Abstract
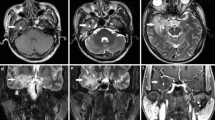
Radiotherapy (RT) is an effective treatment for head and neck cancer (HNC). Radiation-induced temporal lobe injury (TLI) is a serious complication of RT. Late symptoms of radiation-induced TLI are irreversible and manifest as memory loss, cognitive impairment, and even temporal lobe necrosis (TLN). It is currently believed that the mechanism of radiation-induced TLI involves microvascular injury, neuron and neural stem cell injury, glial cell damage, inflammation, and the production of free radicals. Significant RT-related structural changes and dose-dependent changes in gray matter (GM) and white matter (WM) volume and morphology were observed through computed tomography (CT) and magnetic resonance imaging (MRI) which were common imaging assessment tools. Diffusion tensor imaging (DTI), dispersion kurtosis imaging (DKI), susceptibility-weighted imaging (SWI), resting-state functional magnetic resonance (rs-fMRI), magnetic resonance spectroscopy (MRS), and positron emission tomography (PET) can be used for early diagnosis and prognosis evaluation according to functional, molecular, and cellular processes of TLI. Early diagnosis of TLI is helpful to reduce the incidence of TLN and its related complications. This review summarizes the clinical features, mechanisms, and imaging of radiation-induced TLI in HNC patients.
Key Points
• Radiation-induced temporal lobe injury (TLI) is a clinical complication and its symptoms mainly include memory impairment, headache, and cognitive impairment.
• The mechanisms of TLI include microvascular injury, cell injury, and inflammatory and free radical injury. Significant RT-related structural changes and dose-dependent changes in TL volume and morphology were observed through CT and MRI.
• SWI, MRS, DTI, and DKI and other imaging examinations can detect anatomical and functional, molecular, and cellular changes of TLI.



Similar content being viewed by others
Abbreviations
- Ang:
-
Angiopoietin
- Ang-2:
-
Angiopoietin-2
- BBB:
-
Blood-brain barrier
- CCR2:
-
Chemokine (C-C motif) receptor 2
- CMBs:
-
Cerebral microbleeds
- CNS:
-
Central nervous system
- COX-2:
-
Cyclocyte-2
- CT:
-
Computed tomography
- CXCR4:
-
CXC chemokine receptor 4
- D1cc :
-
The dose delivered to the 1-cm3 volume
- DKI:
-
Dispersion kurtosis imaging
- DTI:
-
Diffusion tensor imaging
- ERK1/2:
-
Extracellular regulated protein kinases 1/2
- fALFF:
-
Fractional amplitude of low-frequency fluctuation
- GM:
-
Gray matter
- hESC:
-
Human embryonic stem cells
- HIT:
-
Heavy ion therapy
- hMSC:
-
Human mesenchymal stem cells
- HNC:
-
Head and neck cancer
- IL:
-
Interleukin
- IMRT:
-
Intensity-modulated radiation therapy
- LPS:
-
Lipopolysaccharide
- MEK1:
-
Mitogen-activated protein kinase kinase 1
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- NF-κB:
-
Nuclear factor kappa-B
- NGF:
-
Nerve growth factor
- NPC:
-
Nasopharyngeal carcinoma
- NSCs:
-
Neural stem cells
- P2Y6R:
-
Purinergic receptor P2Y6 receptor
- PBT:
-
Proton beam therapy
- PET:
-
Positron emission tomography
- PET:
-
Positron emission tomography
- RIBI:
-
Radiation-induced brain injury
- ROS:
-
Reactive oxygen species
- rs-fMRI:
-
Resting-state functional magnetic resonance
- RT:
-
Radiotherapy
- SDF-1:
-
Stromal cell-derived factor 1
- SWI:
-
Susceptibility-weighted imaging
- T1WI:
-
T1-weighted image
- T2WI:
-
T2-weighted image
- TL:
-
Temporal lobe
- TLI:
-
Temporal lobe injury
- TLN:
-
Temporal lobe necrosis
- TNF-α:
-
Tumor necrosis factor-alpha
- VEGF:
-
Vascular endothelial growth factor
- VMAT:
-
Volumetric modulated arc therapy
