Abstract
Objective
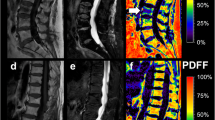
This study evaluated the diagnostic performance of the proton density fat fraction (PDFF) in predicting the progression of osteoporotic vertebral compression fractures (OVCFs).
Methods
The cohort in this retrospective study consisted of 48 patients with OVCFs who underwent spine MRI that included PDFF between December 2016 and June 2018. The patients were divided into two groups (with versus without OVCF progression, based on the radiographic results obtained at the 6-month follow-up examination). Two musculoskeletal radiologists independently calculated the PDFF of the fracture and the PDFF ratio (fracture PDFF/normal vertebrae PDFF) using regions of interest. The mean values of these parameters were compared between the two groups, and the receiver operating characteristic curves were analysed.
Results
The mean age was significantly higher in the group with OVCF progression (71.6 ± 8.4 years) than in the group without (64.8 ± 10.5 years) (p = 0.018). According to reader 1, the PDFF ratio was significantly lower in the group with OVCF progression versus that without OVCF progression (0.38 ± 0.13 vs 0.51 ± 0.20; p = 0.009), whereas the difference in the PDFF itself was not statistically significant. The PDFF ratio [area under the curve (AUC) = 0.723; 95% confidence interval (CI), 0.575–0.842] had a larger AUC than did the PDFF (AUC = 0.667; 95% CI, 0.516–0.796). The optimal cut-off value of the PDFF ratio for predicting OVCF progression was 0.42; this threshold corresponded to sensitivity, specificity, and accuracy values of 84.0%, 60.9%, and 72.9%, respectively.
Conclusion
The age and PDFF ratio can be used to predict OVCF progression.
Key Points
• Chemical shift-encoded magnetic resonance imaging provides quantitative parameters for predicting OVCF progression.
• The PDFF ratio is significantly lower in patients with OVCF progression.
• The PDFF ratio is superior to the PDFF for predicting OVCF progression.



Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CSE-MRI:
-
Chemical shift-encoded magnetic resonance imaging
- DM:
-
Diabetes mellitus
- FOV:
-
Field of view
- HTN:
-
Hypertension
- ICC:
-
Intraclass correlation coefficient
- MRS:
-
Magnetic resonance spectroscopy
- OVCF:
-
Osteoporotic vertebral compression fracture
- PDFF:
-
Proton density fat fraction
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- TE:
-
Echo time
- TR:
-
Repetition time
- VAS:
-
Visual analogue scale
References
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Gabriel SE, Tosteson AN, Leibson CL et al (2002) Direct medical costs attributable to osteoporotic fractures. Osteoporos Int 13:323–330
Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V (2012) Osteoporotic vertebral fractures: current concepts of conservative care. Br Med Bull 102:171–189
Kanchiku T, Taguchi T, Toyoda K, Fujii K, Kawai S (2003) Dynamic contrast-enhanced magnetic resonance imaging of osteoporotic vertebral fracture. Spine (Phila Pa 1976) 28:2522–2526 discussion 2522
Kanchiku T, Imajo Y, Suzuki H, Yoshida Y, Taguchi T (2014) Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech 27:E61–E65
Sugita M, Watanabe N, Mikami Y, Hase H, Kubo T (2005) Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech 18:376–381
Tsujio T, Nakamura H, Terai H et al (2011) Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976) 36:1229–1235
Ha KY, Kim YH (2013) Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos Int 24:1207–1213
Patil S, Nene AM (2014) Predictors of kyphotic deformity in osteoporotic vertebral compression fractures: a radiological study. Eur Spine J 23:2737–2742
Omi H, Yokoyama T, Ono A, Numasawa T, Wada K, Fujisawa Y (2014) Can MRI predict subsequent pseudarthrosis resulting from osteoporotic thoracolumbar vertebral fractures? Eur Spine J 23:2705–2710
