Abstract
Background
For the diagnosis of prosthetic joint infection, real evidence-based guidelines to aid clinicians in choosing the most accurate diagnostic strategy are lacking.
Aim and Methods
To address this need, we performed a multidisciplinary systematic review of relevant nuclear medicine, radiological, orthopaedic, infectious, and microbiological literature to define the diagnostic accuracy of each diagnostic technique and to address and provide evidence-based answers on uniform statements for each topic that was found to be important to develop a commonly agreed upon diagnostic flowchart.
Results and Conclusion
The approach used to prepare this set of multidisciplinary guidelines was to define statements of interest and follow the procedure indicated by the Oxford Centre for Evidence-based Medicine (OCEBM).
Similar content being viewed by others
Preamble
The European Association of Nuclear Medicine (EANM) is a professional nonprofit medical association that facilitates communication worldwide between individuals pursuing clinical and research excellence in nuclear medicine. The EANM was founded in 1985. EANM members are physicians, technologists, and scientists specializing in the research and practice of nuclear medicine.
The EANM will periodically define new guidelines for nuclear medicine practice to help advance the science of nuclear medicine and to improve the quality of service to patients throughout the world. Existing practice guidelines will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated.
Each practice guideline, representing a policy statement by the EANM, has undergone a thorough consensus process in which it has been subjected to extensive review. The EANM recognizes that the safe and effective use of diagnostic nuclear medicine imaging requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice guideline by those entities not providing these services is not authorized.
These guidelines are an educational tool designed to assist practitioners in providing appropriate care for patients. They are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care. For these reasons and those set forth below, the ESR, EBJIS, ESCMID, and the EANM suggest caution against the use of these guidelines in litigation in which the clinical decisions of a practitioner are called into question.
The ultimate judgment regarding the propriety of any specific procedure or course of action must be made by the physician or medical physicist in light of all the circumstances presented. Thus, there is no implication that an approach differing from the guidelines, standing alone, is below the standard of care. To the contrary, a conscientious practitioner may responsibly adopt a course of action different from that set forth in the guidelines when, in the reasonable judgment of the practitioner, such course of action is indicated by the condition of the patient, limitations of available resources, or advances in knowledge or technology subsequent to publication of the guidelines.
The practice of medicine includes both the art and the science of the prevention, diagnosis, alleviation, and treatment of disease. The variety and complexity of human conditions makes it impossible to always reach the most appropriate diagnosis or to predict with certainty a particular response to treatment. Therefore, it should be recognized that adherence to these guidelines will not ensure an accurate diagnosis or a successful outcome. All that should be expected is that the practitioner will follow a reasonable course of action based on current knowledge, available resources, and the needs of the patient, to deliver effective and safe medical care. The sole purpose of these guidelines is to assist practitioners in achieving this objective.
Introduction
Because of increased life expectancy, the number of joint prosthesis replacements continues to grow at a significant rate, with several millions prosthetic joints implanted each year worldwide [1]. Most of the time this surgery results in better joint function and pain relief, and the procedure itself is safe and cost-effective [2]. However, prosthetic joint infection (PJI) is a complication that can occur, with an incidence ranging from 2.0% to 2.4% for primary interventions [3], but increasing to as high as 20% for revision procedures [4], leading to a true economic burden, since costs are very high when an infection develops [3]. PJI is a serious condition that may lead to repeated surgical interventions, prolonged hospitalization, high costs, and significant morbidity, although low mortality.
PJIs are usually classified in relation to the time of onset after surgery: (i) early, within the first 3 months after surgery, (ii) delayed (between 3 months and 2 years after surgery), and (iii) late (more than 2 years after surgery) [5]. Microorganisms may reach the prosthesis at the time of implantation or later by haematogenous spread [6, 7].
Early infection is often easy to recognize by acute pain in the wound area, redness, swelling, wound leakage, heat, and fever. Late infection is often caused by haematogenous spread, with symptoms from both the affected joint and the primary infection site. The main diagnostic problem is the delayed, often low-grade infection with mostly nonspecific symptoms. In all PJIs, a delay in starting an appropriate antibiotic regimen and surgical treatment has an important impact on the chance of saving the prosthesis and joint function. Therefore, early diagnosis is of utmost importance.