- WM:
-
White matter
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386. https://doi.org/10.1002/ijc.29210
Huang J, Kong FF, Oei RW, Zhai RP, Hu CS, Ying HM (2019) Dosimetric predictors of temporal lobe injury after intensity-modulated radiotherapy for T4 nasopharyngeal carcinoma: a competing risk study. Radiat Oncol 14:31. https://doi.org/10.1186/s13014-019-1229-9
Lu L, Sheng Y, Zhang G et al (2018) Temporal lobe injury patterns following intensity modulated radiotherapy in a large cohort of nasopharyngeal carcinoma patients. Oral Oncol 85:8–14. https://doi.org/10.1016/j.oraloncology.2018.07.020
Zhou X, Liu P, Wang X (2020) Temporal lobe necrosis following radiotherapy in nasopharyngeal carcinoma: new insight into the management. Front Oncol 10:593487. https://doi.org/10.3389/fonc.2020.593487
Belov OV, Batmunkh M, Incerti S, Lkhagva O (2016) Radiation damage to neuronal cells: simulating the energy deposition and water radiolysis in a small neural network. Phys Med 32:1510–1520. https://doi.org/10.1016/j.ejmp.2016.11.004
Tseng BP, Giedzinski E, Izadi A et al (2014) Functional consequences of radiation-induced oxidative stress in cultured neural stem cells and the brain exposed to charged particle irradiation. Antioxid Redox Signal 20:1410–1422. https://doi.org/10.1089/ars.2012.5134
Chong VF, Fan YF, Mukherji SK (2000) Radiation-induced temporal lobe changes: CT and MR imaging characteristics. AJR Am J Roentgenol 175:431–436. https://doi.org/10.2214/ajr.175.2.1750431
Liyan L, Si W, Qian W et al (2018) Diffusion kurtosis as an in vivo imaging marker of early radiation-induced changes in radiation-induced temporal lobe necrosis in nasopharyngeal carcinoma patients. Clin Neuroradiol 28:413–420. https://doi.org/10.1007/s00062-017-0585-9
Chen W, Qiu S, Li J et al (2015) Diffusion tensor imaging study on radiation-induced brain injury in nasopharyngeal carcinoma during and after radiotherapy. Tumori 101:487–490. https://doi.org/10.5301/tj.5000348
Wang HZ, Qiu SJ, Lv XF et al (2012) Diffusion tensor imaging and 1H-MRS study on radiation-induced brain injury after nasopharyngeal carcinoma radiotherapy. Clin Radiol 67:340–345. https://doi.org/10.1016/j.crad.2011.09.008
Co J, De Moraes MV, Katznelson R et al (2019) Hyperbaric oxygen for radiation necrosis of the brain. Can J Neurol Sci 47:1–8. https://doi.org/10.1017/cjn.2019.290
Li YQ, Chen P, Jain V, Reilly RM, Wong CS (2004) Early radiation-induced endothelial cell loss and blood-spinal cord barrier breakdown in the rat spinal cord. Radiat Res 161:143–152. https://doi.org/10.1667/rr3117
Pena LA, Fuks Z, Kolesnick RN (2000) Radiation-induced apoptosis of endothelial cells in the murine central nervous system: protection by fibroblast growth factor and sphingomyelinase deficiency. Cancer Res 60:321–327
Shen Q, Lin F, Rong X et al (2016) Temporal cerebral microbleeds are associated with radiation necrosis and cognitive dysfunction in patients treated for nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 94:1113–1120. https://doi.org/10.1016/j.ijrobp.2015.11.037
Ai X, Ye Z, Yao Y et al (2020) Endothelial autophagy: an effective target for radiation-induced cerebral capillary damage. Sci Rep 10:614. https://doi.org/10.1038/s41598-019-57234-9
Deng Z, Huang H, Wu X, Wu M, He G, Guo J (2017) Distinct expression of various angiogenesis factors in mice brain after whole-brain irradiation by X-ray. Neurochem Res 42:625–633. https://doi.org/10.1007/s11064-016-2118-3
Lee WH, Cho HJ, Sonntag WE, Lee YW (2011) Radiation attenuates physiological angiogenesis by differential expression of VEGF, Ang-1, tie-2 and Ang-2 in rat brain. Radiat Res 176:753–760. https://doi.org/10.1667/rr2647.1
