite this article
Harikumar, G., Greenough, A. & Rafferty, G.F. Ventilator assessment of respiratory mechanics in paediatric intensive care. Eur J Pediatr 167, 287–291 (2008). https://doi.org/10.1007/s00431-007-0477-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-007-0477-0