Abstract
Objective
To validate a new index, the surface–length index (SLI) based on area change in a short-axis view and length reduction in the horizontal long-axis view, which is used to quickly (<1 min) detect right ventricles with an abnormal ejection fraction (EF) during a cardiac MRI examination. SLI can be used to avoid a complete delineation of the endocardial contours of normal right ventricles.
Methods
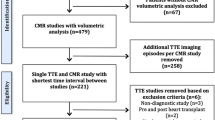
Sixty patients (group A) were retrospectively included to calibrate the SLI formula by optimisation of the area under the ROC curves and SLI thresholds were chosen to obtain 100 % sensitivity. Another 340 patients (group B) were prospectively recruited to test SLI’s capacity to detect right ventricles (RVs) with an abnormal EF (<0.5).
Results
The appropriate threshold to obtain 100 % sensitivity in group A was 0.58. In group B, with the 0.58 threshold, SLI yielded a sensitivity of 100 % and specificity of 51 %. SLI would have saved 35 % of the RV studies in our population, without inducing any diagnostic error. SLI and EF correlation was good (r 2 = 0.64).
Conclusion
SLI combines two simple RV measures, and brings significant improvement in post-processing efficiency by preselecting RVs that require a complete study.
Key Points
• Assessment of right ventricle ejection fraction (RVEF) with cine-MRI is time consuming.
• Therefore, RVEF is not always assessed during cardiac MRI.
• Surface–length index (SLI) allows rapid detection of abnormal RVEF during cardiac MRI.
• SLI saves one third of the operator time.
• Every cardiac MRI could include RVEF assessment by means of SLI.





Similar content being viewed by others
Abbreviations
- EF:
-
Ejection fraction
- FAC:
-
Fractional area change
- ROC:
-
Receiver operating characteristic
- RV:
-
Right ventricle
- SF:
-
Shortening fraction
- SLI:
-
Surface–length index
References
Selton-Suty C, Juillière Y (2009) Non-invasive investigations of the right heart: how and why? Arch Cardiovasc Dis 102:219–232
American College of Cardiology Foundation Task Force on Expert Consensus Documents, Hundley WG, Bluemke DA et al (2010) ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol 55:2614–2662
Maceira AM, Prasad SK, Khan M, Pennell DJ (2006) Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J 27:2879–2888
Bonnemains L, Mandry D, Marie PY, Micard E, Chen B, Vuissoz PA (2012) Assessment of right ventricle volumes and function by cardiac MRI: quantification of the regional and global interobserver variability. Magn Reson Med 67:1740–1746
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107:526–531
Forni G, Pozzoli M, Cannizzaro G et al (1996) Assessment of right ventricular function in patients with congestive heart failure by echocardiographic automated boundary detection. Am J Cardiol 78:1317–1321
Giusca S, Dambrauskaite V, Scheurwegs C et al (2010) Deformation imaging describes right ventricular function better than longitudinal displacement of the tricuspid ring. Heart 96:281–288
Jurcut R, Giusca S, La Gerche A, Vasile S, Ginghina C, Voigt J-U (2010) The echocardiographic assessment of the right ventricle: what to do in 2010? Eur J Echocardiogr 11:81–96
Cacciapuoti F (2009) Echocardiographic evaluation of right heart function and pulmonary vascular bed. Int J Cardiovasc Imaging 25:689–697
van der Hulst AE, Roest AA, Delgado V et al (2011) Corrected tetralogy of Fallot: comparison of tissue Doppler imaging and velocity-encoded MR for assessment of performance and temporal activation of right ventricle. Radiology 260:88–97
Kutty S, Zhou J, Gauvreau K, Trincado C, Powell AJ, Geva T (2011) Regional dysfunction of the right ventricular outflow tract reduces the accuracy of Doppler tissue imaging assessment of global right ventricular systolic function in patients with repaired tetralogy of Fallot. J Am Soc Echocardiogr 24:637–643
Bonnemains L, Stos B, Vaugrenard T, Marie P-Y, Odille F, Boudjemline Y (2012) Echocardiographic right ventricle longitudinal contraction indices cannot predict ejection fraction in post-operative Fallot children. Eur Heart J Cardiovasc Imaging 13:235–242