Nonoguchi N, Miyatake S, Fukumoto M et al (2011) The distribution of vascular endothelial growth factor-producing cells in clinical radiation necrosis of the brain: pathological consideration of their potential roles. J Neurooncol 105:423–431. https://doi.org/10.1007/s11060-011-0610-9
Maisonpierre PC, Suri C, Jones PF et al (1997) Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 277:55–60. https://doi.org/10.1126/science.277.5322.55
Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J (2000) Vascular-specific growth factors and blood vessel formation. Nature 407:242–248. https://doi.org/10.1038/35025215
Wu Q, Fang Y, Zhang X et al (2020) Effect of X-rays on transcript expression of rat brain microvascular endothelial cells: role of calcium signaling in X-ray-induced endothelium damage. Biosci Rep 40. https://doi.org/10.1042/BSR20193760
Wu VWC, Tam SY (2020) Radiation induced temporal lobe necrosis in nasopharyngeal cancer patients after radical external beam radiotherapy. Radiat Oncol 15:7. https://doi.org/10.1186/s13014-020-01560-0
Sabirzhanov B, Makarevich O, Barrett J, Jackson IL, Faden AI, Stoica BA (2020) Down-regulation of miR-23a-3p mediates irradiation-induced neuronal apoptosis. Int J Mol Sci 21. https://doi.org/10.3390/ijms21103695
Kempf SJ, Moertl S, Sepe S et al (2015) Low-dose ionizing radiation rapidly affects mitochondrial and synaptic signaling pathways in murine hippocampus and cortex. J Proteome Res 14:2055–2064. https://doi.org/10.1021/acs.jproteome.5b00114
Eriksson P, Fischer C, Stenerlow B, Fredriksson A, Sundell-Bergman S (2010) Interaction of gamma-radiation and methyl mercury during a critical phase of neonatal brain development in mice exacerbates developmental neurobehavioural effects. Neurotoxicology 31:223–229. https://doi.org/10.1016/j.neuro.2010.01.002
Parihar VK, Pasha J, Tran KK, Craver BM, Acharya MM, Limoli CL (2015) Persistent changes in neuronal structure and synaptic plasticity caused by proton irradiation. Brain Struct Funct 220:1161–1171. https://doi.org/10.1007/s00429-014-0709-9
Du Y, Zhang J, Zheng Q et al (2014) Heavy ion and X-ray irradiation alter the cytoskeleton and cytomechanics of cortical neurons. Neural Regen Res 9:1129–1137. https://doi.org/10.4103/1673-5374.135315
Wang TM, Shen GP, Chen MY et al (2019) Genome-wide association study of susceptibility loci for radiation-induced brain injury. J Natl Cancer Inst 111:620–628. https://doi.org/10.1093/jnci/djy150
Pereira Dias G, Hollywood R, Bevilaqua MC et al (2014) Consequences of cancer treatments on adult hippocampal neurogenesis: implications for cognitive function and depressive symptoms. Neuro Oncol 16:476–492. https://doi.org/10.1093/neuonc/not321
Wang Y, Zhou K, Li T et al (2017) Inhibition of autophagy prevents irradiation-induced neural stem and progenitor cell death in the juvenile mouse brain. Cell Death Dis 8:e2694. https://doi.org/10.1038/cddis.2017.120
Monje ML, Palmer T (2003) Radiation injury and neurogenesis. Curr Opin Neurol 16:129–134. https://doi.org/10.1097/01.wco.0000063772.81810.b7
Dong X, Luo M, Huang G et al (2015) Relationship between irradiation-induced neuro-inflammatory environments and impaired cognitive function in the developing brain of mice. Int J Radiat Biol 91:224–239. https://doi.org/10.3109/09553002.2014.988895
Kurita H, Kawahara N, Asai A, Ueki K, Shin M, Kirino T (2001) Radiation-induced apoptosis of oligodendrocytes in the adult rat brain. Neurol Res 23:869–874. https://doi.org/10.1179/016164101101199324
