Abstract
Background
Anastomotic configurations may be a predictor of postoperative recurrence for Crohn’s disease. One previous meta-analysis showed side-to-side anastomosis was associated with fewer anastomotic leaks but did not reduce postoperative recurrence rates. After 2007, more articles that found distinct results were published. We aimed to update the meta-analysis comparing outcomes between side-to-side anastomosis and other anastomotic configurations after intestinal resection for patients with Crohn’s disease.
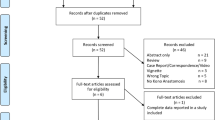
Methods
A literature search that included PubMed, EMBASE, the Science Citation Index, and the Cochrane Library was conducted to identify studies up to May 2012. Trials comparing side-to-side anastomosis with other anastomotic configurations for Crohn’s disease were analyzed. Sensitivity analysis and heterogeneity assessment were also performed.
Results
Eleven trials compared side-to-side with other anastomotic configurations were included. Overall, results showed a significant reduction in the overall postoperative complications [n = 777; odds ratio (OR) = 0.60; P = 0.01], but side-to-side anastomosis did not reduce the anastomotic leak rate (n = 879; OR = 0.48; P = 0.07), complications other than anastomotic leak (n = 777; OR = 0.72; P = 0.13), endoscopic recurrence rates [hazard ratio (HR) = 0.73; P = 0.07], symptomatic recurrence rates (HR = 0.74; P = 0.20), and reoperation rates for recurrence (HR = 0.37; P = 0.06). Sensitivity analysis including two randomized controlled trials found no significant differences in short-term complications between the two groups. Sensitivity analysis including nine trials comparing only stapled side-to-side anastomosis with other anastomotic configurations showed stapled side-to-side anastomosis could reduce reoperation rates (HR = 0.38; P = 0.01).
Conclusions
Side-to-side anastomosis did not reduce short-term complications and postoperative recurrence for Crohn’s disease. Stapled side-to-side anastomosis may lead to fewer reoperations needed for recurrence. Further randomized, controlled trials should be conducted for confirmation of recurrent events.





Similar content being viewed by others
References
Khor B, Gardet A, Xavier RJ (2011) Genetics and pathogenesis of inflammatory bowel disease. Nature 474:307–317
Olaison G, Sjodahl R, Tagesson C (1990) Glucocorticoid treatment in ileal Crohn’s disease: relief of symptoms but not of endoscopically viewed inflammation. Gut 31:325–328
Buisson A, Chevaux JB, Allen PB et al (2012) Review article: the natural history of postoperative Crohn’s disease recurrence. Aliment Pharmacol Ther 35:625–633
De Cruz P, Kamm MA, Prideaux L et al (2012) Postoperative recurrent luminal Crohn’s disease: a systematic review. Inflamm Bowel Dis 18:758–777
Yamamoto T (2005) Factors affecting recurrence after surgery for Crohn’s disease. World J Gastroenterol 11:3971–3979
Reese GE, Nanidis T, Borysiewicz C et al (2008) The effect of smoking after surgery for Crohn’s disease: a meta-analysis of observational studies. Int J Colorectal Dis 23:1213–1221
Simillis C, Yamamoto T, Reese GE et al (2008) A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn’s disease. Am J Gastroenterol 103:196–205
Cameron JL, Hamilton SR, Coleman J et al (1992) Patterns of ileal recurrence in Crohn’s disease. Ann Surg 215:546–552
Caprilli R, Corrao G, Taddei G et al (1996) Prognostic factors for postoperative recurrence of Crohn’s disease. Dis Colon Rectum 39:335–341
Bordeianou L, Dursun A (2010) Current thinking on recurrence: does anastomotic surgical technique affect recurrence rates in Crohn’s patients? Inflamm Bowel Dis 16:539–540
Post S, Betzler M, von Ditfurth B et al (1991) Risks of intestinal anastomoses in Crohn’s disease. Ann Surg 213:37–42
Simillis C, Purkayastha S, Yamamoto T et al (2007) A meta-analysis comparing conventional end-to-end anastomosis vs. other anastomotic configurations after resection in Crohn’s disease. Dis Colon Rectum 50:1674–1687
Scarpa M, Ruffolo C, Bertin E et al (2007) Surgical predictors of recurrence of Crohn’s disease after ileocolonic resection. Int J Colorectal Dis 22:1061–1069
McLeod RS, Wolff BG, Ross S et al (2009) Recurrence of Crohn’s disease after ileocolic resection is not affected by anastomotic type: results of a multicenter, randomized, controlled trial. Dis Colon Rectum 52:919–927
Zhu WM, Li Y, Yu C et al (2011) Impact of anastomosis type on postoperative recurrence after bowel resection for Crohn’s disease. Zhonghua Wei Chang Wai Ke Za Zhi 14:168–170
Zurbuchen U, Kroesen AJ, Knebel P et al. (2012) Complications after end-to-end vs. side-to-side anastomosis in ileocecal Crohn’s disease—early postoperative results from a randomized controlled multi-center trial (ISRCTN-45665492). Langenbecks Arch Surg. doi:10.1007/s00423-012-0904-1
