Abstract
Purpose
Living donor liver transplantation (LDLT) is a widely accepted option to address the lack of a deceased liver program for transplantation. Understanding vascular and biliary anatomy and their variants is crucial for successful and safe graft harvesting. Anatomic variations are common, particularly in the right hepatic lobe. To provide evidence for screening potential liver transplant donors, the presence of vascular and biliary anatomic variations in Pakistan’s preoperative assessment of transplantation donor candidates was explored.
Methods
This retrospective cross-sectional study evaluated the hepatic artery, portal vein, hepatic vein, and biliary variations in living liver donors. The study included 400 living liver donors; data were collected from March 2019 to March 2023. We used a CT scan and MRCP to assess the anatomical variations.
Results
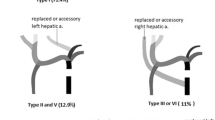
The study examined 400 liver donors aged 18 to 53 years. Conventional arterial anatomy was the most common (65.8%), followed by replaced right hepatic artery (16%) and replaced left hepatic artery (10.8%). Conventional type 1 biliary anatomy was seen in 65.8% of cases. The dominant right hepatic vein was found in 13.3% of donors. There was a significant association between the prevalence of variant portal venous anatomy with variant biliary anatomy.
Conclusion
Variations of the hepatic arterial, portal venous, and biliary systems are frequent and should be carefully evaluated while selecting a suitable living donor. A strong relationship between variant portal venous and biliary anatomy was found. These findings can aid in selecting suitable candidates and improving surgical planning for liver transplantation.
Similar content being viewed by others
Data availability
Data can be provided upon reasonable request.
References
Adam R, McMaster P, O’Grady JG et al (2003) Evolution of liver transplantation in Europe: report of the European Liver Transplant Registry. Liver Transpl 9:1231–1243. https://doi.org/10.1016/j.lts.2003.09.018
Settmacher U, Neuhaus P (2003) Innovations in liver surgery through transplantation from living donors. Chirurg 74:536–546. https://doi.org/10.1007/s00104-003-0675-x
Sugawara Y, Makuuchi M, Takayama T et al (2002) Safe donor hepatectomy for living related liver transplantation. Liver Transpl 8:58–62. https://doi.org/10.1053/jlts.2002.29761
Zhuang ZG, Qian LJ, Gong HX et al (2008) Multidetector computed tomography angiography in the evaluation of potential living donors for liver transplantation: single-center experience in China. Transplant Proc 40:2466–2477. https://doi.org/10.1016/j.transproceed.2008.08.031
Schroeder T, Malagó M, Debatin JF et al (2005) “All-in-one” imaging protocols for the evaluation of potential living liver donors: comparison of magnetic resonance imaging and multidetector computed tomography. Liver Transpl 11:776–787. https://doi.org/10.1002/lt.20429
Right lobe living donor liver transplantation - PubMed. https://pubmed.ncbi.nlm.nih.gov/10515380/. Accessed 15 Apr 2023
Hidajat N, Vogl TJ, Möller M et al (1996) Intravenous spiral CT angiography for assessment before orthotopic liver transplantation: comparisons between tomography, MIP, 3-dimensional surface imaging and intra-arterial DSA. Rofo 165:445–451. https://doi.org/10.1055/s-2007-1015787
Cheng YF, Lee TY, Chen CL et al (1997) Three-dimensional helical computed tomographic cholangiography: application to living related hepatic transplantation. Clin Transpl 11:209–213
Sahani D, Mehta A, Blake M et al (2004) Preoperative hepatic vascular evaluation with CT and MR angiography: implications for surgery. Radiographics 24:1367–1380. https://doi.org/10.1148/rg.245035224
Jehangir M, Nazir R, Jang A et al (2016) Macrovesicular steatosis in living related liver donors: correlation of biopsy findings with CT liver attenuation index and body mass index. Clin Transpl 30:1016–1020. https://doi.org/10.1111/ctr.12782
Nakamura T, Tanaka K, Kiuchi T et al (2002) Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation 73:1896–1903. https://doi.org/10.1097/00007890-200206270-00008
Varotti G, Gondolesi GE, Goldman J et al (2004) Anatomic variations in right liver living donors. J Am Coll Surg 198:577–582. https://doi.org/10.1016/j.jamcollsurg.2003.11.014