Szerlip N, Rutter C, Ram N et al (2011) Factors impacting volumetric white matter changes following whole brain radiation therapy. J Neurooncol 103:111–119. https://doi.org/10.1007/s11060-010-0358-7
Nordal RA, Wong CS (2005) Molecular targets in radiation-induced blood-brain barrier disruption. Int J Radiat Oncol Biol Phys 62:279–287. https://doi.org/10.1016/j.ijrobp.2005.01.039
Wei J, Wang B, Wang H et al (2019) Radiation-induced normal tissue damage: oxidative stress and epigenetic mechanisms. Oxidative Med Cell Longev 2019:3010342. https://doi.org/10.1155/2019/3010342
Nakamura M, Yamasaki T, Ueno M et al (2019) Radiation-induced redox alteration in the mouse brain. Free Radic Biol Med 143:412–421. https://doi.org/10.1016/j.freeradbiomed.2019.08.020
Zhao W, Diz DI, Robbins ME (2007) Oxidative damage pathways in relation to normal tissue injury. Br J Radiol 80 Spec No 1:S23-31. 10.1259/bjr/18237646
Belarbi K, Jopson T, Tweedie D et al (2012) TNF-alpha protein synthesis inhibitor restores neuronal function and reverses cognitive deficits induced by chronic neuroinflammation. J Neuroinflammation 9:23. https://doi.org/10.1186/1742-2094-9-23
Rosi S, Ramirez-Amaya V, Vazdarjanova A et al (2009) Accuracy of hippocampal network activity is disrupted by neuroinflammation: rescue by memantine. Brain 132:2464–2477. https://doi.org/10.1093/brain/awp148
Wu L, Chung YL (2019) Tumor-infiltrating T cell receptor-beta repertoires are linked to the risk of late chemoradiation-induced temporal lobe necrosis in locally advanced nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 104:165–176. https://doi.org/10.1016/j.ijrobp.2019.01.002
Guan W, Xie K, Fan Y et al (2020) Development and validation of a nomogram for predicting radiation-induced temporal lobe injury in nasopharyngeal carcinoma. Front Oncol 10:594494. https://doi.org/10.3389/fonc.2020.594494
Lumniczky K, Szatmari T, Safrany G (2017) Ionizing radiation-induced immune and inflammatory reactions in the brain. Front Immunol 8:517. https://doi.org/10.3389/fimmu.2017.00517
Prinz M, Priller J (2010) Tickets to the brain: role of CCR2 and CX3CR1 in myeloid cell entry in the CNS. J Neuroimmunol 224:80–84. https://doi.org/10.1016/j.jneuroim.2010.05.015
Belarbi K, Jopson T, Arellano C, Fike JR, Rosi S (2013) CCR2 deficiency prevents neuronal dysfunction and cognitive impairments induced by cranial irradiation. Cancer Res 73:1201–1210. https://doi.org/10.1158/0008-5472.CAN-12-2989
Dong XR, Luo M, Fan L et al (2010) Corilagin inhibits the double strand break-triggered NF-kappaB pathway in irradiated microglial cells. Int J Mol Med 25:531–536
Biber K, Neumann H, Inoue K, Boddeke HW (2007) Neuronal' on ' and' off ' signals control microglia. Trends Neurosci 30:596–602. https://doi.org/10.1016/j.tins.2007.08.007
Deng Z, Sui G, Rosa PM, Zhao W (2012) Radiation-induced c-Jun activation depends on MEK1-ERK1/2 signaling pathway in microglial cells. PLoS One 7:e36739. https://doi.org/10.1371/journal.pone.0036739
Kalm M, Roughton K, Blomgren K (2013) Lipopolysaccharide sensitized male and female juvenile brains to ionizing radiation. Cell Death Dis 4:e962. https://doi.org/10.1038/cddis.2013.482
Behin A, Delattre JY (2004) Complications of radiation therapy on the brain and spinal cord. Semin Neurol 24:405–417. https://doi.org/10.1055/s-2004-861535
Tofilon PJ, Fike JR (2000) The radioresponse of the central nervous system: a dynamic process. Radiat Res 153:357–370. https://doi.org/10.1667/0033-7587(2000)153[0357:trotcn]2.0.co;2
