Abstract
Background
Reduced sleep quality is associated with impaired quality of life and increased mortality in patients with heart failure. The aim of this study was to observe changes in sleep fragmentation and sleep quality in patients with heart disease and preserved left ventricular ejection fraction (pEF) treated with adaptive servo-ventilation (ASV) therapy for treatment of emergent central sleep apnea (TECSA) or central sleep apnea (CSA).
Methods
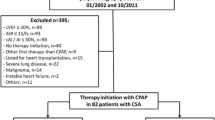
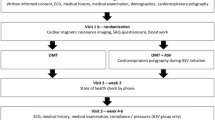
114 patients with structural heart disease and pEF introduced to ASV therapy between 2010 and 2015 were retrospectively analyzed. Patients were stratified into two groups; TECSA (n = 60) or CSA (n = 54). Changes of sleep fragmentation and sleep quality from baseline to ASV initiation were compared.
Results
ASV therapy leads to a significant reduction of apnea–hypopnea index (AHI) and arousal index in patients with TECSA and CSA (∆AHI: − 43 ± 21 vs. − 47 ± 22/h; ∆arousal index − 11 ± 15, vs. − 11 ± 21/h). ASV treatment leads to a significant increase in sleep efficiency in TECSA compared to CSA (∆SE: 10 ± 19 vs. 1 ± 18%, p = 0.019). Both groups had significantly longer stage N3 (N3) and rapid eye movement sleep (REM) on ASV (∆N3: 8 ± 11 vs. 9 ± 13%; ∆REM 7 ± 9 vs. 3 ± 8%; p < 0.05 for all comparisons baseline vs. ASV).
Conclusions
In patients with heart disease and pEF, whose TECSA and CSA were treated with ASV, a significant reduction of AHI and arousal index as well as an increase of N3 and REM sleep was observed. Increase of sleep efficiency was significantly greater in TECSA compared to CSA. Hence, improvements of sleep quality were modestly greater in patients with TECSA compared to those with CSA.



Similar content being viewed by others
References
Arzt M, Woehrle H, Oldenburg O et al (2016) Prevalence and predictors of sleep-disordered breathing in patients with stable chronic heart failure: the SchlaHF registry. JACC Heart Fail 4(2):116–125. https://doi.org/10.1016/j.jchf.2015.09.014
Geib T, Plappert N, Roth T et al (2015) Prevalence of sleep-disordered breathing-related symptoms in patients with chronic heart failure and reduced ejection fraction. Can J Cardiol 31(7):839–845. https://doi.org/10.1016/j.cjca.2015.02.025
Oldenburg O, Lamp B, Faber L et al (2007) Sleep-disordered breathing in patients with symptomatic heart failure A contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 9(3):251–257. https://doi.org/10.1016/j.ejheart.2006.08.003
Mentz RJ, Fiuzat M (2014) Sleep disordered breathing in patients with heart failure. Heart Failure Clin 10(2):243–250. https://doi.org/10.1016/j.hfc.2013.10.001
Linz D, Woehrle H, Bitter T et al (2015) The importance of sleep-disordered breathing in cardiovascular disease. Clin Res Cardiol 104(9):705–718. https://doi.org/10.1007/s00392-015-0859-7
Reinhard W, Plappert N, Zeman F et al (2013) Prognostic impact of sleep duration and sleep efficiency on mortality in patients with chronic heart failure. Sleep Med 14(6):502–509. https://doi.org/10.1016/j.sleep.2012.12.014
Oldenburg O, Spiesshofer J, Fox H et al (2015) Cheyne-Stokes respiration in heart failure: friend or foe? Hemodynamic effects of hyperventilation in heart failure patients and healthy volunteers. Clin Res Cardiol 104(4):328–333. https://doi.org/10.1007/s00392-014-0784-1
Teschler H, Dohring J, Wang YM et al (2001) Adaptive pressure support servo-ventilation: a novel treatment for Cheyne–Stokes respiration in heart failure. Am J Respir Crit Care Med 164(4):614–619. https://doi.org/10.1164/ajrccm.164.4.9908114
Loredo JS, Ancoli-Israel S, Kim EJ et al (2006) Effect of continuous positive airway pressure versus supplemental oxygen on sleep quality in obstructive sleep apnea: a placebo-CPAP-controlled study. Sleep 29(4):564–571
Sharma BK, Bakker JP, McSharry DG et al (2012) Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: a systematic review and meta-analysis. Chest 142(5):1211–1221. https://doi.org/10.1378/chest.12-0815
Correia S, Martins V, Sousa L et al (2015) Clinical impact of adaptive servoventilation compared to other ventilatory modes in patients with treatment-emergent sleep apnea, central sleep apnea and Cheyne–Stokes respiration. Rev Port Pneumol (2006) 21(3):132–137. https://doi.org/10.1016/j.rppnen.2014.08.005
Mayer G, Arzt M, Braumann B et al (2017) German S3 guideline nonrestorative sleep/sleep disorders, chapter “sleep-related breathing disorders in adults.” Short Version Somnologie. https://doi.org/10.1007/s11818-017-0136-2
