Abstract
Background
We evaluated the ability of transthoracic echocardiography (TTE) to correctly identify abnormal left ventricular (LV) size, function, and mass when compared to cardiac magnetic resonance (CMR). Whilst numerous studies have compared TTE and CMR with respect to correlation between measurements and study reproducibility, few have employed categorical analysis relevant to clinical practice.
Methods
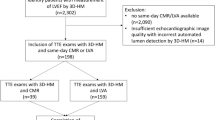
Two hundred and fifteen consecutive patients who underwent both TTE and CMR were evaluated for the presence of abnormal LV size, systolic function, and mass. Abnormal LV systolic function was further categorized into grades (mild, moderate, and severe). Quantification of LV morphology and function was performed on TTE and CMR according to published guidelines. The level of agreement between TTE and CMR was compared across binary and categorical variables using Cohen’s kappa.
Results
Compared to CMR, TTE demonstrated excellent agreement in identification of abnormal versus normal function (κ = 0.87). However, agreement across grades of LV function was less strong (κ = 0.63). Whilst agreement for identification of severe LV dysfunction was good (κ = 0.68), this would still lead to misclassification of severe dysfunction in approximately one in seven cases. Agreement between TTE and CMR was moderate to good for identification of LV dilation (κ = 0.43–0.63), but poor for identification of increased mass (κ = 0.04).
Conclusions
Whilst in clinical practice TTE performs well in identification of normal versus abnormal systolic function, it has substantial limitations across grades of dysfunction and in the assessment of LV size and mass. These limitations have important implications when considering management decisions for patients based on thresholds of LV morphology or function.






Similar content being viewed by others
Abbreviations
- 2DE:
-
Two-dimensional echocardiography
- 3DE:
-
Three-dimensional echocardiography
- ACEI:
-
Angiotensin-converting enzyme inhibitors
- BMI:
-
Body mass index
- BSA:
-
Body surface area
- CMR:
-
Cardiac magnetic resonance
- EDV:
-
End-diastolic volume
- EF:
-
Ejection fraction
- ICD:
-
Implantable cardioverter-defibrillator
- LV:
-
Left ventricular
- LVEDD:
-
Left ventricular end-diastolic diameter
- TTE:
-
Transthoracic echocardiography
References
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail. 2008;10(10):933–89.
Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012). The Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). G Ital Cardiol (Rome). 2013;14(3):167–214.
Wood PW, Choy JB, Nanda NC, Becher H. Left ventricular ejection fraction and volumes: it depends on the imaging method. Echocardiography. 2014;31(1):87–100.
Alfakih K, Bloomer T, Bainbridge S, et al. A comparison of left ventricular mass between two-dimensional echocardiography, using fundamental and tissue harmonic imaging, and cardiac MRI in patients with hypertension. Eur J Radiol. 2004;52(2):103–9.
Kirkpatrick JN, Vannan MA, Narula J, Lang RM. Echocardiography in heart failure: applications, utility, and new horizons. J Am Coll Cardiol. 2007;50(5):381–96.
Krum H, Driscoll A. Management of heart failure. Med J Aust. 2013;199(5):334–9.
Tracy CM, Epstein AE, Darbar D, et al. ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation. 2012;126(14):1784–800.
Hoffmann R, von Bardeleben S, ten Cate F, et al. Assessment of systolic left ventricular function: a multi-centre comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast-enhanced echocardiography. Eur Heart J. 2005;26(6):607–16.
Mor-Avi V, Sugeng L, Weinert L, et al. Fast measurement of left ventricular mass with real-time three-dimensional echocardiography: comparison with magnetic resonance imaging. Circulation. 2004;110(13):1814–8.
Jenkins C, Moir S, Chan J, et al. Left ventricular volume measurement with echocardiography: a comparison of left ventricular opacification, three-dimensional echocardiography, or both with magnetic resonance imaging. Eur Heart J. 2009;30(1):98–106.
Mistry N, Halvorsen S, Hoffmann P, et al. Assessment of left ventricular function with magnetic resonance imaging vs. echocardiography, contrast echocardiography, and single-photon emission computed tomography in patients with recent ST-elevation myocardial infarction. Eur J Echocardiogr. 2010;11(9):793–800.
