Abstract
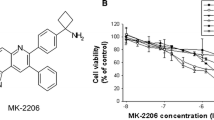
Myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML) are characterized by risk of relapses, poor survival, unwanted side effects and high toxicity with the current therapies. In light of these facts, there are efforts to develop new drugs specific for deregulated molecules that participate in leukemia pathogenesis. Hematopoietic cell kinase (HCK), an Src kinase family member, is overexpressed on hematopoietic stem cells of MDS and de novo AML patients and involved in the oncogenic process. Thus, we investigated in vitro, ex vivo and in vivo effects of a novel chemical compound targeting HCK inhibition (iHCK-37), in combination with the most used drugs for the treatment of MDS and de novo AML, 5-Azacytidine and Cytarabine. Herein, the combination treatment with iHCK-37 and 5-Azacytidine or Cytarabine demonstrated additive effects against leukemia cells, compared to either drug alone. iHCK-37 plus 5-Azacytidine or Cytarabine treatment was able to reduce the activation of oncogenic pathways, MAPK/ERK and PI3K/AKT, leading to reduction of ERK and AKT phosphorylation, and increased BAX and decreased BCL-XL protein expression. Moreover, treatment with iHCK-37 reduced MDS and AML CD34-positive cell numbers inside a 3D-structure but did not affect normal CD34-positive cell numbers. In vivo analysis showed that leukemic mice treated with iHCK-37 had reduced ERK and AKT proteins phosphorylation levels and leukocyte numbers. In conclusion, the iHCK-37 inhibitor has anti-neoplastic activity in leukemia cells without altering apoptosis and survival rate of normal cells, suggesting on-target malignant cell killing activity as a single agent or in combination with 5-Azacytidine or Cytarabine.





Similar content being viewed by others
References
Siveen KS, Uddin S, Mohammad RM (2017) Targeting acute myeloid leukemia stem cell signaling by natural products. Mol Cancer 16(1):13. https://doi.org/10.1186/s12943-016-0571-x
Ades L, Itzykson R, Fenaux P (2014) Myelodysplastic syndromes. Lancet 383(9936):2239–2252. https://doi.org/10.1016/S0140-6736(13)61901-7
Brunner AM, Neuberg DS, Wander SA, Sadrzadeh H, Ballen KK, Amrein PC, Attar E, Hobbs GS, Chen YB, Perry A, Connolly C, Joseph C, Burke M, Ramos A, Galinsky I, Yen K, Yang H, Straley K, Agresta S, Adamia S, Borger DR, Iafrate A, Graubert TA, Stone RM, Fathi AT (2019) Isocitrate dehydrogenase 1 and 2 mutations, 2-hydroxyglutarate levels, and response to standard chemotherapy for patients with newly diagnosed acute myeloid leukemia. Cancer 125(4):541–549. https://doi.org/10.1002/cncr.31729
Dombret H, Gardin C (2016) An update of current treatments for adult acute myeloid leukemia. Blood 127(1):53–61. https://doi.org/10.1182/blood-2015-08-604520
El-Jawahri A, Abel GA, Traeger L, Waldman L, Markovitz N, VanDusen H, Fathi A, Steensma DP, LeBlanc TW, Horick NK, DeAngelo DJ, Wadleigh M, Hobbs G, Foster J, Brunner AM, Amrein P, Stone RM, Temel JS, Greer JA (2019) Quality of life and mood of older patients with acute myeloid leukemia (AML) receiving intensive and non-intensive chemotherapy. Leukemia 33(10):2393–2402. https://doi.org/10.1038/s41375-019-0449-1
Mohammadi M, Cao Y, Glimelius I, Bottai M, Eloranta S, Smedby KE (2015) The impact of comorbid disease history on all-cause and cancer-specific mortality in myeloid leukemia and myeloma – a Swedish population-based study. BMC Cancer 15:850. https://doi.org/10.1186/s12885-015-1857-x
Dubois F, Leroy C, Simon V, Benistant C, Roche S (2015) YES oncogenic activity is specified by its SH4 domain and regulates RAS/MAPK signaling in colon carcinoma cells. Am J Cancer Res 5(6):1972–1987
Amata I, Maffei M, Pons M (2014) Phosphorylation of unique domains of Src family kinases. Front Genet 5:181. https://doi.org/10.3389/fgene.2014.00181
Aleshin A, Finn RS (2010) SRC: a century of science brought to the clinic. Neoplasia 12(8):599–607. https://doi.org/10.1593/neo.10328