Tang Y, Luo D, Rong X, Shi X, Peng Y (2012) Psychological disorders, cognitive dysfunction and quality of life in nasopharyngeal carcinoma patients with radiation-induced brain injury. PLoS One 7:e36529. https://doi.org/10.1371/journal.pone.0036529
Welsh LC, Dunlop AW, McGovern T et al (2014) Neurocognitive function after (chemo)-radiotherapy for head and neck cancer. Clin Oncol (R Coll Radiol) 26:765–775. https://doi.org/10.1016/j.clon.2014.06.014
He L, Xiao J, Wei Z et al (2020) Toxicity and dosimetric analysis of nasopharyngeal carcinoma patients undergoing radiotherapy with IMRT or VMAT: a regional center ' s experience. Oral Oncol 109:104978. https://doi.org/10.1016/j.oraloncology.2020.104978
Hsiao KY, Yeh SA, Chang CC, Tsai PC, Wu JM, Gau JS (2010) Cognitive function before and after intensity-modulated radiation therapy in patients with nasopharyngeal carcinoma: a prospective study. Int J Radiat Oncol Biol Phys 77:722–726. https://doi.org/10.1016/j.ijrobp.2009.06.080
Su SF, Huang Y, Xiao WW et al (2012) Clinical and dosimetric characteristics of temporal lobe injury following intensity modulated radiotherapy of nasopharyngeal carcinoma. Radiother Oncol 104:312–316. https://doi.org/10.1016/j.radonc.2012.06.012
Feng M, Huang Y, Fan X, Xu P, Lang J, Wang D (2018) Prognostic variables for temporal lobe injury after intensity modulated-radiotherapy of nasopharyngeal carcinoma. Cancer Med 7:557–564. https://doi.org/10.1002/cam4.1291
Guo Z, Han L, Yang Y et al (2018) Longitudinal brain structural alterations in patients with nasopharyngeal carcinoma early after radiotherapy. Neuroimage Clin 19:252–259. https://doi.org/10.1016/j.nicl.2018.04.019
Lin J, Lv X, Niu M et al (2017) Radiation-induced abnormal cortical thickness in patients with nasopharyngeal carcinoma after radiotherapy. Neuroimage Clin 14:610–621. https://doi.org/10.1016/j.nicl.2017.02.025
Lv XF, Zheng XL, Zhang WD et al (2014) Radiation-induced changes in normal-appearing gray matter in patients with nasopharyngeal carcinoma: a magnetic resonance imaging voxel-based morphometry study. Neuroradiology 56:423–430. https://doi.org/10.1007/s00234-014-1338-y
Lee AW, Cheng LO, Ng SH et al (1990) Magnetic resonance imaging in the clinical diagnosis of late temporal lobe necrosis following radiotherapy for nasopharyngeal carcinoma. Clin Radiol 42:24–31. https://doi.org/10.1016/s0009-9260(05)81617-4
Lee AW, Ng SH, Ho JH et al (1988) Clinical diagnosis of late temporal lobe necrosis following radiation therapy for nasopharyngeal carcinoma. Cancer 61:1535–1542. https://doi.org/10.1002/1097-0142(19880415)61:8<1535::aid-cncr2820610809>3.0.co;2-e
Zhou GQ, Yu XL, Chen M et al (2013) Radiation-induced temporal lobe injury for nasopharyngeal carcinoma: a comparison of intensity-modulated radiotherapy and conventional two-dimensional radiotherapy. PLoS One 8:e67488. https://doi.org/10.1371/journal.pone.0067488
Hsu YC, Wang LF, Lee KW, Ho KY, Huang CJ, Kuo WR (2005) Cerebral radionecrosis in patients with nasopharyngeal carcinoma. Kaohsiung J Med Sci 21:452–459. https://doi.org/10.1016/s1607-551x(09)70150-0
Du QH, Gan YX, Wang RS et al (2021) Half-brain delineation for prediction of radiation-induced temporal lobe injury in nasopharyngeal carcinoma receiving intensity-modulated radiotherapy. Front Oncol 11:599942. https://doi.org/10.3389/fonc.2021.599942
Zeng L, Huang SM, Tian YM et al (2015) Normal tissue complication probability model for radiation-induced temporal lobe injury after intensity-modulated radiation therapy for nasopharyngeal carcinoma. Radiology 276:243–249. https://doi.org/10.1148/radiol.14141721