Aebischer NM, Czegledy F (1989) Determination of right ventricular volume by two-dimensional echocardiography with a crescentic model. J Am Soc Echocardiogr 2:110–118
Alfakih K, Reid S, Jones T, Sivananthan M (2004) Assessment of ventricular function and mass by cardiac magnetic resonance imaging. Eur Radiol 14:1813–1822
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Buechel EV, Kaiser T, Jackson C, Schmitz A, Kellenberger CJ (2009) Normal right- and left ventricular volumes and myocardial mass in children measured by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson 11:19
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Reddington AN (2006) Physiopathology of right ventricular failure. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 3–10
Jensen CJ, Wolf A, Eberle HC et al (2011) Accuracy and variability of right ventricular volumes and mass assessed by dual-source computed tomography: influence of slice orientation in comparison to magnetic resonance imaging. Eur Radiol 21:2492–2502
Maffei E, Messalli G, Martini C et al (2012) Left and right ventricle assessment with cardiac CT: validation study vs. cardiac MR. Eur Radiol 22:1041–1049
Jiang L, Levine RA, Weyman AE (1997) Echocardiographic assessment of right ventricular volume and function. Echocardiography 14:189–206
Graham TP Jr, Jarmakani JM, Atwood GF, Canent RV Jr (1973) Right ventricular volume determinations in children. Normal values and observations with volume or pressure overload. Circulation 47:144–153
Shimazaki Y, Kawashima Y, Mori T, Beppu S, Yokota K (1980) Angiographic volume estimation of right ventricle. Re-evaluation of the previous methods. Chest 77:390–395
Czegledy F, Aebischer N, Smith D, Katz J (1993) A mathematical model of the right ventricular muscle geometry and mass. J Biomed Eng 15:127–131
di Cesare E (2003) MRI assessment of right ventricular dysplasia. Eur Radiol 13:1387–1393
Acknowledgements
The authors acknowledge the help of the Région Lorraine, the Communauté Urbaine du Grand Nancy and the FEDER European program.
The subjects from group A (60 persons) were already reported in another article concerning another question: Bonnemains L, Mandry D, Marie PY, Micard E, Chen B, Vuissoz PA (2012) Assessment of right ventricle volumes and function by cardiac MRI: quantification of the regional and global interobserver variability. Magn Reson Med 67:1740–6. Group A was just used to tune our parameters and we verified our hypothesis within group B (340 persons prospectively included and never reported until now).
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
The RV volume has often been approximated by area–length methods [13, 21–24]. These methods postulate that there is a proportional ratio (usually close to two thirds) among RV volume, its length (L) and its basal shortaxis area (A).
Let X d and X s be the value of X (X being one of the variables V, L or A) in end-diastole and in end-systole.
By definition,
However, the area–length models are based on the hypothesis of isotropic contraction: The shape of the ventricle is not modified by the contraction, only its size is. It has been proven that this hypothesis is not verified and many studies have shown the existence of a longitudinal contraction gradient from the basal segments (which contract less) to the apical segments (which contract more).
We applied the calculus presented above to a more complex model proposed in 1989 by Aebischer and Czegledy [13] called the crescentic shell model and introduced the notion of a contraction gradient from base to apex. This led to the introduction of a correction factor α in the longitudinal member of the formula with α slightly greater than 1:
Rights and permissions
About this article
Cite this article
Bonnemains, L., Mandry, D., Menini, A. et al. Surface–length index: a novel index for rapid detection of right ventricles with abnormal ejection fraction using cardiac MRI. Eur Radiol 23, 2383–2391 (2013). https://doi.org/10.1007/s00330-013-2851-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2851-9