Muratore M, Ferrera A, Masse A, Bistolfi A (2018) Osteoporotic vertebral fractures: predictive factors for conservative treatment failure. A systematic review. Eur Spine J 27:2565–2576
Goldstein S, Smorgick Y, Mirovsky Y, Anekstein Y, Blecher R, Tal S (2016) Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J Clin Neurosci 31:122–126
Zhang J, He X, Fan Y, Du J, Hao D (2019) Risk factors for conservative treatment failure in acute osteoporotic vertebral compression fractures (OVCFs). Arch Osteoporos 14:24
Schmeel FC, Luetkens JA, Enkirch SJ et al (2018) Proton density fat fraction (PDFF) MR imaging for differentiation of acute benign and neoplastic compression fractures of the spine. Eur Radiol 28:5001–5009
Schmeel FC, Luetkens JA, Wagenhauser PJ et al (2018) Proton density fat fraction (PDFF) MRI for differentiation of benign and malignant vertebral lesions. Eur Radiol 28:2397–2405
Zajick DC Jr, Morrison WB, Schweitzer ME, Parellada JA, Carrino JA (2005) Benign and malignant processes: normal values and differentiation with chemical shift MR imaging in vertebral marrow. Radiology 237:590–596
Kim DH, Yoo HJ, Hong SH, Choi JY, Chae HD, Chung BM (2017) Differentiation of acute osteoporotic and malignant vertebral fractures by quantification of fat fraction with a Dixon MRI sequence. AJR Am J Roentgenol 209:1331–1339
Fischer MA, Nanz D, Shimakawa A et al (2013) Quantification of muscle fat in patients with low back pain: comparison of multi-echo MR imaging with single-voxel MR spectroscopy. Radiology 266:555–563
Schmeel FC, Vomweg T, Traber F et al (2019) Proton density fat fraction MRI of vertebral bone marrow: accuracy, repeatability, and reproducibility among readers, field strengths, and imaging platforms. J Magn Reson Imaging 50:1762–1772
Sun K, Chai W, Fu C et al (2016) Diffusion-weighted imaging-guided MR spectroscopy in breast lesions using readout-segmented echo-planar imaging. Eur Radiol 26:1565–1574
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Meisamy S, Hines CD, Hamilton G et al (2011) Quantification of hepatic steatosis with T1-independent, T2-corrected MR imaging with spectral modeling of fat: blinded comparison with MR spectroscopy. Radiology 258:767–775
Kuhn JP, Hernando D, Munoz del Rio A et al (2012) Effect of multipeak spectral modeling of fat for liver iron and fat quantification: correlation of biopsy with MR imaging results. Radiology 265:133–142
Lee SH, Yoo HJ, Yu SM, Hong SH, Choi JY, Chae HD (2019) Fat quantification in the vertebral body: comparison of modified Dixon technique with single-voxel magnetic resonance spectroscopy. Korean J Radiol 20:126–133
Kim D, Kim SK, Lee SJ, Choo HJ, Park JW, Kim KY (2019) Simultaneous estimation of the fat fraction and R(2)(*) via T(2)(*)-Corrected 6-echo Dixon volumetric interpolated breath-hold examination imaging for osteopenia and osteoporosis detection: correlations with sex, age, and menopause. Korean J Radiol 20:916–930
Suh CH, Yun SJ, Jin W, Lee SH, Park SY, Ryu CW (2018) ADC as a useful diagnostic tool for differentiating benign and malignant vertebral bone marrow lesions and compression fractures: a systematic review and meta-analysis. Eur Radiol 28:2890–2902
van Vucht N, Santiago R, Lottmann B et al (2019) The Dixon technique for MRI of the bone marrow. Skeletal Radiol 48:1861–1874
Kugel H, Jung C, Schulte O, Heindel W (2001) Age- and sex-specific differences in the 1H-spectrum of vertebral bone marrow. J Magn Reson Imaging 13:263–268
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sunghoon Park.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yun, J.S., Lee, HD., Kwack, KS. et al. Use of proton density fat fraction MRI to predict the radiographic progression of osteoporotic vertebral compression fracture. Eur Radiol 31, 3582–3589 (2021). https://doi.org/10.1007/s00330-020-07529-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07529-7