Abstract
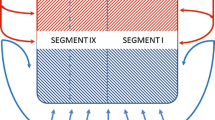
An adequate venous outflow is essential for securing viability of both graft and remnant in adult living donor liver transplantation (ALDLT). Seventy-five potential live liver donors were evaluated for LDLT by means of an “all-in-one” CT, which defined the biliary tree, portal vein, hepatic artery, and hepatic vein anatomy. The acquired data sets were further analysed by means of the software HepaVision (MeVis, Germany). Only a minority (29%) of potential donors were found to have a vascular and biliary anatomy consistent with the classically described “normal” patterns. The vast majority (71%) had “anatomical variations”. Thirty-nine (52%) donors underwent ALDLT hepatectomy. The right hepatic vein was dominant in 64 cases, representing 48 ± 6% of the total liver volume (TLV). The middle hepatic vein was dominant in 11 cases, making up 40 ± 8% of the TLV. The left hepatic vein was never dominant. The volume contribution of the middle hepatic vein (MHV) was 114–782 ml for the right and 87–419 ml for the left hemiliver. Computer-assisted planning allows for the 3D reconstruction of the vascular and biliary anatomy, automatic calculation of the total and territorial liver volumes, and risk analysis of hepatic vein dominance relationships. This comprehensive data acquisition supports preoperative evaluation and provides a high degree of safety for donors and improved outcomes for recipients.





Similar content being viewed by others
REFERENCES
Broelsch CE, Frilling A, Nadalin S, et al. Living organ donor transplantation—the German experience in comparison to others. Chirurg 2003;74:510–522.
Lee S, Park K, Hwang S, et al. Congestion of right liver graft in living donor liver transplantation. Transplantation 2001;71:812–817.
Troisi R, Ricciardi S, Smeets P, et al. Effects of hemi-portocaval shunts for inflow modulation on the outcome of small-for-size grafts in living donor liver transplantation. Am J Transpl 2005;5:1397–1404.
Marcos A, Olzinski AT, Ham JM, et al. The interrelationship between portal and arterial blood flow after adult to adult living donor liver transplantation. Transplantation 2000;70:1697–1703.
Sugawara Y, Makuuchi M, Akamatsu N, et al. Refinement of venous reconstruction using cryopreserved veins in right liver grafts. Liver Transpl 2004;10:541–547.
Sugawara Y, Makuuchi M. Advances in adult living liver transplantation: a review based on reports from the 10th anniversary of the adult-to-adult living donor liver transplantation meeting in Tokyo. Liver Transpl 2004;10:715–720.
Kubota T, Togo S, Sekido H, et al. Indications for hepatic vein reconstruction in living donor liver transplantation of right liver grafts. Transpl Proc 2003;36:2263–2266.
Tanaka K, Yamada T. Living donor liver transplantation in Japan and Kyoto University: what can we learn? Forum Liver Transpl 2005;3:25–28.
Valentin-Gamazo C, Malagò M, Karliova M, et al. Experience after the evaluation of 700 potential donors for living donor liver transplantation in a single center. Liver Transpl 2004;10:1087–1096.
Nadalin S, Malago M, Valentin-Gamazo C, et al. Preoperative donor liver biopsy for adult living donor liver transplantation: risks and benefits. Liver Transpl 2005;11:980–986.
Malago M, Molmenti EP, Paul A, et al. Hepatic venous outflow reconstruction in right live donor liver transplantation. Liver Transpl 2005;11:364–365.
Selle D, Spindler W, Preim B, et al. Mathematical methods in medical imaging: analysis of vascular structures for liver surgery planning. In Engquist B, Schmid W, editors, Mathematics Unlimited—2001 and Beyond. Berlin Heidelberg New York: Springer, 2000, pp 1039–1059
Selle D, Preim B, Schenk A, et al. Analysis of vasculature for liver surgical planning. IEEE Trans Med Imaging 2002;21:1344–1357.
Nadalin S, Testa G, Malago M, et al. Volumetric and functional recovery of the liver after right hepatectomy for living donation. Liver Transpl 2004;10:1024–1029.