There is no single routine test available that can diagnose PJI with sufficient accuracy. Cultures, biopsies, serum inflammatory markers, and imaging techniques all have their pros and cons. C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and leukocyte count are not sensitive or specific enough to detect or exclude a PJI. Joint aspiration itself involves a risk of infection, and its sensitivity is highly variable. In general, a combination of clinical, laboratory, microbiological, and imaging tests are performed based on personal experience, techniques available in the institute, and cost aspects. Indeed, most signs and symptoms that might indicate the presence of a PJI may be simply related to an aseptic loosening of the prosthesis or to a soft tissue infection. Since loosening, soft tissue infection without osteomyelitis, and PJI require different treatment strategies (NSAIDs, antibiotic therapy, or surgery for explant and re-implant), the correct differential diagnosis among these clinical situations is crucial.
The development of biofilms plays a strategic role in the pathogenesis of PJI. Microorganisms adhere to the implant and form a biofilm, within which they are protected from the host immune system and most antibiotics [7, 8]. The most frequent etiologic agents are staphylococci, accounting for more than 50% of PJIs [8]. Staphylococcus aureus is most commonly isolated in early infection, whereas coagulase-negative staphylococci are more frequent in late infection [8].
Other commonly isolated organisms in late infections are streptococci (9–10%), enterococci (3–7%), and anaerobes (2–4%) [7]. Gram-negative bacteria, mostly Pseudomonas aeruginosa, Enterobacter spp., and Proteus spp., even if relatively uncommon agents, have an important clinical impact because of the difficulty in treating them [9, 10]. Overall, about 20% of PJIs are polymicrobial and 7–11% are culture-negative [11, 12]. Unusual pathogens such as Candida spp., Brucella spp., and mycobacteria have also been reported [13].
Other commonly isolated organisms in late infections are streptococci (9–10%), enterococci (3–7%), and anaerobes (2–4%) [7]. Gram-negative bacteria, mostly Pseudomonas aeruginosa, Enterobacter spp., and Proteus spp., even if relatively uncommon agents, have an important clinical impact because of the difficulty in treating them [9, 10]. Overall, about 20% of PJIs are polymicrobial and 7–11% are culture-negative [11, 12]. Unusual pathogens such as Candida spp., Brucella spp., and mycobacteria have also been reported [13].
There are several papers available with recommendations for diagnosing PJI, all with limitations: not focusing strictly on PJI, not focused on a diagnostic flow chart, not including nuclear medicine, based only on expert opinion and/or local consensus meetings, or not up to date (not analysing the currently available diagnostic techniques). Therefore, multidisciplinary evidence-based guidelines are needed, including the most relevant imaging techniques to support the most accurate diagnostic strategy. To achieve this goal, nuclear medicine physicians organized a pre-congress meeting with infectious disease specialists, radiologists, and orthopaedic surgeons on the occasion of the 20th congress of the European Association of Nuclear Medicine (EANM), where each professional discipline explained their points of view, and together they drafted a possible diagnostic flowchart for PJI [14]. As this was still only expert opinion, the aim now becomes to define a real evidence-based diagnostic flowchart for PJI by performing a thorough systematic review of the relevant literature in the areas of nuclear medicine, radiology, infectious diseases, and microbiology to define the diagnostic accuracy of each technique and to address and provide evidence-based answers on uniform statements for each topic found to be important for developing a diagnostic flowchart.
Methods
Working group
After several joint symposia and reading of several available guidelines based only on expert opinion, we recognised that a multidisciplinary evidence-based guideline for diagnosing peripheral bone infections was needed. This joint society project started in 2015, and a working group was created with delegates from four European societies: the European Association of Nuclear Medicine (EANM), the European Society of Radiology (ESR), the European Bone and Joint Infection Society (EBJIS), and the European Society of Clinical Microbiology and Infectious Diseases (ESCMID). The delegates first met in Vienna (November 2015) to define the statements and after that in Rome (February 2016) to jointly define the revised and final statements, based on the literature evidence that had first been circulated among all participants. Finally, all delegates approved the final version of each statement.
Statements
Uniform statements were addressed for each topic, with the aim of positioning all diagnostic procedures in a commonly agreed upon and evidence-based diagnostic flowchart. Each consensus statement is followed by comments derived from analysis of the relevant literature.
Literature search
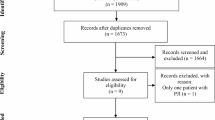
An extensive literature search of the PubMed/Medline and Scopus databases was conducted (for the period from 1 January 2000 up to December 2015) for each statement and for overall diagnostic accuracy of each diagnostic technique. Search terms were defined in agreement with all delegates from the four participating societies. Inclusion of the papers per statement was based on a PICO (Population/problem – Intervention/indicator – Comparator – Outcome) question to search for evidence after converting the PICO question into a search strategy. This strategy is described in detail by the Oxford Centre for Evidence-based Medicine (OCEBM) [15]. Case reports, reviews, and papers with fewer than 10 patients were excluded, as well as non-English-language papers. Systematic reviews were included. A cross-search with references included in the retrieved articles was also performed to look for further evidence. Based on expert experience, if some known paper was not retrieved by the search, it was added for competence.
