Abstract
Purpose
8% of the US population has asthma. Air pollution is linked to exacerbation in susceptible individuals. The objective was to identify air pollutants that increased the risk of asthma emergency department visits during a time wherein a polluting factory was criminally convicted, changing local air pollutant levels.
Methods
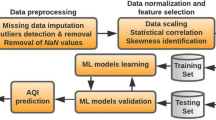
An ecological time-series design used a daily count of asthma emergency visits from 2007 to 2012 as the dependent variable. Independent variables air pollutants (NO2, PM2.5 CO, and O3), controlling for meteorological conditions, were analyzed using time-series and Poisson GLM models.
Results
76,651 emergency asthma visits were included with an average of 35 visits per day (SD = 9.2, range 11–80) in a stationary time series. Increased visit volume in fall and spring had no associations to the air pollutants. Associations between individual air pollutants occurred in otherwise low-volume months for asthma emergency visits. The strongest relationship was an 11.6% increase in the asthma emergency visit rate during the month of June. In monthly groupings that removed most of the autumn and spring months, O3, PM2.5, CO, and NO2 were associated with 5, 4, 2, and 2% increases in asthma emergency visits, respectively. CO was the only pollutant with a negative association with asthma emergency visits, occurring in the month of April.
Conclusions
Pollutants NO2, PM2.5 CO, and O3 were associated with increased emergency asthma visits in some, but not all months of the year. Air pollution’s impact on asthma emergencies may be masked by other, more influential seasonal triggers, such as infections or allergies.

Similar content being viewed by others
References
42 USC (1977) 7401-7671 Clean Air Act
Alhanti BA, Chang HH, Winquist A, Mulholland JA, Darrow LA, Sarnat SE (2016) Ambient air pollution and emergency department visits for asthma: a multi-city assessment of effect modification by age. J Expo Sci Environ Epidemiol 26(2):180–188. doi:10.1038/jes.2015.57
Anderson HR, Favarato G, Atkinson RW (2013) Long-term exposure to air pollution and the incidence of asthma: meta-analysis of cohort studies. Air Qual Atmos Health 6(1):47–56
Choi M, Curriero FC, Johantgen M, Mills ME, Sattler B, Lipscomb J (2011) Association between ozone and emergency department visits: an ecological study. Int J Environ Health Res 21(3):201–221
Cirera L et al (2012) Daily effects of air pollutants and pollen types on asthma and COPD hospital emergency visits in the industrial and Mediterranean Spanish city of Cartagena. Allergol Immunopathol 40(4):231–237
Civic Impulse (2017) S. 1630—101st Congress: Clean Air Act Amendments of 1990
Cook AG, deVos AJ, Pereira G, Jardine A, Weinstein P (2011) Use of a total traffic count metric to investigate the impact of roadways on asthma severity: a case-control study. Environ Health A Global Access Sci Source 10:52
Cromar KR, Gladson LA, Perlmutt LD, Ghazipura M, Ewart GW (2016) American Thoracic Society and Marron Institute Report. Estimated excess morbidity and mortality caused by air pollution above American thoracic society-recommended standards, 2011–2013. Ann Am Thorac Soc 13(8):1195–1201. doi:10.1513/AnnalsATS.201602-103AR
D’Amato G et al (2016) Climate change and air pollution: effects on respiratory allergy. Allergy Asthma Immunol Res 8(5):391–395. doi:10.4168/aair.2016.8.5.391
Darrow LA et al (2011) The use of alternative pollutant metrics in time-series studies of ambient air pollution and respiratory emergency department visits. J Expo Sci Environ Epidemiol 21(1):10–19. doi:10.1038/jes.2009.49
Darrow LA, Klein M, Flanders WD, Mulholland JA, Tolbert PE, Strickland MJ (2014) Air pollution and acute respiratory infections among children 0–4 years of age: an 18-year time-series study. Am J Epidemiol 180(10):968–977. doi:10.1093/aje/kwu234
Delfino RJ, Wu J, Tjoa T, Gullesserian SK, Nickerson B, Gillen DL (2014) Asthma morbidity and ambient air pollution: effect modification by residential traffic-related air pollution. Epidemiology 25(1):48–57. doi:10.1097/ede.0000000000000016
Di Q et al (2017) Air pollution and mortality in the medicare population. N Engl J Med 376(26):2513–2522. doi:10.1056/NEJMoa1702747
United States Environmental Protection Agency (2017). https://aqs.epa.gov/aqsweb/documents/data_mart_welcome.html. Accessed 05 May 2017