Lam TC, Wong FC, Leung TW, Ng SH, Tung SY (2012) Clinical outcomes of 174 nasopharyngeal carcinoma patients with radiation-induced temporal lobe necrosis. Int J Radiat Oncol Biol Phys 82:e57–e65. https://doi.org/10.1016/j.ijrobp.2010.11.070
Tang Y, Rong X, Hu W et al (2014) Effect of edaravone on radiation-induced brain necrosis in patients with nasopharyngeal carcinoma after radiotherapy: a randomized controlled trial. J Neurooncol 120:441–447. https://doi.org/10.1007/s11060-014-1573-4
Abdel-Magied N, Shedid SM, Ahmed AG (2019) Mitigating effect of biotin against irradiation-induced cerebral cortical and hippocampal damage in the rat brain tissue. Environ Sci Pollut Res Int 26:13441–13452. https://doi.org/10.1007/s11356-019-04806-x
Peng Y, Lu K, Li Z et al (2014) Blockade of Kv1.3 channels ameliorates radiation-induced brain injury. Neuro Oncol 16:528–539. https://doi.org/10.1093/neuonc/not221
Jenrow KA, Brown SL, Lapanowski K, Naei H, Kolozsvary A, Kim JH (2013) Selective inhibition of microglia-mediated neuroinflammation mitigates radiation-induced cognitive impairment. Radiat Res 179:549–556. https://doi.org/10.1667/RR3026.1
Schnegg CI, Greene-Schloesser D, Kooshki M, Payne VS, Hsu FC, Robbins ME (2013) The PPARdelta agonist GW0742 inhibits neuroinflammation, but does not restore neurogenesis or prevent early delayed hippocampal-dependent cognitive impairment after whole-brain irradiation. Free Radic Biol Med 61:1–9. https://doi.org/10.1016/j.freeradbiomed.2013.03.002
Zhang Y, Cheng Z, Wang C, Ma H, Meng W, Zhao Q (2016) Neuroprotective effects of kukoamine a against radiation-induced rat brain injury through inhibition of oxidative stress and neuronal apoptosis. Neurochem Res 41:2549–2558. https://doi.org/10.1007/s11064-016-1967-0
Wang X, Ying H, Zhou Z, Hu C, Eisbruch A (2011) Successful treatment of radiation-induced temporal lobe necrosis with mouse nerve growth factor. J Clin Oncol 29:e166–e168. https://doi.org/10.1200/JCO.2010.31.7081
Heo JI, Kim KI, Woo SK et al (2019) Stromal cell-derived factor 1 protects brain vascular endothelial cells from radiation-induced brain damage. Cells 8(10). https://doi.org/10.3390/cells8101230
Zhuang H, Shi S, Yuan Z, Chang JY (2019) Bevacizumab treatment for radiation brain necrosis: mechanism, efficacy and issues. Mol Cancer 18:21. https://doi.org/10.1186/s12943-019-0950-1
Zhang B, Lian Z, Zhong L et al (2020) Machine-learning based MRI radiomics models for early detection of radiation-induced brain injury in nasopharyngeal carcinoma. BMC Cancer 20:502. https://doi.org/10.1186/s12885-020-06957-4
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures, they are data. Radiology 278:563–577. https://doi.org/10.1148/radiol.2015151169
Lv X, He H, Yang Y et al (2019) Radiation-induced hippocampal atrophy in patients with nasopharyngeal carcinoma early after radiotherapy: a longitudinal MR-based hippocampal subfield analysis. Brain Imaging Behav 13:1160–1171. https://doi.org/10.1007/s11682-018-9931-z
Yang Y, Lin X, Li J et al (2019) Aberrant brain activity at early delay stage post-radiotherapy as a biomarker for predicting neurocognitive dysfunction late-delayed in patients with nasopharyngeal carcinoma. Front Neurol 10:752. https://doi.org/10.3389/fneur.2019.00752
Shams S, Martola J, Cavallin L et al (2015) SWI or T2*: which MRI sequence to use in the detection of cerebral microbleeds? The Karolinska Imaging Dementia Study. AJNR Am J Neuroradiol 36:1089–1095. https://doi.org/10.3174/ajnr.A4248
Haller S, Montandon ML, Lazeyras F et al (2016) Radiologic-histopathologic correlation of cerebral microbleeds using pre-mortem and post-mortem MRI. PLoS One 11:e0167743. https://doi.org/10.1371/journal.pone.0167743
