Abstract
Purpose of Review
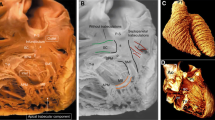
Review three-dimensional echocardiographic (3DE) acquisition and analysis of the right ventricular (RV) chamber, the recommended technique by the American Society of Echocardiography guidelines.
Recent Findings
3DE acquisition and analysis of RV size and function is available in the majority of clinical echocardiographic laboratories. Recent publications showed this approach provides accurate information despite the challenging chamber anatomy and physiology, when compared to magnetic resonance imaging as reference. 3DE assessment directly measures RV volumes without geometric assumptions. Accordingly, 3DE analysis was found more accurate and reproducible than conventional 2DE methodology, which measures only surrogate parameters of RV function.
Summary
RV 3DE assessment is ready for routine clinical use and has direct implications for patient management. 3DE evaluation has the potential to expand the analysis not only to traditionally parameters of size and function, but to new indices including shape, which may become a new useful diagnostic and prognostic information.







Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Cohen MS, Jegatheeswaran A, Baffa JM, Gremmels DB, Overman DM, Caldarone CA, et al. Echocardiographic features defining right dominant unbalanced atrioventricular septal defect: a multi-institutional Congenital Heart Surgeons’ Society study. Circ Cardiovasc Imaging. 2013;6(4):508–13. https://doi.org/10.1161/CIRCIMAGING.112.000189.
Cohen S, Gaddam S, Gemignani A, Wu WC, Sharma S, Choudhary G. Right ventricular function relates to functional capacity in men with atrial fibrillation and preserved left ventricular ejection fraction. Echocardiography. 2013;30(5):542–50. https://doi.org/10.1111/echo.12099.
Damy T, Ghio S, Rigby AS, Hittinger L, Jacobs S, Leyva F, et al. Interplay between right ventricular function and cardiac resynchronization therapy: an analysis of the CARE-HF trial (Cardiac Resynchronization-Heart Failure). J Am Coll Cardiol. 2013;61(21):2153–60. https://doi.org/10.1016/j.jacc.2013.02.049.
Finocchiaro G, Knowles JW, Pavlovic A, Perez M, Magavern E, Sinagra G, et al. Prevalence and clinical correlates of right ventricular dysfunction in patients with hypertrophic cardiomyopathy. Am J Cardiol. 2014;113(2):361–7. https://doi.org/10.1016/j.amjcard.2013.09.045.
Guazzi M, Bandera F, Pelissero G, Castelvecchio S, Menicanti L, Ghio S, et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol. 2013;305(9):H1373–81. https://doi.org/10.1152/ajpheart.00157.2013.
Hasan BS, Lunze FI, Chen MH, Brown DW, Boudreau MJ, Rhodes J, et al. Effects of transcatheter pulmonary valve replacement on the hemodynamic and ventricular response to exercise in patients with obstructed right ventricle-to-pulmonary artery conduits. JACC Cardiovasc Interv. 2014;7(5):530–42. https://doi.org/10.1016/j.jcin.2014.02.006.
Leong DP, Hoke U, Delgado V, Auger D, Witkowski T, Thijssen J, et al. Right ventricular function and survival following cardiac resynchronisation therapy. Heart. 2013;99(10):722–8. https://doi.org/10.1136/heartjnl-2012-303076.
Poliacikova P, Cockburn J, Pareek N, James R, Lee L, Trivedi U, et al. Prognostic impact of pre-existing right ventricular dysfunction on the outcome of transcatheter aortic valve implantation. J Invasive Cardiol. 2013;25(3):142–5.
Pruszczyk P, Goliszek S, Lichodziejewska B, Kostrubiec M, Ciurzynski M, Kurnicka K, et al. Prognostic value of echocardiography in normotensive patients with acute pulmonary embolism. JACC Cardiovasc Imaging. 2014;7(6):553–60. https://doi.org/10.1016/j.jcmg.2013.11.004.