Dos Santos C, Demur C, Bardet V, Prade-Houdellier N, Payrastre B, Recher C (2008) A critical role for Lyn in acute myeloid leukemia. Blood 111(4):2269–2279. https://doi.org/10.1182/blood-2007-04-082099
Dos Santos C, McDonald T, Ho YW, Liu H, Lin A, Forman SJ, Kuo YH, Bhatia R (2013) The Src and c-Kit kinase inhibitor dasatinib enhances p53-mediated targeting of human acute myeloid leukemia stem cells by chemotherapeutic agents. Blood 122(11):1900–1913. https://doi.org/10.1182/blood-2012-11-466425
Shen K, Moroco JA, Patel RK, Shi H, Engen JR, Dorman HR, Smithgall TE (2018) The src family kinase fgr is a transforming oncoprotein that functions independently of SH3-SH2 domain regulation. Sci Signal. https://doi.org/10.1126/scisignal.aat5916
Baratti MO, Moreira YB, Traina F, Costa FF, Verjovski-Almeida S, Olalla-Saad ST (2010) Identification of protein-coding and non-coding RNA expression profiles in CD34+ and in stromal cells in refractory anemia with ringed sideroblasts. BMC Med Genomics 3:30. https://doi.org/10.1186/1755-8794-3-30
Roversi FM, Pericole FV, Machado-Neto JA, Duarte ADSS, Longhini AL, Corrocher FA, Palodetto B, Ferro KP, Rosa RG, Baratti MO, Verjovski-Almeida S, Traina F, Molinari A, Botta M (1863) Saad SOT (2017) Hematopoietic cell kinase (HCK) is a potential therapeutic target for dysplastic and leukemic cells due to integration of erythropoietin/PI3K pathway and regulation of erythropoiesis: HCK in erythropoietin/PI3K pathway. Biochim et Biophys Acta (BBA)- Mol Basis Dis 2:450–461. https://doi.org/10.1016/j.bbadis.2016.11.013
Chen Z, Shen S, Shi W, Jiang G, Wang X, Jian H, Zhou Z, Ding Z, Lu S (2019) Intercalated combination of chemotherapy and erlotinib for stage IIIA non-small-cell lung cancer: a multicenter, open-label, single-arm, phase II study. Cancer Manag Res 11:6543–6552. https://doi.org/10.2147/CMAR.S189287
Boehrer S, Galluzzi L, Lainey E, Bouteloup C, Tailler M, Harper F, Pierron G, Adès L, Thépot S, Sébert M, Gardin C, de Botton S, Fenaux P, Kroemer G (2011) Erlotinib antagonizes constitutive activation of SRC family kinases and mTOR in acute myeloid leukemia. Cell Cycle 10(18):3168–3175. https://doi.org/10.4161/cc.10.18.16599
Taylor JW, Dietrich J, Gerstner ER, Norden AD, Rinne ML, Cahill DP, Stemmer-Rachamimov A, Wen PY, Betensky RA, Giorgio DH, Snodgrass K, Randall AE, Batchelor TT, Chi AS (2015) Phase 2 study of bosutinib, a Src inhibitor, in adults with recurrent glioblastoma. J Neurooncol 121(3):557–63. https://doi.org/10.1007/s11060-014-1667-z
Bieerkehazhi S, Chen Z, Zhao Y, Yu Y, Zhang H, Vasudevan SA, Woodfield SE, Tao L, Yi JS, Muscal JA, Pang JC, Guan S, Zhang H, Nuchtern JG, Li H, Li H, Yang J (2017) Novel Src/Abl tyrosine kinase inhibitor bosutinib suppresses neuroblastoma growth via inhibiting Src/Abl signaling. Oncotarget 8(1):1469–1480. https://doi.org/10.18632/oncotarget.13643
MacDonald RJ, Bunaciu RP, Ip V, Dai D, Tran D, Varner JD, Yen A (2018) Src family kinase inhibitor bosutinib enhances retinoic acid-induced differentiation of HL-60 leukemia cells. Leuk Lymphoma 59(12):2941–2951. https://doi.org/10.1080/10428194.2018.1452213
Weir MC, Shu ST, Patel RK, Hellwig S, Chen L, Tan L, Gray NS, Smithgall TE (2018) Selective inhibition of the myeloid src-family kinase fgr potently suppresses AML cell growth in vitro and in vivo. ACS Chem Biol 13(6):1551–1559. https://doi.org/10.1021/acschembio.8b00154
Tintori C, Laurenzana I, La Rocca F, Falchi F, Carraro F, Ruiz A, Esté JA, Kissova M, Crespan E, Maga G, Biava M, Brullo C, Schenone S, Botta M (2013) Identification of Hck inhibitors as hits for the development of antileukemia and anti-HIV agents. ChemMedChem 8(8):1353–1360. https://doi.org/10.1002/cmdc.201300204
Ugo V, Marzac C, Teyssandier I, Larbret F, Lécluse Y, Debili N, Vainchenker W, Casadevall N (2004) Multiple signaling pathways are involved in erythropoietin-independent differentiation of erythroid progenitors in polycythemia vera. Exp Hematol 32(2):179–187. https://doi.org/10.1016/j.exphem.2003.11.003