Malago M, Testa G, Frilling A, et al. Right living donor liver transplantation: an option for adult patients: single institution experience with 74 patients. Ann Surg 2003;238:853–862.
Heinemann A, Wichhusen F, Puschel K, et al. Standard liver volume in the Caucasian population. Liver Transpl Surg 1999;5:366–368.
Radtke A, Schroeder T, Sotiropoulos GC, et al. Anatomical and physiological classification of hepatic vein dominance applied to liver transplantation. Eur J Med Res 2005;10:187–194.
Broelsch CE, Frilling A, Testa G, et al. Living donor liver transplantations in adults. Eur J Gastroenterol Hepatol 2003;15:3–6.
Miller CM, Gondolesi GE, Florman S, et al. One hundred nine live donor liver transplants in adults and children: a single-center experience. Ann Surg 2001;3:301–312.
Fan ST, de Villa VH, Kiuchi T, et al. Right anterior sector drainage in right-lobe live-donor liver transplantation. Transplantation 2003;75:S25–S27.
De Villa VH, Chen CL, Chen YS, et al. Right lobe living donor liver transplantation—addressing the middle hepatic vein controversy. Ann Surg 2003;238:275–282.
Marcos A. Right lobe living donor liver transplantation: a review. Liver Transpl 2000;6:3–20.
Peitgen HO, Krass S, Lang M. [Computer assistance in clinical image-based diagnosis and therapy: a challenge for German research] (in German). Rofo 2004;176:297–301.
Peitgen HO, Preim B. Virtual reality in radiology. Between hope and dilemma. Radiologe 2000;40:203–210.
Bogetti JD, Herts BR, Sands MJ, et al. Accuracy and utility of 3-dimensional computed tomography in evaluating donors for adult living related liver transplants. Liver Transpl 2001;7:687–692.
Brancatelli G, Katyal S, Federle MP, et al. Three-dimensional multislice helical computed tomography with the volume rendering technique in the detection of vascular complications after liver transplantation. Transplantation 2002;73:237–242.
Hiroshige S, Nishizaki T, Soejima Y, et al. Beneficial effects of 3-dimensional visualization on hepatic vein reconstruction in living donor liver transplantation using right lobe graft. Transplantation 2001;72:1993–1996.
Kamel IR, Kruskal JB, Keogan MT, et al. Multidetector CT of potential right-lobe liver donors. AJR Am J Roentgenol 2001;177:645–651.
Kanazawa A, Hirohashi K, Tanaka H, et al. Usefulness of three-dimensional computed tomography in a living-donor extended right lobe liver transplantation. Liver Transpl 2002;8:1076–1079.
Saito S, Yamanaka J, Miura K, et al. A novel 3D hepatectomy simulation based on liver circulation: application to liver resection and transplantation. Hepatology 2005;41:1297–1304.
Oldhafer KJ, Hogemann D, Stamm G, et al. 3-dimensional (3-D) visualization of the liver for planning extensive liver resections. Chirurg 1999;70:233–238.
Oldhafer KJ, Preim B, Dorge C, et al. Acceptance of computer-assisted surgery planning in visceral (abdominal) surgery. Zentralbl Chir 2002;127:128–133.
Lamade W, Glombitza G, Fischer L, et al. The impact of 3-dimensional reconstructions on operation planning in liver surgery. Arch Surg 2000;135:1256–1261.
Lang H, Radtke A, Liu C, et al. Extended left hepatectomy—modified operation planning based on three-dimensional visualization of liver anatomy. Langenbecks Arch Surg 2004;389:306–310.
Lang H, Radtke A, Hindennach M, et al. Impact of virtual tumor resection and computer-assisted risk analysis on operation planning and intraoperative strategy in major hepatic resection. Arch Surg 2005;140:629–638.
ACKNOWLEDGEMENT
This study was supported by a grant from the German Society for Research: Nr: 117/1-1:A2.2.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radtke, A., Nadalin, S., Sotiropoulos, G.C. et al. Computer-Assisted Operative Planning in Adult Living Donor Liver Transplantation: A New Way to Resolve the Dilemma of the Middle Hepatic Vein. World J. Surg. 31, 175–185 (2007). https://doi.org/10.1007/s00268-005-0718-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0718-1