Abstract
Introduction
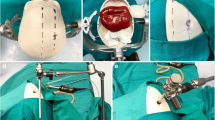
The practice of neuroendoscopic procedures requires many years of training to obtain the adequate skills to perform these operations safely. In this study, we present a new pediatric neuroendoscopic simulator that facilitates training.
Description of the simulator
This realistic simulator was built with a synthetic thermo-retractile and thermo-sensible rubber called Neoderma® which, when combined with different polymers, produces more than 30 different formulae, which present textures, consistencies, and mechanical resistances similar to many human tissues. Silicon and fiberglass molds, in the shape of the cerebral ventricles, constitute the basic structure of the neuroendoscopic training module. The module offers the possibility for practicing many basic neuroendoscopic techniques such as: navigating the ventricular system to visualize important anatomic landmarks (e.g., septal and thalamostriate veins, foramen of Monro, temporal horns, aqueduct, and fourth ventricle), performing third ventriculostomy and choroid plexus cauterization, and resecting intraventricular “tumors” that bleed.
Conclusion
It is important to emphasize that it is possible to perform with this simulator not only the rigid but also the flexible endoscopy, with good correspondence to reality and no risks. Notable future perspectives can be considered regarding this new pediatric simulator, for example, to improve the learning curve for nonexperienced neurosurgeons and to spread the flexible endoscopy technique.








Similar content being viewed by others
References
Agrawal A, Kato Y, Sano H, Kanno T (2013) The incorporation of neuroendoscopy in neurosurgical training programs. World Neurosurg 79:S15.e11–S15.e13
Balogh AA, Preul MC, Laszlo K, Schornak M, Hickman M, Deshmukh P, Spetzler RF (2006) Multilayer image grid reconstruction technology: four-dimensional interactive image reconstruction of microsurgical neuroanatomic dissections. Neurosurgery 58:ONS157–165
Barnes RW, Lang NP, Whiteside MF (1989) Halstedian technique revisited. Innovations in teaching surgical skills. Ann Surg 210:118–121
Bouras T, Sgouros S (2011) Complications of endoscopic third ventriculostomy. A review. J Neurosurg Pediatr 7:643–649
Coelho G, Kondageski C, Vaz-Guimaraes Filho F, Ramina R, Hunhevicz SC, Daga F, Lyra MR, Cavalheiro S, Zymberg ST (2011) Frameless image-guided neuroendoscopy training in real simulators. Minim Invasive Neurosurg 54:115–118
Cohen AR, Lohani S, Manjila S, Natsupakpong S, Brown N, Cavusoglu MC (2013) Virtual reality simulation: basic concepts and use in endoscopic neurosurgery training. Childs Nerv Syst 29(8):1235–44
Filho FV, Coelho G, Cavalheiro S, Lyra M, Zymberg ST (2011) Quality assessment of a new surgical simulator for neuroendoscopic training. Neurosurg Focus 30:E17
Ganju A, Aoun SG, Daou MR et al (2013) The role of simulation in neurosurgical education: a survey of 99 United States neurosurgery program directors. World Neurosurg 80(5):e1–8
Ganju A, Kahol K, Lee P et al (2012) The effect of call on neurosurgery residents’ skills: implications for policy regarding resident call periods. J Neurosurg 116(3):478–482
Gallagher AG, Cates CU (2004) Virtual reality training for the operating room and cardiac catheterization laboratory. Lancet 364:1538–1540
Gorman PJ, Meier AH, Krummel TM (1999) Simulation and virtual reality in surgical education: real or unreal? Arch Surg 134:1203–1208
Haji FA, Dubrowski A, Drake J, de Ribaupierre S (2013) Needs assessment for simulation training in neuroendoscopy: a Canadian national survey. J Neurosurg 118(2):250–7
Kavic MS (2006) Simulators: a new use for an old paradigm. JSLS 10(3):281–3
Letterie GS (2002) How virtual reality may enhance training in obstetrics and gynecology. Am J Obstet Gynecol 187:37–40
Malone HR, Syed ON, Downes MS, D’Ambrosio AL, Quest DO, Kaiser MG (2010) Simulation in neurosurgery: a review of computer-based simulation environments and their surgical applications. Neurosurgery 67:1105–1116
Navarro R, Gil-Parra R, Reitman AJ, Olavarria G, Grant JA, Tomita T (2006) Endoscopic third ventriculostomy in children: early and late complications and their avoidance. Childs Nerv Syst 22:506–513
Paas FG (1992) Training strategies for attaining transfer of problem-solving skill in statistics: a cognitive-load approach. J Educ Psychol 84:429–434
Paas FG, Van Merriënboer JJ, Adam JJ (1994) Measurement of cognitive load in instructional research. Percept Mot Skills 79:419–430
ProDelphus (2011) The importance of surgical simulators. Available at: http://www.prodelphus.com. Accessed December 10.
Reznick RK (1993) Teaching and testing technical skills. Am J Surg 165:358–361
Sachdeva AK, Loiacono LA, Amiel GE, Blair PG, Friedman M, Roslyn JJ (1995) Variability in the clinical skills of residents entering training programs in surgery. Surgery 118:300–308
Schroeder HWS, Niendorf WR, Gaab MR (2002) Complications of endoscopic third ventriculostomy. J Neurosurg 96:1032–1040
Stone S, Warf BC (2014). Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment for infant hydrocephalus: a prospective North American series. J Neurosurg Pediatr.
Thomas WEG (2008) The making of a surgeon. Surgery 26:400–402
Walt AJ (1994) The uniqueness of American surgical education and its preservation. Bull Am Coll Surg 79:8–20
Warf BC (2005) Comparison of endoscopic third ventriculostomy alone and combined with choroid plexus cauterization in infants younger than 1 year of age: a prospective study in 550 African children. J Neurosurg 103:475–481, 6 Suppl Pediatrics
Warf BC (2007) Endoscopic third ventriculostomy combined with choroid plexus cauterization for pediatric hydrocephalus. Clin Neurol 54:78–82
Warf BC, Campbell JW (2008) Combined endoscopic third ventriculostomy and choroid plexus cauterization (ETV/CPC) as primary treatment of hydrocephalus for infants with myelomeningocele: long-term results of a prospective intention to treat study in 115 African infants. J Neurosurg Pediatr 2:310–316
Warf BC, Campbell JW, Riddle E (2011) Initial experience with combined endoscopic third ventriculostomy and choroid plexus cauterization for post-hemorrhagic hydrocephalus of prematurity: the importance of pre-pontine cistern status and the predictive value of FIESTA MRI imaging. Childs Nerv Syst 27:1063–1071
Winckel CP, Reznick RK, Cohen R, Taylor B (1994) Reliability and construct validity of a structured technical skills assessment form. Am J Surg 167:423–427
Zymberg S, Vaz-Guimaraes Filho F, Lyra M (2010) Neuroendoscopic training: presentation of a new real simulator. Minim Invasive Neurosurg 53:44–46
Zymberg ST, Cavalheiro S (1996) Neuroendoscopia. A propósito de 30 casos. Rev Neurociências 4:57–62
Acknowledgments
The authors thank the plastic artists: Jair Lyra; Georgina Barretto, and Josemi Fabricio da Silva for their attendance and notable dedication in developing the simulators; Maíra Coelho R. Caselato and Valéria Aires Cruz for their assistance in preparing the pictures.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coelho, G., Zymberg, S., Lyra, M. et al. New anatomical simulator for pediatric neuroendoscopic practice. Childs Nerv Syst 31, 213–219 (2015). https://doi.org/10.1007/s00381-014-2538-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-014-2538-9