Li Y, Zhu W, Zuo L et al (2012) Frequency and risk factors of postoperative recurrence of Crohn’s disease after intestinal resection in the Chinese population. J Gastrointest Surg 16:1539–1547
Wells GA, Shea B, O’Connell D et al. (2000) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. In: Paper presented at 3rd symposium on systematic reviews: beyond the basics. Oxford. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 17 Jan 2013
Moher D, Pham B, Jones A et al (1998) Does quality of reports of randomized trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 352:609–613
Higgins JPT, Altman DG (2008) Assessing risk of bias in included studies, chap 8. In: Higgins J, Green S (eds) Cochrane handbook for systematic reviews of interventions, version 5.0.0 (updated Feb 2008), The Cochrane Collaboration. Wiley, Chichester
Tierney JF, Stewart LA, Ghersi D et al (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Kusunoki M, Ikeuchi H, Yanagi H et al (1998) A comparison of stapled and hand-sewn anastomoses in Crohn’s disease. Dig Surg 15:679–682
Ikeuchi H, Kusunoki M, Yamamura T (2000) Long-term results of stapled and hand-sewn anastomoses in patients with Crohn’s disease. Dig Surg 17:493–496
Cameron JL, Hamilton SR, Coleman J et al (1992) Patterns of ileal recurrence in Crohn’s disease. A prospective randomized study. Ann Surg 215:546–551
Funayama Y, Fukushima K, Shibata C et al (2006) Early postoperative results of novel procedure of side-to-side isoperistaltic ileocolonic anastomosis for Crohn’s disease—randomized controlled trial. Gastroenterology 1302:A866–A867
Moskovitz D, McLeod RS, Greenberg GR et al (1999) Operative and environmental risk factors for recurrence of Crohn’s disease. Int J Colorectal Dis 14:224–226
Kwok KHK, Rodwell L, Young JM et al (2011) The effect of anastomotic technique on surgical recurrence rates in Crohn’s disease—a NSW data linkage study. Colorectal Dis 13:62
Frieri G, Pimpo MT, Palumbo G et al (2000) Anastomotic configuration and mucosal 5-aminosalicyclic acid (5-ASA) concentrations in patients with Crohn’s disease: a GISC study. Gruppo Italiano per lo Studio del Colon e del Retto. Am J Gastroenterol 95:1486–1490
Yamamoto T, Allan RN, Keighley MR (1999) Strategy for surgical management of ileocolonic anastomotic recurrence in Crohn’s disease. World J Surg 23:1055–1060. doi:10.1007/s002689900623
Yamamoto T, Bain IM, Allan RN et al (1998) Side-to-side stapled versus end-to-end sutured anastomosis following ileocolonic resection for Crohn’s disease: complications and early recurrence rates. Gastroenterology 114S:A1119
Scarpa M, Barollo M, Angriman I et al (2000) Stapled end-to-side vs sutured side-to-side anastomosis in Crohn’s disease. Dig Liver Dis 32:A41
Scott NA, Sue-Ling HM, Hughes LE (1995) Anastomotic configuration does not affect recurrence of Crohn’s disease after ileocolonic resection. Int J Colorectal Dis 10:67–69
Caprilli R, Corrao G, Taddei G et al (1996) Prognostic factors for postoperative recurrence of Crohn’s disease. Gruppo Italiano per lo Studio del Colon e del Retto (GISC). Dis Colon Rectum 39:335–341
Hashemi M, Novell JR, Lewis AA (1998) Side-to-side stapled anastomosis may delay recurrence in Crohn’s disease. Dis Colon Rectum 41:1293–1296
Yamamoto T, Bain IM, Mylonakis E et al (1999) Stapled functional end-to-end anastomosis versus sutured end-to-end anastomosis after ileocolonic resection in Crohn disease. Scand J Gastroenterol 34:708–713
Munoz-Juarez M, Yamamoto T, Wolff BG et al (2001) Wide-lumen stapled anastomosis vs. conventional end-to-end anastomosis in the treatment of Crohn’s disease. Dis Colon Rectum 44:20–26
Resegotti A, Astegiano M, Farina EC et al (2005) Side-to-side stapled anastomosis strongly reduces anastomotic leak rates in Crohn’s disease surgery. Dis Colon Rectum 48:464–468
Barlow R, Price P, Reid TD et al (2011) Prospective multicentre randomised controlled trial of early enteral nutrition for patients undergoing major upper gastrointestinal surgical resection. Clin Nutr 30:560–566
Ng SC, Lied GA, Arebi N et al (2009) Clinical and surgical recurrence of Crohn’s disease after ileocolonic resection in a specialist unit. Eur J Gastroenterol Hepatol 21:551–557
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guo, Z., Li, Y., Zhu, W. et al. Comparing Outcomes Between Side-to-Side Anastomosis and Other Anastomotic Configurations After Intestinal Resection for Patients with Crohn’s Disease: A Meta-Analysis. World J Surg 37, 893–901 (2013). https://doi.org/10.1007/s00268-013-1928-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-1928-6