Galan I, Tobias A, Banegas JR, Aranguez E (2003) Short-term effects of air pollution on daily asthma emergency room admissions. Eur Respir J 22(5):802–808
Gass K et al (2015) Associations between ambient air pollutant mixtures and pediatric asthma emergency department visits in three cities: a classification and regression tree approach. Environ Health 14:58. doi:10.1186/s12940-015-0044-5
Gauderman WJ et al (2015) Association of improved air quality with lung development in children. N Engl J Med 372(10):905–913. doi:10.1056/NEJMoa1414123
Guarnieri M, Balmes JR (2014) Outdoor air pollution and asthma. Lancet 383(9928):1581–1592. doi:10.1016/s0140-6736(14)60617-6
Halonen JI, Lanki T, Tiittanen P, Niemi JV, Loh M, Pekkanen J (2010) Ozone and cause-specific cardiorespiratory morbidity and mortality. J Epidemiol Community Health 64(9):814–820. doi:10.1136/jech.2009.087106
Johnston NW, Sears MR (2006) Asthma exacerbations. 1: Epidemiology. Thorax 61(8):722–728. doi:10.1136/thx.2005.045161
Johnston NW, Johnston SL, Norman GR, Dai J, Sears MR (2006) The September epidemic of asthma hospitalization: school children as disease vectors. J Allergy Clin Immunol 117(3):557–562. doi:10.1016/j.jaci.2005.11.034
Kloog I, Nordio F, Zanobetti A, Coull BA, Koutrakis P, Schwartz JD (2014) Short term effects of particle exposure on hospital admissions in the Mid-Atlantic states: a population estimate. PLoS One 9(2):e88578. doi:10.1371/journal.pone.0088578
Kousha T, Castner J (2016) the air quality health index and emergency department visits for otitis media. J Nurs Scholarsh 48(2):163–171. doi:10.1111/jnu.12195
Kousha T, Rowe BH (2014) Ambient ozone and emergency department visits due to lower respiratory condition. Int J Occup Med Environ Health 27(1):50–59. doi:10.2478/s13382-014-0229-0
Lavigne E, Villeneuve PJ, Cakmak S (2012) Air pollution and emergency department visits for asthma in Windsor, Canada. Can J Public Health 103(1):4–8
Lim SS et al (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2224–2260. doi:10.1016/s0140-6736(12)61766-8
Linaker CH et al (2000) Personal exposure to nitrogen dioxide and risk of airflow obstruction in asthmatic children with upper respiratory infection. Thorax 55(11):930–933
Malig BJ et al (2016) A time-stratified case-crossover study of ambient ozone exposure and emergency department visits for specific respiratory diagnoses in California (2005–2008). Environ Health Perspect 124(6):745–753. doi:10.1289/ehp.1409495
Masjedi MR et al (2003) The effects of air pollution on acute respiratory conditions. Respirology 8(2):213–230
Masoli M, Fabian D, Holt S, Beasley R (2004) The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 59(5):469–478. doi:10.1111/j.1398-9995.2004.00526.x
Moineddin R, Nie JX, Domb G, Leong AM, Upshur RE (2008) Seasonality of primary care utilization for respiratory diseases in Ontario: a time-series analysis. BMC Health Serv Res 8:160. doi:10.1186/1472-6963-8-160
New York State Department of Environmental Conservation (2009) Tonawanda community air quality study—June 2009. https://www.dec.ny.gov/chemical/59464.html. Accessed 5 May 2015
New York State Department of Health (2015) Statewide Planning and Research Cooperative System (SPARCS)
New York State Department of Environmental Conservation (2016) Tonawanda community air quality study—update, December 2016. https://www.dec.ny.gov/chemical/59464.html. Accessed 13 Oct 2017
Paulu C, Smith AE (2008) Tracking associations between ambient ozone and asthma-related emergency department visits using case-crossover analysis. J Public Health Manag Pract 14(6):581–591. doi:10.1097/01.PHH.0000338371.53242.0e
Peel JL et al (2005) Ambient air pollution and respiratory emergency department visits. Epidemiology 16(2):164–174
Sacks JD, Rappold AG, Davis JA Jr, Richardson DB, Waller AE, Luben TJ (2014) Influence of urbanicity and county characteristics on the association between ozone and asthma emergency department visits in North Carolina. Environ Health Perspect 122(5):506–512. doi:10.1289/ehp.1306940
Stafoggia M et al (2013) Short-term associations between fine and coarse particulate matter and hospitalizations in Southern Europe: results from the MED-PARTICLES project. Environ Health Perspect 121(9):1026–1033. doi:10.1289/ehp.1206151
Stieb DM, Szyszkowicz M, Rowe BH, Leech JA (2009) Air pollution and emergency department visits for cardiac and respiratory conditions: a multi-city time-series analysis. Environ Health 8:25. doi:10.1186/1476-069x-8-25