Aurora RN, Chowdhuri S, Ramar K et al (2012) The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses. Sleep 35(1):17–40. https://doi.org/10.5665/sleep.1580
Bitter T, Westerheide N, Hossain MS et al (2011) Complex sleep apnoea in congestive heart failure. Thorax 66(5):402–407. https://doi.org/10.1136/thx.2010.146522
Westhoff M, Arzt M, Litterst P (2012) Prevalence and treatment of central sleep apnoea emerging after initiation of continuous positive airway pressure in patients with obstructive sleep apnoea without evidence of heart failure. Sleep Breath 16(1):71–78. https://doi.org/10.1007/s11325-011-0486-0
Nigam G, Pathak C, Riaz M (2016) A systematic review on prevalence and risk factors associated with treatment- emergent central sleep apnea. Ann Thorac Med 11(3):202–210. https://doi.org/10.4103/1817-1737.185761
Hetzenecker A, Escourrou P, Kuna ST et al (2016) Treatment of sleep apnea in chronic heart failure patients with auto-servo ventilation improves sleep fragmentation: a randomized controlled trial. Sleep Med 17:25–31. https://doi.org/10.1016/j.sleep.2015.08.020
Hetzenecker A, Roth T, Birner C et al (2016) Adaptive servo-ventilation therapy of central sleep apnoea and its effect on sleep quality. Clin Res Cardiol 105(3):189–195. https://doi.org/10.1007/s00392-015-0904-6.
Malfertheiner MV, Lerzer C, Kolb L et al (2017) Whom are we treating with adaptive servo-ventilation? A clinical post hoc analysis. Clin Res Cardiol. https://doi.org/10.1007/s00392-017-1112-3
Bitter T, Faber L, Hering D et al (2009) Sleep-disordered breathing in heart failure with normal left ventricular ejection fraction. Eur J Heart Fail 11(6):602–608. https://doi.org/10.1093/eurjhf/hfp057
Herrscher TE, Akre H, Overland B et al (2011) High prevalence of sleep apnea in heart failure outpatients: even in patients with preserved systolic function. J Card Fail 17(5):420–425. https://doi.org/10.1016/j.cardfail.2011.01.013
McMurray JJ, Adamopoulos S, Anker SD et al (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 14(8):803–869. https://doi.org/10.1093/eurjhf/hfs105
Kwon BJ, Kim DB, Jang SW et al (2010) Prognosis of heart failure patients with reduced and preserved ejection fraction and coexistent chronic obstructive pulmonary disease. Eur J Heart Fail 12(12):1339–1344. https://doi.org/10.1093/eurjhf/hfq157
Komajda M, Lam CS (2014) Heart failure with preserved ejection fraction: a clinical dilemma. Eur Heart J 35(16):1022–1032. https://doi.org/10.1093/eurheartj/ehu067
Irizarry Pagan EE, Vargas PE, Lopez-Candales A (2016) The clinical dilemma of heart failure with preserved ejection fraction: an update on pathophysiology and management for physicians. Postgrad Med J 92(1088):346–355. https://doi.org/10.1136/postgradmedj-2015-133859
Lam CS, Donal E, Kraigher-Krainer E et al (2011) Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail 13(1):18–28. https://doi.org/10.1093/eurjhf/hfq121
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8):891–975. https://doi.org/10.1002/ejhf.592
Ponikowski P, Voors AA, Anker SD et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Practice parameters for the indications for polysomnography and related procedures (1997) Polysomnography task force, American sleep disorders association standards of practice committee. Sleep 20(6):406–422
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events: deliberations of the sleep apnea definitions task force of the american academy of sleep medicine. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med 8(5):597–619. https://doi.org/10.5664/jcsm.2172
Iber CAAoSM (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. American Academy of Sleep Medicine, Westchester
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Johns MW (1994) Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep 17(8):703–710
Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults (2016) An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17(4):412. https://doi.org/10.1093/ehjci/jew041
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J 28(20):2539
Bitter T, Westerheide N, Faber L et al (2010) Adaptive servoventilation in diastolic heart failure and Cheyne–Stokes respiration. Eur Respir J 36(2):385–392. https://doi.org/10.1183/09031936.00045609
Yoshihisa A, Suzuki S, Yamaki T et al (2013) Impact of adaptive servo-ventilation on cardiovascular function and prognosis in heart failure patients with preserved left ventricular ejection fraction and sleep-disordered breathing. Eur J Heart Fail 15(5):543–550. https://doi.org/10.1093/eurjhf/hfs197