Neu MA, Tanyildizi Y, Wingerter A et al (2018) Susceptibility-weighted magnetic resonance imaging of cerebrovascular sequelae after radiotherapy for pediatric brain tumors. Radiother Oncol 127:280–286. https://doi.org/10.1016/j.radonc.2018.03.010
Tanino T, Kanasaki Y, Tahara T et al (2013) Radiation-induced microbleeds after cranial irradiation: evaluation by phase-sensitive magnetic resonance imaging with 3.0 tesla. Yonago Acta Med 56:7–12
Leng X, Fang P, Lin H et al (2017) Structural MRI research in patients with nasopharyngeal carcinoma following radiotherapy: a DTI and VBM study. Oncol Lett 14:6091–6096. https://doi.org/10.3892/ol.2017.6968
Tringale KR, Nguyen TT, Karunamuni R et al (2019) Quantitative imaging biomarkers of damage to critical memory regions are associated with post-radiation therapy memory performance in brain tumor patients. Int J Radiat Oncol Biol Phys 105:773–783. https://doi.org/10.1016/j.ijrobp.2019.08.003
Viallon M, Cuvinciuc V, Delattre B et al (2015) State-of-the-art MRI techniques in neuroradiology: principles, pitfalls, and clinical applications. Neuroradiology 57:441–467. https://doi.org/10.1007/s00234-015-1500-1
Klos J, van Laar PJ, Sinnige PF et al (2019) Quantifying effects of radiotherapy-induced microvascular injury; review of established and emerging brain MRI techniques. Radiother Oncol 140:41–53. https://doi.org/10.1016/j.radonc.2019.05.020
Zhu J, Zhuo C, Qin W et al (2015) Performances of diffusion kurtosis imaging and diffusion tensor imaging in detecting white matter abnormality in schizophrenia. Neuroimage Clin 7:170–176. https://doi.org/10.1016/j.nicl.2014.12.008
Wu G, Luo SS, Balasubramanian PS et al (2020) Early stage markers of late delayed neurocognitive decline using diffusion kurtosis imaging of temporal lobe in nasopharyngeal carcinoma patients. J Cancer 11:6168–6177. https://doi.org/10.7150/jca.48759
Barajas RF, Chang JS, Sneed PK, Segal MR, McDermott MW, Cha S (2009) Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 30:367–372. https://doi.org/10.3174/ajnr.A1362
Ding Z, Zhang H, Lv XF et al (2018) Radiation-induced brain structural and functional abnormalities in presymptomatic phase and outcome prediction. Hum Brain Mapp 39:407–427. https://doi.org/10.1002/hbm.23852
Lo EH, DeLaPaz RL, Frankel KA et al (1991) MRI and PET of delayed heavy-ion radiation injury in the rabbit brain. Int J Radiat Oncol Biol Phys 20:689–696. https://doi.org/10.1016/0360-3016(91)90010-2
Li H, Deng L, Bai HX et al (2018) Diagnostic accuracy of amino acid and FDG-PET in differentiating brain metastasis recurrence from radionecrosis after radiotherapy: a systematic review and meta-analysis. AJNR Am J Neuroradiol 39:280–288. https://doi.org/10.3174/ajnr.A5472
Qiao Z, Zhao X, Wang K et al (2019) Utility of dynamic susceptibility contrast perfusion-weighted MR imaging and (11)C-methionine PET/CT for differentiation of tumor recurrence from radiation injury in patients with high-grade gliomas. AJNR Am J Neuroradiol 40:253–259. https://doi.org/10.3174/ajnr.A5952
Lohmann P, Stoffels G, Ceccon G et al (2017) Radiation injury vs. recurrent brain metastasis: combining textural feature radiomics analysis and standard parameters may increase (18)F-FET PET accuracy without dynamic scans. Eur Radiol 27:2916–2927. https://doi.org/10.1007/s00330-016-4638-2
Hatzoglou V, Yang TJ, Omuro A et al (2016) A prospective trial of dynamic contrast-enhanced MRI perfusion and fluorine-18 FDG PET-CT in differentiating brain tumor progression from radiation injury after cranial irradiation. Neuro Oncol 18:873–880. https://doi.org/10.1093/neuonc/nov301