He LZ, Tribioli C, Rivi R, Peruzzi D, Pelicci PG, Soares V, Cattoretti G, Pandolfi PP (1997) Acute leukemia with promyelocytic features in PML/RARalpha transgenic mice. Proc Natl Acad Sci U S A 94(10):5302–5307. https://doi.org/10.1073/pnas.94.10.5302
Rego EM, Ruggero D, Tribioli C (2006) Leukemia with distinct phenotypes in transgenic mice expressing PML/RAR alpha. PLZF/RAR alpha or NPM/RAR alpha Oncogene 25(13):1974–1979. https://doi.org/10.1038/sj.onc.1209216
dos Santos GA, e Abreu Lima RS, Pestana CR, Lima AS, Scheucher PS, Thomé CH, Gimenes-Teixeira HL, Santana-Lemos BA, Lucena-Araujo AR, Rodrigues FP, Nasr R, Uyemura SA, Falcão RP, de Thé H, Pandolfi PP, Curti C, Rego EM (2012) (+)α-Tocopheryl succinate inhibits the mitochondrial respiratory chain complex I and is as effective as arsenic trioxide or ATRA against acute promyelocytic leukemia in vivo. Leukemia. 26(3):451–60. https://doi.org/10.1038/leu.2011.216
Jácomo RH, Santana-Lemos BA, Lima AS et al (2012) Methionine induced hyper homocysteinemia reverts fibrinolytic pathway activation in a murine model of acute promyelocytic leukemia. Blood 120(1):207–213. https://doi.org/10.1182/blood-2011-04-347187
Ferreira AK, Santana-Lemos BA, Rego EM, Filho OM, Chierice GO, Maria DA (2013) Synthetic phosphoethanolamine has in vitro and in vivo anti-leukemia effects. Br J Cancer 109(11):2819–2828. https://doi.org/10.1038/bjc.2013.510
Torello CO, Shiraishi RN, Della Via FI, Castro TCL, Longhini AL, Santos I, Bombeiro AL, Silva CLA, Queiroz MLS, Rego EM, Saad STO (2018) Reactive oxygen species production triggers green tea-induced anti-leukaemic effects on acute promyelocytic leukaemia model. Cancer Lett 414:116–126. https://doi.org/10.1016/j.canlet.2017.11.006
Braicu C, Buse M, Busuioc C, Drula R, Gulei D, Raduly L, Rusu A, Irimie A, Atanasov AG, Slaby O, Ionescu C, Berindan-Neagoe I (2019) A comprehensive review on MAPK: a promising therapeutic target in cancer. Cancers (Basel) 11(10):1618. https://doi.org/10.3390/cancers11101618
Bianco JER, Rosa RG, Congrains-Castillo A, Joazeiro PP, Waldman SD, Weber JF, Saad STO (2019) Characterization of a novel decellularized bone marrow scaffold as an inductive environment for hematopoietic stem cells. Biomat Sci 7(4):1516–1528. https://doi.org/10.1039/c8bm01503a
Adelman ER, Huang HT, Roisman A, Olsson A, Colaprico A, Qin T, Lindsley RC, Bejar R, Salomonis N, Grimes HL, Figueroa ME (2019) Aging human hematopoietic stem cells manifest profound epigenetic reprogramming of enhancers that may predispose to leukemia. Cancer Discov 9(8):1080–1101. https://doi.org/10.1158/2159-8290.CD-18-1474
Shih AH, Abdel-Wahab O, Patel JP, Levine RL (2012) The role of mutations in epigenetic regulators in myeloid malignancies. Nat Rev Cancer 12:599–612. https://doi.org/10.1038/nrc3343
Klepin HD (2016) Myelodysplastic syndromes and acute myeloid leukemia in the elderly. Clin Geriatr Med 32(1):155–173. https://doi.org/10.1016/j.cger.2015.08.010
Juliusson G, Lazarevic V, Hörstedt AS, Hagberg O, Höglund M (2012) Acute leukemia registry group. Acute myeloid leukemia in the real world: why population-based registries are needed. Blood 119(17):3890–3899. https://doi.org/10.1182/blood-2011-12-379008
Mufti GJ, Potter V (2012) Myelodysplastic syndromes: who and when in the course of disease to transplant. Hematology Am Soc Hematol Educ Program 1:49–55. https://doi.org/10.1182/asheducation-2012.1.49
Bayat Mokhtari R, Homayouni TS, Baluch N, Morgatskaya E, Kumar S, Das B, Yeger H (2017) Combination therapy in combating cancer. Oncotarget 8(23):38022–38043. https://doi.org/10.18632/oncotarget.16723
Miyamoto K, Minami Y (2019) Precision medicine and novel molecular target therapies in acute myeloid leukemia: the background of hematologic malignancies (HM)-SCREEN-Japan 01. Int J Clin Oncol. 24(8):893–898. https://doi.org/10.1007/s10147-019-01467-1
Poh AR, O’Donoghue RJ, Ernst M (2015) Hematopoietic cell kinase (HCK) as a therapeutic target in immune and cancer cells. Oncotarget 6:15752–15771. https://doi.org/10.18632/oncotarget.4199