Saguner AM, Vecchiati A, Baldinger SH, Rueger S, Medeiros-Domingo A, Mueller-Burri AS, et al. Different prognostic value of functional right ventricular parameters in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circ Cardiovasc Imaging. 2014;7(2):230–9. https://doi.org/10.1161/CIRCIMAGING.113.000210.
Said SM, Dearani JA, Burkhart HM, Connolly HM, Eidem B, Stensrud PE, et al. Management of tricuspid regurgitation in congenital heart disease: is survival better with valve repair? J Thorac Cardiovasc Surg. 2014;147(1):412–7. https://doi.org/10.1016/j.jtcvs.2013.08.034.
Schuuring MJ, van Gulik EC, Koolbergen DR, Hazekamp MG, Lagrand WK, Backx AP, et al. Determinants of clinical right ventricular failure after congenital heart surgery in adults. J Cardiothorac Vasc Anesth. 2013;27(4):723–7. https://doi.org/10.1053/j.jvca.2012.10.022.
Schuuring MJ, van Riel AC, Vis JC, Duffels MG, van Dijk AP, de Bruin-Bon RH, et al. New predictors of mortality in adults with congenital heart disease and pulmonary hypertension: midterm outcome of a prospective study. Int J Cardiol. 2015;181:270–6. https://doi.org/10.1016/j.ijcard.2014.11.222.
Wald RM, Altaha MA, Alvarez N, Caldarone CA, Cavalle-Garrido T, Dallaire F, et al. Rationale and design of the Canadian Outcomes Registry Late After Tetralogy of Fallot Repair: the CORRELATE study. Can J Cardiol. 2014;30(11):1436–43. https://doi.org/10.1016/j.cjca.2014.06.011.
Mertens LL, Friedberg MK. Imaging the right ventricle—current state of the art. Nat Rev Cardiol. 2010;7(10):551–63. https://doi.org/10.1038/nrcardio.2010.118.
• Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713; quiz 86–8. doi:https://doi.org/10.1016/j.echo.2010.05.010. Right ventricular echocardiographic guidelines.
• Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39 e14. https://doi.org/10.1016/j.echo.2014.10.003. Updated cardiac chamber quantification guidelines.
Bleeker GB, Steendijk P, Holman ER, Yu CM, Breithardt OA, Kaandorp TA, et al. Assessing right ventricular function: the role of echocardiography and complementary technologies. Heart. 2006;92(Suppl 1):i19–26. https://doi.org/10.1136/hrt.2005.082503.
Ling LF, Obuchowski NA, Rodriguez L, Popovic Z, Kwon D, Marwick TH. Accuracy and interobserver concordance of echocardiographic assessment of right ventricular size and systolic function: a quality control exercise. J Am Soc Echocardiogr. 2012;25(7):709–13. https://doi.org/10.1016/j.echo.2012.03.018.
Jenkins C, Chan J, Bricknell K, Strudwick M, Marwick TH. Reproducibility of right ventricular volumes and ejection fraction using real-time three-dimensional echocardiography: comparison with cardiac MRI. Chest. 2007;131(6):1844–51. https://doi.org/10.1378/chest.06-2143.
Leibundgut G, Rohner A, Grize L, Bernheim A, Kessel-Schaefer A, Bremerich J, et al. Dynamic assessment of right ventricular volumes and function by real-time three-dimensional echocardiography: a comparison study with magnetic resonance imaging in 100 adult patients. J Am Soc Echocardiogr. 2010;23(2):116–26. https://doi.org/10.1016/j.echo.2009.11.016.
Nesser HJ, Tkalec W, Patel AR, Masani ND, Niel J, Markt B, et al. Quantitation of right ventricular volumes and ejection fraction by three-dimensional echocardiography in patients: comparison with magnetic resonance imaging and radionuclide ventriculography. Echocardiography. 2006;23(8):666–80. https://doi.org/10.1111/j.1540-8175.2006.00286.x.
