Abstract
Background
The value of routine nasogastric tube (NGT) decompression after elective hepatetctomy is not yet established. Previous studies in the setting of non-liver abdominal surgery suggested that the use of NGT decreased the incidence of nausea or vomiting, while increasing the frequency of pulmonary complications.
Study Design
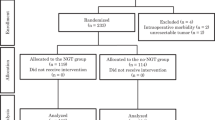
Out of a total of 284 consecutive patients undergoing hepatectomy, 210 patients were included in this study. The patients were randomized to a group that received NGT decompression (NGT group; n = 108), in which a NGT was left in place after surgery until the patient passed flatus or stool, or a group that did not receive NGT decompression (no-NGT group; n = 102), in which the NGT was removed at the end of surgery.
Results
There were no differences between the NGT group and no-NGT group in terms of the overall morbidity (34.3 vs 35.3 %; P = 0.99), incidence of pulmonary complications (18.5 vs 19.5 %; P = 0.84), frequency of postoperative vomiting (6.5 vs 7.8 %; P = 0.70), time to start of oral intake (median (range) 3 (2–6) vs 3 (2–6) days; P = 0.69), or postoperative duration of hospital stay (19 (7–74) vs 18 (9–186) days; P = 0.37). In the no-NGT group, three patients required reinsertion of the tube 0 (0–3) days after surgery. In the NGT group, severe discomfort was recorded in five patients.
Conclusions
Routine NGT decompression after elective hepatectomy does not appear to have any advantages.

Similar content being viewed by others
References
Levin AL. A new gastroduodenal catheter. JAMA 1921; 76: 1007.
Nathan BN, Pain JA. Nasogastric suction after elective abdominal surgery: a randomised study. Annals of the Royal College of Surgeons of England 1991; 73: 291–294.
Feo CV, Romanini B, Sortini D, et al. Early oral feeding after colorectal resection: a randomized controlled study. ANZ journal of surgery 2004; 74: 298–301.
Verma R, Nelson RL. Prophylactic nasogastric decompression after abdominal surgery. The Cochrane database of systematic reviews, CD004929 (2010).
Vermeulen H, Storm-Versloot MN, Busch OR, et al. Nasogastric intubation after abdominal surgery: a meta-analysis of recent literature. Archives of surgery (Chicago, Ill: 1960) 2006; 141: 307–314.
Carrere N, Seulin P, Julio CH, et al. Is nasogastric or nasojejunal decompression necessary after gastrectomy? A prospective randomized trial. World journal of surgery 2007; 31: 122–127.
Savassi-Rocha PR, Conceicao SA, Ferreira JT, et al. Evaluation of the routine use of the nasogastric tube in digestive operation by a prospective controlled study. Surgery, gynecology & obstetrics 1992; 174: 317–320.
Petrelli NJ, Stulc JP, Rodriguez-Bigas M, et al. Nasogastric decompression following elective colorectal surgery: a prospective randomized study. The American surgeon 1993; 59: 632–635.
Cheatham ML, Chapman WC, Key SP, et al. A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Annals of surgery 1995; 221: 469–476; discussion 476–468.
Choi YY, Kim J, Seo D, et al. Is routine nasogastric tube insertion necessary in pancreaticoduodenectomy? Journal of the Korean Surgical Society 2011; 81: 257–262.
Rao W, Zhang X, Zhang J, et al. The role of nasogastric tube in decompression after elective colon and rectum surgery: a meta-analysis. International journal of colorectal disease 2011; 26: 423–429.
Pessaux P, Regimbeau JM, Dondero F, et al. Randomized clinical trial evaluating the need for routine nasogastric decompression after elective hepatic resection. The British journal of surgery 2007; 94: 297–303.
Ephgrave KS, Kleiman-Wexler R, Pfaller M, et al. Postoperative pneumonia: a prospective study of risk factors and morbidity. Surgery 1993; 114: 815–819; discussion 819–821.
Friedman M, Baim H, Shelton V, et al. Laryngeal injuries secondary to nasogastric tubes. The Annals of otology, rhinology, and laryngology 1981; 90: 469–474.
Manning BJ, Winter DC, McGreal G, et al. Nasogastric intubation causes gastroesophageal reflux in patients undergoing elective laparotomy. Surgery 2001; 130: 788–791.
Taylor FW. Electrolyte loss by postoperative nasal-gastric suction. AMA archives of surgery 1953; 66: 538–544.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the institutional review board of Juntendo University Hospital. Written informed consent was obtained from all the patients participating in the study.
Rights and permissions
About this article
Cite this article
Ichida, H., Imamura, H., Yoshimoto, J. et al. Randomized Controlled Trial for Evaluation of the Routine Use of Nasogastric Tube Decompression After Elective Liver Surgery. J Gastrointest Surg 20, 1324–1330 (2016). https://doi.org/10.1007/s11605-016-3116-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3116-0