Singh R, Letai A, Sarosiek K (2019) Regulation of apoptosis in health and disease: the balancing act of BCL-2 family proteins. Nat Rev Mol Cell Biol 20(3):175–193. https://doi.org/10.1038/s41580-018-0089-8
Youle RJ, Strasser A (2008) The BCL-2 protein family: opposing activities that mediate cell death. Nat Rev Mol Cell Biol 9(1):47–59. https://doi.org/10.1038/nrm2308
Jin S, Cojocari D, Purkal JJ, Popovic R, Talaty NN, Xiao Y, Solomon LR, Boghaert ER, Leverson JD, Phillips DC (2020) 5-azacytidine induces NOXA to prime AML cells for venetoclax-mediated apoptosis. Clin Cancer Res 26(13):3371–3383. https://doi.org/10.1158/1078-0432.CCR-19-1900
Wouters BJ, Delwel R (2016) Epigenetics and approaches to targeted epigenetic therapy in acute myeloid leukemia. Blood 127(1):42–52. https://doi.org/10.1182/blood-2015-07-604512
Pillinger G, Loughran NV, Piddock RE, Shafat MS, Zaitseva L, Abdul-Aziz A, Lawes MJ, Bowles KM, Rushworth SA (2016) Targeting PI3Kdelta and PI3Kgamma signalling disrupts human AML survival and bone marrow stromal cell mediated protection. Oncotarget 7(26):39784–39795. https://doi.org/10.18632/oncotarget.9289
Zhou C, Du J, Zhao L, Liu W, Zhao T, Liang H, Fang P, Zhang K, Zeng H (2021) GLI1 reduces drug sensitivity by regulating cell cycle through PI3K/AKT/GSK3/CDK pathway in acute myeloid leukemia. Cell Death Dis 12(3):231. https://doi.org/10.1038/s41419-021-03504-2
Acknowledgements
The authors would like to thank Raquel S Foglio (Hematology and Transfusion Medicine Center, University of Campinas, São Paulo, Brazil) for the English revision; Ana Leda Longhini (University of Alabama, Birmingham, AL, USA) and Irene Santos (Hematology and Transfusion Medicine Center, University of Campinas, São Paulo, Brazil) for flow cytometry assistance; Renata Giardini Rosa and Juares Ednaldo Romero Bianco for the development of scaffold material; and Alessio Molinari and Maurizzio Bottas (in memoriam) (Dipartimento di Biotecnologie, Chimica e Farmacia-Università degli Studi di Siena, Siena, Italy) for the synthesis of iHCK-37 compound. We also thank the National Institute of Science and Technology on Photonics Applied to Cell Biology (INFABIC) at UNICAMP for the access to equipment and confocal assistance and analysis (FAPESP Grants 2014/50938-8 and CNPq Grants 465699/2014-6) and the Hemostasis Laboratory of Hematology and Transfusion Medicine Center (FAPESP Grants 2016/14172-6) at UNICAMP for cell proliferation analysis by IncuCyte S3 System (Sartorius). The authors also thank CNPq, FAPESP, and INCT-Sangue for the financial support.
Funding
This study was funded by grants from the Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP Grants 2011/22376–7, and 2017/21801–2) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Author information
Authors and Affiliations
Contributions
Fernanda Marconi Roversi was the principal investigator of this study, designing and performing the experiments, collecting, analyzing and interpreting data, and writing the manuscript; Maura Lima Pereira Bueno, Juliete Aparecida Francisco da Silva, Guilherme Rossi Assis-Mendonça contributed in the experiments and in the writing of the manuscript; Cristiane Okuda Torello, Rodrigo Nato Shiraishi, Karla Priscila Ferro, Eduardo Magalhães Rego contributed to mice experiments; Adriana Santos Silva Duarte carried out the cell separation; Fernando Viera Pericole acted as the reference physician and helped to analyze the data; Sara Teresinha Olalla Saad provided the study conception, directed the research, provided financial support, revised and gave final approval of the manuscript. All the authors read and approved the final manuscript and agreed that they are accountable for all the aspects of the work and assure the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roversi, F.M., Bueno, M.L.P., da Silva, J.A.F. et al. Novel inhibitor of hematopoietic cell kinase as a potential therapeutic agent for acute myeloid leukemia. Cancer Immunol Immunother 71, 1909–1921 (2022). https://doi.org/10.1007/s00262-021-03111-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-021-03111-2