Niemann PS, Pinho L, Balbach T, Galuschky C, Blankenhagen M, Silberbach M, et al. Anatomically oriented right ventricular volume measurements with dynamic three-dimensional echocardiography validated by 3-Tesla magnetic resonance imaging. J Am Coll Cardiol. 2007;50(17):1668–76. https://doi.org/10.1016/j.jacc.2007.07.031.
Sugeng L, Mor-Avi V, Weinert L, Niel J, Ebner C, Steringer-Mascherbauer R, et al. Multimodality comparison of quantitative volumetric analysis of the right ventricle. JACC Cardiovasc Imaging. 2010;3(1):10–8. https://doi.org/10.1016/j.jcmg.2009.09.017.
van der Zwaan HB, Geleijnse ML, McGhie JS, Boersma E, Helbing WA, Meijboom FJ, et al. Right ventricular quantification in clinical practice: two-dimensional vs. three-dimensional echocardiography compared with cardiac magnetic resonance imaging. Eur J Echocardiogr. 2011;12(9):656–64. https://doi.org/10.1093/ejechocard/jer107.
Tosoratti E, Badano LP, Gianfagna P, Baldassi M, Proclemer A, Capelli C, et al. Improved delineation of morphological features of arrhythmogenic right ventricular cardiomyopathy with the use of contrast-enhanced echocardiography. J Cardiovasc Med (Hagerstown). 2006;7(7):566–8. https://doi.org/10.2459/01.JCM.0000234777.03949.10.
Ota T, Fleishman CE, Strub M, Stetten G, Ohazama CJ, von Ramm OT, et al. Real-time, three-dimensional echocardiography: feasibility of dynamic right ventricular volume measurement with saline contrast. Am Heart J. 1999;137(5):958–66.
Kaminska M, Sobkowicz B, Sawicki R, Lewkowicz J, Tomaszuk-Kazberuk A, Glinska R, et al. Is real time contrast echocardiography useful for assessment of the right ventricular morphology, function, and perfusion? Echocardiography. 2015;32(7):1080–6. https://doi.org/10.1111/echo.12819.
• Medvedofsky D, Mor-Avi V, Kruse E, Guile B, Ciszek B, Weinert L, et al. Quantification of right ventricular size and function from contrast-enhanced three-dimensional echocardiographic images. J Am Soc Echocardiogr. 2017;30(12):1193–202. https://doi.org/10.1016/j.echo.2017.08.003. Three-dimensional echocardiographic validation study using contrast anhancing agents.
Kim J, Cohen SB, Atalay MK, Maslow AD, Poppas A. Quantitative assessment of right ventricular volumes and ejection fraction in patients with left ventricular systolic dysfunction by real time three-dimensional echocardiography versus cardiac magnetic resonance imaging. Echocardiography. 2015;32(5):805–12. https://doi.org/10.1111/echo.12715.
Seguela PE, Hascoet S, Brierre G, Bongard V, Acar P. Feasibility of three-dimensional transthoracic echocardiography to evaluate right ventricular volumes in children and comparison to left ventricular values. Echocardiography. 2012;29(4):492–501. https://doi.org/10.1111/j.1540-8175.2011.01596.x.
. Medvedofsky D, Addetia K, Patel AR, Sedlmeier A, Baumann R, Mor-Avi V, et al. Novel approach to three-dimensional echocardiographic quantification of right ventricular volumes and function from focused views. J Am Soc Echocardiogr. 2015;28(10):1222–31. https://doi.org/10.1016/j.echo.2015.06.013. Three-dimensional echocardiographic validation study vs cardiac magnetic resonance imaging.
• Muraru D, Spadotto V, Cecchetto A, Romeo G, Aruta P, Ermacora D, et al. New speckle-tracking algorithm for right ventricular volume analysis from three-dimensional echocardiographic data sets: validation with cardiac magnetic resonance and comparison with the previous analysis tool. Eur Heart J Cardiovasc Imaging. 2016;17(11):1279–89. https://doi.org/10.1093/ehjci/jev309. Three-dimensional echocardiographic validation study vs cardiac magnetic resonance imaging.