Strickland MJ et al (2010) Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med 182(3):307–316. doi:10.1164/rccm.200908-1201OC
Strickland MJ et al (2011) Implications of different approaches for characterizing ambient air pollutant concentrations within the urban airshed for time-series studies and health benefits analyses. Environ Health 10:36. doi:10.1186/1476-069x-10-36
Strickland MJ, Hao H, Hu X, Chang HH, Darrow LA, Liu Y (2016) Pediatric emergency visits and short-term changes in PM2.5 concentrations in the U.S. State of Georgia. Environ Health Perspect 124(5):690–696. doi:10.1289/ehp.1509856
Szyszkowicz M, Kousha T (2014) Emergency department visits for asthma in relation to the Air Quality Health Index: a case-crossover study in Windsor, Canada. Can J Public Health 105(5):e336–e341
Tetreault LF et al (2016) Severe and moderate asthma exacerbations in asthmatic children and exposure to ambient air pollutants. Int J Environ Res Public Health. doi:10.3390/ijerph13080771
Tolbert PE et al (2000) Air quality and pediatric emergency room visits for asthma in Atlanta, Georgia, USA. Am J Epidemiol 151(8):798–810
Toxic Release Inventory Explorer (2015) https://iaspub.epa.gov/triexplorer/tri_release.chemical. Accessed 5 May 2015
United States v Tonawanda Coke Corporation (2013) W.D.N.Y 10-CR-219S
Woodruff TJ et al (2009) Methodological issues in studies of air pollution and reproductive health. Environ Res 109(3):311–320. doi:10.1016/j.envres.2008.12.012
Wright RJ et al (2008) Transdisciplinary research strategies for understanding socially patterned disease: the Asthma Coalition on Community, Environment, and Social Stress (ACCESS) project as a case study. Cien Saude Colet 13(6):1729–1742
Zahran H, Bailey C, Garbe P (2011) Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001–2009. MMWR Morb Mortal Wkly Rep 60(17):547–552
Acknowledgements
This study was funded by the University at Buffalo’s Civic Engagement and Public Policy Dissemination Fellowship grant and the Patricia H. Garman Behavioral Health Nursing Endowment at the University at Buffalo School of Nursing. This study was performed in partial fulfillment of Dr. Caster’s role as lead investigator, with anticipated support from, the Environmental Health Study of Western New York (also documented as The Tonawanda Health Study: An Epidemiologic Study of Health Effects and Coke Oven Emissions from Tonawanda Coke). The authors gratefully acknowledge our community partners, IT support, and Drs. Tarunraj Singh and Robert Baier, as well as students and research assistants Souransu Nandi, Ziqiang Chen, Wolf Wackeroth, Nan Nan, Harish Mangalampalli and Angad Gadre.
Author information
Authors and Affiliations
Contributions
JC and YY contributed to the concept, design and analysis of the data. LG contributed to the analysis and interpretation of the data. JC drafted the paper and all authors contributed to the revision and final approval.
Corresponding author
Ethics declarations
Ethical approval
Relevant ethical approval was obtained from the New York State Data Protection Review Board (#1403-05) and the University at Buffalo’s Institutional Review Board.
Conflict of interest
Dr. Yin and Mr. Guo declare no conflict of interest. Dr. Castner’s research has been funded by grants from The Rockefeller University Heilbrunn Family Center for Nursing Research, NSF (#1737617, #1645090), The Ohio State University, University at Buffalo, and had been committed support by the University at Buffalo through NIH (#1U54TR001358). Dr. Castner has received support from the Emergency Nursing Association/Journal of Emergency Nursing for teaching, speaking honoraria, and editor/editorial board travel. Dr. Castner has had a research/data analysis consulting relationship with the Harvard T. H. Chan School of Public Health, American Lung Association, and hospitals in the region of study, with additional funding/consulting disclosures which are unlikely to be perceived as a conflict of interest available on request.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Castner, J., Guo, L. & Yin, Y. Ambient air pollution and emergency department visits for asthma in Erie County, New York 2007–2012. Int Arch Occup Environ Health 91, 205–214 (2018). https://doi.org/10.1007/s00420-017-1270-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-017-1270-7