Abstract
Background
Although esophagectomy is the only curative option for esophageal cancer, the associated invasiveness is high. Nasogastric (NG) tube use may prevent complications; however, its utility remains unclear, and the decompression period depends on the doctor. This study aimed to reveal the effect of conventional versus early NG tube removal on postoperative complications after esophagectomy.
Methods
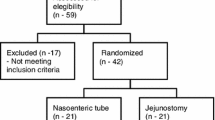
This single-center prospective randomized controlled clinical trial enrolled patients aged 20–80 years with histologically proven primary esophageal squamous cell carcinoma. Eighty patients admitted for transthoracic first-stage esophagectomy reconstructed with gastric conduit were randomly assigned (1:1) to the conventional and early NG tube removal groups. In the conventional NG tube removal group, the tube was removed on postoperative day (POD) 7; in the other, it was removed on POD 1. The occurrence rate of major complications, length of postoperative hospital stay, and NG tube reinsertion rate were compared between the groups.
Results
The incidence of postoperative major complications such as pneumonia, anastomotic leakage, recurrent nerve palsy and gastrointestinal bleeding, and the NG tube reinsertion rate was not different between the groups. However, recurrent nerve palsy was more commonly observed in the conventional removal group; this difference was not significant. In terms of postoperative pneumonia, tumor location and field of lymph node dissection were significant risk factors.
Conclusion
Although early NG tube removal did not reduce the rate of postoperative pneumonia, it could be performed safely. Hence, the NG tube can be removed earlier than conventional methods.

Similar content being viewed by others
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Griffin SM, Shaw IH, Dresner SM (2002) Early complications after Ivor Lewis subtotal esophagectomy with two-field lymphadenectomy: risk factors and management. J Am Coll Surg 194:285–297
Ando N, Ozawa S, Kitagawa Y, Shinozawa Y, Kitajima M (2000) Improvement in the results of surgical treatment of advanced squamous esophageal carcinoma during 15 consecutive years. Ann Surg 232:225–232
Whooley BP, Law S, Murthy SC, Alexandrou A, Wong J (2001) Analysis of reduced death and complication rates after esophageal resection. Ann Surg 233:338–344
Sato T, Takayama T, So K, Murayama I (2007) Is retention of a nasogastric tube after esophagectomy a risk factor for postoperative respiratory tract infection? J Infect Chemother 13:109–113
Nguyen NT, Slone J, Wooldridge J, Smith BR, Reavis KM, Hoyt D (2009) Minimally invasive esophagectomy without the use of postoperative nasogastric tube decompression. Am Surg 75:929–931
Daryaei P, Vaghef Davari F, Mir M, Harirchi I, Salmasian H (2009) Omission of nasogastric tube application in postoperative care of esophagectomy. World J Surg 33:773–777. https://doi.org/10.1007/s00268-009-9930-8
Shackcloth MJ, McCarron E, Kendall J, Russell GN, Pennefather SH, Tran J, Page RD (2006) Randomized clinical trial to determine the effect of nasogastric drainage on tracheal acid aspiration following oesophagectomy. Br J Surg 93:547–552
Mistry RC, Vijayabhaskar R, Karimundackal G, Jiwnani S, Pramesh CS (2012) Effect of short-term vs prolonged nasogastric decompression on major postesophagectomy complications: a parallel-group, randomized trial. Arch Surg 147:747–751
Kaburagi T, Takeuchi H, Kawakubo H, Omori T, Ozawa S, Kitagawa Y (2014) Clinical utility of a novel hybrid position combining the left lateral decubitus and prone positions during thoracoscopic esophagectomy. World J Surg 38:410–418. https://doi.org/10.1007/s00268-013-2258-4
Katayama H, Kurokawa Y, Nakamura K et al (2016) Extended Clavien-Dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today 46:668–685
Lee JH, Hyung WJ, Noh SH (2002) Comparison of gastric cancer surgery with versus without nasogastric decompression. Yonsei Med J 43:451–456
Rao W, Zhang X, Zhang J, Yan R, Hu Z, Wang Q (2011) The role of nasogastric tube in decompression after elective colon and rectum surgery: a meta-analysis. Int J Colorectal Dis 26:423–429
Nelson R, Edwards S, Tse B (2007) Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev 3:CD004929
Weijs TJ, Kumagai K, Berkelmans GH, Nieuwenhuijzen GA, Nilsson M, Luyer MD (2017) Nasogastric decompression following esophagectomy: a systematic literature review and meta-analysis. Dis Esophagus 30:1–8
Ichida H, Imamura H, Yoshimoto J, Sugo H, Ishizaki Y, Kawasaki S (2016) Randomized controlled trial for evaluation of the routine use of nasogastric tube decompression after elective liver surgery. J Gastrointest Surg 20:1324–1330
Shiozaki A, Fujiwara H, Okamura H et al (2012) Risk factors for postoperative respiratory complications following esophageal cancer resection. Oncol Lett 3:907–912
Takeuchi H, Miyata H, Ozawa S et al (2017) Comparison of short-term outcomes between open and minimally invasive esophagectomy for esophageal cancer using a nationwide database in Japan. Ann Surg Oncol 24:1821–1827
Acknowledgements
The authors thank Kumiko Motooka, who belongs to the staff at the Department of Surgery in Keio University School of Medicine, for her help in the preparation of this report.
Funding
This study was funded by Takeda Pharmaceutical Company Limited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayashi, M., Kawakubo, H., Shoji, Y. et al. Analysis of the Effect of Early Versus Conventional Nasogastric Tube Removal on Postoperative Complications After Transthoracic Esophagectomy: A Single-Center, Randomized Controlled Trial. World J Surg 43, 580–589 (2019). https://doi.org/10.1007/s00268-018-4825-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4825-1