Zhuo X, Huang X, Yan M et al (2019) Comparison between high-dose and low-dose intravenous methylprednisolone therapy in patients with brain necrosis after radiotherapy for nasopharyngeal carcinoma. Radiother Oncol 137:16–23. https://doi.org/10.1016/j.radonc.2019.04.015
Ishii J, Natsume A, Wakabayashi T et al (2007) The free-radical scavenger edaravone restores the differentiation of human neural precursor cells after radiation-induced oxidative stress. Neurosci Lett 423:225–230. https://doi.org/10.1016/j.neulet.2007.07.029
Li Y, Huang X, Jiang J et al (2018) Clinical variables for prediction of the therapeutic effects of bevacizumab monotherapy in nasopharyngeal carcinoma patients with radiation-induced brain necrosis. Int J Radiat Oncol Biol Phys 100:621–629. https://doi.org/10.1016/j.ijrobp.2017.11.023
Naylor AS, Bull C, Nilsson MK et al (2008) Voluntary running rescues adult hippocampal neurogenesis after irradiation of the young mouse brain. Proc Natl Acad Sci U S A 105:14632–14637. https://doi.org/10.1073/pnas.0711128105
Xing S, Fan Z, Shi L, Yang Z, Bai Y (2019) Successful treatment of brain radiation necrosis resulting from triple-negative breast cancer with Endostar and short-term hyperbaric oxygen therapy: a case report. Onco Targets Ther 12:2729–2735. https://doi.org/10.2147/OTT.S190409
Baulch JE, Acharya MM, Allen BD et al (2016) Cranial grafting of stem cell-derived microvesicles improves cognition and reduces neuropathology in the irradiated brain. Proc Natl Acad Sci U S A 113:4836–4841. https://doi.org/10.1073/pnas.1521668113
Sato Y, Shinjyo N, Sato M et al (2018) Grafting neural stem and progenitor cells into the hippocampus of juvenile, irradiated mice normalizes behavior deficits. Front Neurol 9:715. https://doi.org/10.3389/fneur.2018.00715
Bai SM, Wang Q, Yu XL et al (2018) Grafted neural stem cells show lesion-specific migration in radiation-injured rat brains. RSC Adv 8:5797–5805. https://doi.org/10.1039/C7RA10151A
Joo KM, Jin J, Kang BG et al (2012) Trans-differentiation of neural stem cells: a therapeutic mechanism against the radiation induced brain damage. PLoS One 7:e25936. https://doi.org/10.1371/journal.pone.0025936
Soria B, Martin-Montalvo A, Aguilera Y et al (2019) Human mesenchymal stem cells prevent neurological complications of radiotherapy. Front Cell Neurosci 13:204. https://doi.org/10.3389/fncel.2019.00204
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This work was supported by the National Natural Science Foundation of China (Grant number 81570344); National Key R & D Program of China (Grant number 2017YFC0112100), the Education Department Foundation of Jilin Province (Grant number JJKH20201036KJ); the Health and Family Planning Commission of Jilin Province Foundations (Grant numbers 2016Q034 and 2017J11); the Fundamental Research Funds for the Central Universities of Jilin University; and the Jilin Provincial Science and Technology Foundations (Grant number 20180414039GH and 20190201200JC).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xin Jiang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Informed consent was obtained.
Ethical approval
Not applicable
Methodology
• Review
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 2133 kb)
Rights and permissions
About this article
Cite this article
Zheng, Z., Wang, B., Zhao, Q. et al. Research progress on mechanism and imaging of temporal lobe injury induced by radiotherapy for head and neck cancer. Eur Radiol 32, 319–330 (2022). https://doi.org/10.1007/s00330-021-08164-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08164-6