Taylor AQ, Messner AA. Algorithm 550, solid polyhedron measures. ACM Trans Math Softw. 1980;6:121–30.
Mor-Avi V, Jenkins C, Kuhl HP, Nesser HJ, Marwick T, Franke A, et al. Real-time 3-dimensional echocardiographic quantification of left ventricular volumes: multicenter study for validation with magnetic resonance imaging and investigation of sources of error. JACC Cardiovasc Imaging. 2008;1(4):413–23. https://doi.org/10.1016/j.jcmg.2008.02.009.
Addetia K, Maffessanti F, Yamat M, Weinert L, Narang A, Freed BH, et al. Three-dimensional echocardiography-based analysis of right ventricular shape in pulmonary arterial hypertension. Eur Heart J Cardiovasc Imaging. 2016;17(5):564–75. https://doi.org/10.1093/ehjci/jev171.
• Addetia K, Uriel N, Maffessanti F, Sayer G, Adatya S, Kim GH, et al. 3D morphological changes in LV and RV during LVAD ramp studies. JACC Cardiovasc Imaging. 2018;11(2 Pt 1):159–69. https://doi.org/10.1016/j.jcmg.2016.12.019. Three-dimensional echocardiographic shape analysis of the left and right ventricles in LVADs patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
There are no issues related to this article that could be construed as a violation of ethical standards.
Conflict of Interest
Eric Kruse reports personal fees from Lantheus Medical Imaging outside of the submitted work. Roberto Lang reports grants from Philips and TOMTEC, outside of the submitted work. The other authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Echocardiography
Electronic Supplementary Material
2DE RV focused 4-chamber view. From a 2DE apical conventional 4-chamber view, the RV focused 4-chamber view is obtained by modifying the position of the transducer more laterally, and its angle more anterior. (MP4 2917 kb)
Video 2
Right ventricular (RV)-focused 3DE dataset acquisition with simultaneous real-time short-axis and long-axis multiplanar reconstruction. An effort should be done to include the entire RV free wall for a more accurate analysis. (WMV 1272 kb)
Top: an example of a good quality 3D RV dataset without contrast (left), in which endocardial border definition further improved with contrast enhancement (right). Bottom: an example of a suboptimal quality 3D RV dataset, in which the endocardial border is poorly visualized without contrast (left), but was considerably improved by contrast enhancement (right), specially for the RV free wall anterior and lateral segments. (MP4 2208 kb)
Video 4
Combined video (left), end-diastolic (center) and end-systolic (right) views, in short-and long-axis views of the right ventricle used to fine tune endocardial border detection. The long-axis image plane can be changed (dotted yellow line in the short-axis views) to assess correct tracing along the right ventricular surface. (WMV 4811 kb)
Two right ventricular generated beating models with a fixed end-diastolic mesh, without (left) and with (right) a 2-dimensional background. (MP4 1360 kb)
Video 6
Similar endocardial border analyses as explained in Video 4, but with contrast enhancement. Imaging of the right ventricle is feasible and results in visible improvement in the definition of the free wall segments in patients with suboptimal visualization without contrast. One difference is that with contrast, the RVOT is considerably better visualized. (WMV 4269 kb)
Video 7
3D fully automatic, dynamic volumetric analysis is one of the next steps for 3D RV analysis. (MOV 625 kb)
Rights and permissions
About this article
Cite this article
Medvedofsky, D., Kruse, E., Mor-Avi, V. et al. Three-Dimensional Echocardiography for Evaluation of the Right Ventricle—Updates on Image Acquisition and Analysis. Curr Cardiovasc Imaging Rep 11, 18 (2018). https://doi.org/10.1007/s12410-018-9460-6
Published:
DOI: https://doi.org/10.1007/s12410-018-9460-6