Arzt M, Schroll S, Series F et al (2013) Auto-servoventilation in heart failure with sleep apnoea: a randomised controlled trial. Eur Respir J 42(5):1244–1254
Priefert H-J, Hetzenecker A, Escourrou P et al (2017) Effects of adaptive servo-ventilation on ventricular arrhythmias in patients with stable congestive heart failure and sleep-disordered breathing. Somnologie 21(1):19–27. https://doi.org/10.1007/s11818-016-0072-6
Mehra R, Wang L, Andrews N et al (2017) Dissociation of objective and subjective daytime sleepiness and biomarkers of systemic inflammation in sleep-disordered breathing and systolic heart failure. J Clin Sleep Med
Morgenthaler TI, Kuzniar TJ, Wolfe LF et al (2014) The complex sleep apnea resolution study: a prospective randomized controlled trial of continuous positive airway pressure versus adaptive servoventilation therapy. Sleep 37(5):927–934. https://doi.org/10.5665/sleep.3662
Javaheri S, Winslow D, McCullough P et al (2015) The Use of a fully automated automatic adaptive servoventilation algorithm in the acute and long-term treatment of central sleep apnea. Chest 148(6):1454–1461. https://doi.org/10.1378/chest.14-2966
Allam JS, Olson EJ, Gay PC et al (2007) Efficacy of adaptive servoventilation in treatment of complex and central sleep apnea syndromes. Chest 132(6):1839–1846. https://doi.org/10.1378/chest.07-1715
Brown SE, Mosko SS, Davis JA et al (2011) A retrospective case series of adaptive servoventilation for complex sleep apnea. J Clin Sleep Med 7(2):187–195
Javaheri S, Shukla R, Zeigler H et al (2007) Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure. J Am Coll Cardiol 49(20):2028–2034. https://doi.org/10.1016/j.jacc.2007.01.084
Lanfranchi PA, Braghiroli A, Bosimini E et al (1999) Prognostic value of nocturnal Cheyne–Stokes respiration in chronic heart failure. Circulation 99(11):1435–1440
Jilek C, Krenn M, Sebah D et al (2011) Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail 13(1):68–75. https://doi.org/10.1093/eurjhf/hfq183
Damy T, Margarit L, Noroc A et al (2012) Prognostic impact of sleep-disordered breathing and its treatment with nocturnal ventilation for chronic heart failure. Eur J Heart Fail 14(9):1009–1019. https://doi.org/10.1093/eurjhf/hfs085
Oldenburg O, Wellmann B, Buchholz A et al (2016) Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J 37(21):1695–1703. https://doi.org/10.1093/eurheartj/ehv624.
Oldenburg O, Arzt M, Börgel J et al (2017) Addendum zum Positionspapier “Schlafmedizin in der Kardiologie. Update 2014”. Kardiologie 11:19–20. https://doi.org/10.1007/s12181-016-0119-8
Randerath WJ, Nothofer G, Priegnitz C et al (2012) Long-term auto-servoventilation or constant positive pressure in heart failure and coexisting central with obstructive sleep apnea. Chest 142(2):440–447. https://doi.org/10.1378/chest.11-2089
Ruttanaumpawan P, Logan AG, Floras JS et al (2009) Effect of continuous positive airway pressure on sleep structure in heart failure patients with central sleep apnea. Sleep 32(1):91–98
Bristow MR, Kao DP, Breathett KK et al (2017) Structural and functional phenotyping of the failing heart: is the left ventricular ejection fraction obsolete? JACC Heart Fail 5(11):772–781. https://doi.org/10.1016/j.jchf.2017.09.009
Borlaug BA, Redfield MM (2011) Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation 123(18):2006–2013. https://doi.org/10.1161/CIRCULATIONAHA.110.954388 (discussion 14)
Lekavich CL, Barksdale DJ, Neelon V et al (2015) Heart failure preserved ejection fraction (HFpEF): an integrated and strategic review. Heart Fail Rev 20(6):643–653. https://doi.org/10.1007/s10741-015-9506-7
Linz D, Fox H, Bitter T et al (2016) Impact of SERVE-HF on management of sleep disordered breathing in heart failure: a call for further studies. Clin Res Cardiol 105(7):563–570. https://doi.org/10.1007/s00392-016-0970-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Arzt reports grants and personal fees from Philips Respironics, grants and personal fees from ResMed, outside the submitted work. All other authors report no conflict of interest.
Rights and permissions
About this article
Cite this article
Heider, K., Arzt, M., Lerzer, C. et al. Adaptive servo-ventilation and sleep quality in treatment emergent central sleep apnea and central sleep apnea in patients with heart disease and preserved ejection fraction. Clin Res Cardiol 107, 421–429 (2018). https://doi.org/10.1007/s00392-018-1203-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1203-9