(12) Gruszczynska K, Krzych LJ, Golba KS et al. Statistical agreement of left ventricle measurements using cardiac magnetic resonance and 2D echocardiography in ischemic heart failure. Med Sci Monit. 2012;18(3):MT19-25.
Van De Heyning CM, Magne J, Pierard LA, et al. Assessment of left ventricular volumes and primary mitral regurgitation severity by 2D echocardiography and cardiovascular magnetic resonance. Cardiovasc Ultrasound. 2013;11:46.
Thavendiranathan P, Liu S, Verhaert D, et al. Feasibility, accuracy, and reproducibility of real-time full-volume 3D transthoracic echocardiography to measure LV volumes and systolic function: a fully automated endocardial contouring algorithm in sinus rhythm and atrial fibrillation. J Am Coll Cardiol Imaging. 2012;5(3):239–51.
Macron L, Lim P, Bensaid A, et al. Single-beat versus multibeat real-time 3D echocardiography for assessing left ventricular volumes and ejection fraction: a comparison study with cardiac magnetic resonance. Circ Cardiovasc Imaging. 2010;3(4):450–5.
Missouris CG, Forbat SM, Singer DR, et al. Echocardiography overestimates left ventricular mass: a comparative study with magnetic resonance imaging in patients with hypertension. J Hypertens. 1996;14(8):1005–10.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18(12):1440–63.
Gandy SJ, Waugh SA, Nicholas RS, et al. Comparison of the reproducibility of quantitative cardiac left ventricular assessments in healthy volunteers using different MRI scanners: a multicenter simulation. J Magn Reson Imaging. 2008;28(2):359–65.
Natori S, Lai S, Finn JP, et al. Cardiovascular function in multi-ethnic study of atherosclerosis: normal values by age, sex, and ethnicity. AJR Am J Roentgenol. 2006;186(6 Suppl 2):S357–65.
Teichholz LE, Kreulen T, Herman MV, Gorlin R. Problems in echocardiographic volume determinations: echocardiographic–angiographic correlations in the presence of absence of asynergy. Am J Cardiol. 1976;37(1):7–11.
Hudsmith LE, Petersen SE, Francis JM, et al. Normal human left and right ventricular and left atrial dimensions using steady state free precession magnetic resonance imaging. J Cardiovasc Magn Reson. 2005;7(5):775–82.
Maceira AM, Prasad SK, Khan M, et al. Normalized left ventricular systolic and diastolic function by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2006;8(3):417–26.
Nishimura RA, Otto CM, Bonow RO, et al. AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(22):e57–185.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239.
Bellenger NG, Burgess MI, Ray SG, et al. Comparison of left ventricular ejection fraction and volumes in heart failure by echocardiography, radionuclide ventriculography and cardiovascular magnetic resonance; are they interchangeable? Eur Heart J. 2000;21(16):1387–96.
Bottini PB, Carr AA, Prisant LM, et al. Magnetic resonance imaging compared to echocardiography to assess left ventricular mass in the hypertensive patient. Am J Hypertens. 1995;8(3):221–8.
Kadish A, Dyer A, Daubert JP, et al. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350(21):2151–8.
Zannad F, McMurray JJ, Krum H, et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011;364(1):11–21.
Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341(10):709–17.
Gibson PH, Becher H, Choy JB. Classification of left ventricular size: diameter or volume with contrast echocardiography? Open Heart. 2014;1(1):e000147.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding to declare for all authors.
Conflict of interest
Authors Andrew Taylor, James Hare, Leah Iles, Andris Ellims and Benedict Costello have multiple affiliations as Cardiologists with Heart Centre, Alfred Hospital, Melbourne and involvement in research opportunities with Baker IDI Heart and Diabetes Institute. No funding was allocated to this research project. Andrew Taylor, James Hare, Benedict Costello, Leah Iles, Andris Ellims and Jeffrey Alexis declare no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
We conducted a retrospective study of de-identified data and therefore formal consent was not required.
Rights and permissions
About this article
Cite this article
Alexis, J.A., Costello, B., Iles, L.M. et al. Assessment of the accuracy of common clinical thresholds for cardiac morphology and function by transthoracic echocardiography. J Echocardiogr 15, 27–36 (2017). https://doi.org/10.1007/s12574-016-0322-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-016-0322-4