Abstract
Background
Intraoperative nerve monitoring (IONM) of the recurrent laryngeal nerve and the vagal nerve can detect nonfunctioning nerves (recurrent laryngeal nerve palsy, RLNP) that are visibly intact. The use of IONM is questionable, however, as we still lack evidence that it reduces the rate of postoperative nerve injuries. Since negative IONM results after thyroid dissection of the first side could change our surgical strategy and thus could prevent patients from bilateral RLNP, we questioned whether IONM results are reliable enough to base changes in surgical strategy and whether this has any effect on surgical outcome.
Methods
We retrospectively analyzed the data of 1333 consecutive patients with suggested benign bilateral thyroid disease who had been operated on under a defined protocol, including the use of a specific IONM technique (tube electrodes and stimulation of the vagal nerve and the inferior recurrent nerve before and after thyroid resection), between January 1, 2006 and December 31, 2008.
Results
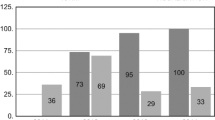
In four patients the IONM system did not work, two nerves had not been found, and in eight patients the tube had to be readjusted. Of five permanent nerve injuries, four were visible during surgery and one was suspected. Sensitivity of IONM in detecting temporary nerve injuries of macroscopically normal-appearing nerves was 93%. Specificity was 75–83% at first side of dissection and 55–67% at the second side, with an overall specificity of 77%. In 11 of 13 patients (85%) with known nerve injury (preexisting or visible) and in 20 of 36 patients (56%) with negative IONM stimulation at the first side of dissection, the surgical strategy was changed (specific surgeon or restricted resection) with no postoperative bilateral RLNP. This was in contrast to 3 of 18 (17%) bilateral RLNP (p < 0.05), when surgeons were not aware of a preexisting or highly likely nerve injury at the first side of thyroid dissection.
Conclusions
Failed IONM stimulation of the vagal or recurrent laryngeal nerve after resection of the first thyroid lobe is specific enough to reconsider the surgical strategy in patients with bilateral thyroid disease to surely prevent bilateral RLNP.
Similar content being viewed by others
References
Röher HD, Goretzki PE, Hellmann P et al (1999) Complications in thyroid surgery. Incidence and therapy. Chirurg 70:999–1010
Dralle H, Sekulla C, Lorenz K et al (2008) Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 32:1358–1366
Hermann M, Hellebart C, Freissmuth M (2004) Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg 240:9–17
Barczynski M, Konturek A, Cichon S (2009) Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 96:240–246
Chiang FY, Lu IC, Kuo WR et al (2008) The mechanism of recurrent laryngeal nerve injury during thyroid surgery–the application of intraoperative neuromonitoring. Surgery 143:743–749
Sindo M, Chheda NN (2007) Incidence of vocal cord paralysis with and without recurrent laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head Neck Surg 133:481–485
Chan WF, Lo CY (2006) Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg 30:806–812
Thomusch O, Sekulla C, Machens A et al (2004) Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg 389:499–503
Goretzki PE, Schwarz K, Lammers BJ (2009) Implementing the general use of dissection devices in thyroid surgery from prospective randomized trial to daily use. Surg Technol Int 18:87–93
Bergenfelz A, Jansson S, Kristoffersson A et al (2008) Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3, 660 patients. Langenbecks Arch Chir 393:667–673
Randolph GW, Kobler JB, Wilkins J (2004) Recurrent laryngeal nerve identification and assessment during thyroid surgery: laryngeal palpation. World J Surg 28:755–760
Sturgeon C, Sturgeon T, Angelos P (2008) Neuromonitoring in thyroid surgery: attitudes, usage patterns, and predictors of use among endocrine surgeons. World J Surg 33:417–425
Dionigi G, Bacuzzi A, Boni L et al (2008) What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg 6:S7–S12
Goretzki PE, Dotzenrath C, Witte J et al (2000) Chirurgie des Morbus Basedow. Viszeralchirurgie 35:117–123
Agarwal G, Aggarwal V (2008) Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J Surg 32:1313–1324
Pieracci FM, Fahey TJ (2008) Effect of hospital volume of thyroidectomies on outcomes following substernal thyroidectomy. World J Surg 32:740–746
Grosheva M, Wittekindt C, Pototschnig C et al (2008) Evaluation of peripheral vocal cord paralysis by electromyography. Laryngoscope 118:987–990
Sittel C, Stennert E, Thumfart WF et al (2001) Prognostic value of laryngeal electromyography in vocal fold paralysis. Arch Otolaryngol Head Neck Surg 127:155–160
Ortega J, Cassinello N, Dorcaratto D et al (2009) Computerized acoustic voice analysis and subjective scaled evaluation of the voice can avoid the need for laryngoscopy after thyroid surgery. Surgery 145:265–271
Serpell JW, Yeung MJ, Grodski S (2009) The motor fibres of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg 249:648–652
Chi SY, Lammers B, Boehner H et al (2008) Is it meaningful to preserve a palsied recurrent laryngeal nerve? Thyroid 18:363–366
Hydman J (2008) Recurrent laryngeal nerve injury. Karolinska Institutet, Larserics Digital Print AB, Bromma, Sweden
Mattsson P, Björck G, Remahl S et al (2005) Nimodipine and microsurgery induced recovery of the vocal cord after recurrent laryngeal nerve resection. Laryngoscope 115:1863–1865
Moskalenko V, Hüller M, Gasser M et al (2009) Investigation of the regeneration potential of the recurrent laryngeal nerve (RLN) after compression injury, using neuromonitoring. Langenbecks Arch Surg 394:469–474
Rosenbaum MA, Haroidas M, McHenry CR (2008) Life-threatening neck hematoma complicating thyroid and parathyroid surgery. Am J Surg 195:339–343
Leyre P, Desurmont T, Lacoste L et al (2008) Does the risk of compression hematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg 393:733–737
Polednak AP (2009) Vocal fold palsy after surgery in elderly thyroid cancer patients with versus without comorbid diabetes. Surgery 144:688–689
Henry JF, Audiffret J, Denizot A et al (1988) The non-recurrent inferior laryngeal nerve: review of 33 cases, including 2 on the left side. Surgery 104:977–984
Weiand G, Mangold G (2004) Verlaufsvarietäten des Nervus laryngeus inferior. Chirurg 75:187–195
Disclosures
The clinic acts as an educational center for IONM for outside surgeons to be trained in the use of IONM in thyroid surgery and is supported financially by Medtronic, Germany. The authors were sponsored by Medtronic, Germany, when reporting their experience of IONM in thyroid surgery to the scientific community.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goretzki, P.E., Schwarz, K., Brinkmann, J. et al. The Impact of Intraoperative Neuromonitoring (IONM) on Surgical Strategy in Bilateral Thyroid Diseases: Is it Worth the Effort?. World J Surg 34, 1274–1284 (2010). https://doi.org/10.1007/s00268-009-0353-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-009-0353-3