Varotti G, Gondolesi GE, Goldman J et al (2004) Anatomic variations in right liver living donors1. J Am Coll Surg 198:577–582. https://doi.org/10.1016/j.jamcollsurg.2003.11.014
Noussios G, Dimitriou I, Chatzis I, Katsourakis A (2017) The main anatomic variations of the hepatic artery and their importance in surgical practice: review of the literature. J Clin Med Res 9:248–252. https://doi.org/10.14740/jocmr2902w
Couinaud C (1981) Controlled hepatectomies and exposure of the intrahepatic bile ducts. Anatomical and Technical Study 1981:73–82
Strasberg SM, Belghiti J, Clavien P-A et al (2000) The Brisbane 2000 terminology of liver anatomy and resections. HPB 2:333–339. https://doi.org/10.1016/S1365-182X(17)30755-4
Marcos A, Fisher RA, Ham JM et al (2000) Selection and outcome of living donors for adult to adult right lobe transplantation. Transplantation 69:2410–2415. https://doi.org/10.1097/00007890-200006150-00034
Koc Z, Ulusan S, Oguzkurt L, Tokmak N (2007) Venous variants and anomalies on routine abdominal multi-detector row CT. Eur J Radiol 61:267–278. https://doi.org/10.1016/j.ejrad.2006.09.008
Macdonald DB, Haider MA, Khalili K et al (2005) Relationship between vascular and biliary anatomy in living liver donors. AJR Am J Roentgenol 185:247–252. https://doi.org/10.2214/ajr.185.1.01850247
Lee VS, Morgan GR, Lin JC et al (2004) Liver transplant donor candidates: associations between vascular and biliary anatomic variants. Liver Transpl 10:1049–1054. https://doi.org/10.1002/lt.20181
Cheng YF, Huang TL, Chen CL et al (1997) Anatomic dissociation between the intrahepatic bile duct and portal vein: risk factors for left hepatectomy. World J Surg 21:297–300. https://doi.org/10.1007/s002689900232
Atri M, Bret PM, Fraser-Hill MA (1992) Intrahepatic portal venous variations: prevalence with US. Radiology 184:157–158. https://doi.org/10.1148/radiology.184.1.1609075
Ayoub EI, Fayed Y, Omar H et al (2020) The impact of donor’s biliary anatomy variations on the procedure of living donor liver transplantation. Egypt J Surg 39:706. https://doi.org/10.4103/ejs.ejs_53_20
Naeem MQ, Ahmed MS, Hamid K et al (2020) Prevalence of different hepatobiliary tree variants on magnetic resonance cholangiopancreatography in patients visiting a tertiary care teaching hospital in Karachi. Cureus. 12(12):e12329. https://doi.org/10.7759/cureus.12329
Takayasu K, Moriyama N, Muramatsu Y et al (1985) Intrahepatic portal vein branches studied by percutaneous transhepatic portography. Radiology 154:31–36. https://doi.org/10.1148/radiology.154.1.3964948
Tanano H, Hasegawa T, Kawahara H et al (1999) Biliary atresia associated with congenital structural anomalies. J Pediatr Surg 34:1687–1690. https://doi.org/10.1016/s0022-3468(99)90645-0
Desmet VJ (1998) Ludwig symposium on biliary disorders--part I. Pathogenesis of ductal plate abnormalities. Mayo Clin Proc 73:80–89. https://doi.org/10.4065/73.1.80
Chen JS, Yeh BM, Wang ZJ et al (2005) Concordance of second-order portal venous and biliary tract anatomies on MDCT angiography and MDCT cholangiography. Am J Roentgenol 184:70–74. https://doi.org/10.2214/ajr.184.1.01840070
Schmidt S, Demartines N, Soler L et al (2008) Portal vein normal anatomy and variants: implication for liver surgery and portal vein embolization. Semin Interv Radiol 25:086–091. https://doi.org/10.1055/s-2008-1076688
Takeishi K, Shirabe K, Yoshida Y et al (2015) Correlation between portal vein anatomy and bile duct variation in 407 living liver donors. Am J Transplant 15:155–160. https://doi.org/10.1111/ajt.12965
Catalano OA, Singh AH, Uppot RN et al (2008) Vascular and biliary variants in the liver: implications for liver surgery. RadioGraphics 28:359–378. https://doi.org/10.1148/rg.282075099
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Abdullah Khalid and M. Asad Saleem. Abdullah Khalid wrote the first draft of the manuscript, and all authors commented on previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Ethics approval and consent to participate
The study was approved by the Institutional Review Board at Pakistan Kidney and Liver Institute & Research Center.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khalid, A., Saleem, M.A., Ihsan-ul-Haq et al. Anatomical variations in living donors for liver transplantation—prevalence and relationship. Langenbecks Arch Surg 408, 323 (2023). https://doi.org/10.1007/s00423-023-03066-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-03066-1