Method for scoring the papers
All included papers per statement were thoroughly read and analysed, and a “level of evidence” was provided in consensus with all delegates for each paper according to the documents for levels of evidence provided by the OCEBM [16]. Finally, putting all levels of evidence for all included papers together, a final level of evidence was provided, again in agreement among all delegates, for each statement.
Current diagnostic approach for PJI
The diagnostic approach in patients with suspected PJI is extremely variable from centre to centre, depending on local experience, technological equipment, and adherence to available guidelines.
However, thus far there are no published “evidence-based” guidelines to guide the diagnostic flow of PJI. Clinical examination and laboratory tests, together with a planar x-ray film, are the first steps. These are followed by biopsies, or joint aspiration with microbiological analysis or advanced imaging modalities such as radiological and nuclear medicine examinations. These are explained in more detail in Appendix 1 [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47], and a statement on the concerns regarding the use of ionizing radiation is described in Appendix 2.
Consensus statements
All PICOs performed for the statements and the list of publications selected for the level of evidence are mentioned in Appendix 3.
1. PJI should be suspected when one or more of the following symptoms and signs are present: otherwise unexplained pain and/or fever, redness, swelling, scar inflammation, and movement limitations. These symptoms are (especially in the chronic phase) not specific and require other investigations.
Level of evidence: 4.
The main clinical signs of early PJI are persistent local pain, erythema, swelling, wound healing disturbance (leakage), and fever. In delayed and chronic infection occurring many years after prosthesis insertion, clinical signs may be absent; when present, they are represented by persistent or increasing joint pain and a loose prosthesis.
Symptoms are not specific for infection, and it is not easy to distinguish PJI from aseptic loosening by clinical history and physical examination alone. As a consequence, patients with one or more of the above-mentioned signs and symptoms should undergo further investigation for diagnosing or excluding the presence of infection [48,49,50,51,52,53,54].
2. Sinus tract and purulent discharge are clear signs of prosthetic joint infection.
Level of evidence: 5.
There are no papers published on this specific issue; rather, this is a general belief based on the logical assumption that, given the natural colonization of the skin, these bacteria will certainly colonize the exposed implant. However, no literature was found providing evidence that a sinus tract with purulent discharge is a sign of PJI. There is no evidence that microbiological analysis of tissue or fluid from sinus tracts is reliable for diagnosis.
3. CRP and ESR should always be performed in patients with suspected prosthetic joint infection. A normal value does not rule out PJI.
Level of evidence: 2.
Patients presenting with clinical signs of prosthetic joint infection (i.e. fever, unexplained pain at the site of arthroplasty, prosthetic loosening, or a sinus tract) should be subjected to screening for inflammatory markers in serum. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are good preliminary tests. Screening of these markers can be performed rapidly, inexpensively, and with minimal inconvenience. Although there is considerable variation in sensitivity (SE) and specificity (SP) for both CRP (SE 21–100%, SP 20–96%) and ESR (SE 58–97%, SP 33–90.9%), in general they show good diagnostic value, and are of relevance particularly for therapy follow-up. A threshold of 10 mg/l for CRP and 30 mm/h for ESR of is recommended for diagnostic purposes. One level 1 study and 32 level 2 studies addressed the diagnostic efficacy of CRP and ESR in serum [19, 55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82]. However, when testing for CRP and ESR, one should keep in mind that both markers can be influenced by numerous factors (i.e. neoplastic and inflammatory conditions, age, and technical details). Furthermore, CRP is produced in the liver, and especially in low-grade chronic PJI, levels may not be elevated. Therefore, a careful history and physical examination are mandatory. Several studies suggest using the combination of ESR and CRP [56, 59, 83]. In any case, if one of these markers is above the threshold, further diagnostic tests should be performed. Low CRP and ESR do not rule out PJI.
4. In the case of fever, blood cultures should always be performed in patients suspected of having prosthetic joint infection in order to identify the causative bacteria.
Level of evidence: 5.
Microorganisms may reach the prosthesis at the time of implantation or later by haematogenous spread [6, 7].
Haematogenous seeding can occur at any time after joint implantation. The main sources of bacteraemia are skin, respiratory tract, dental procedures, and urinary tract infection [7]. Haematogenous spread of S. aureus can also occur in patients without a detectable primary focus [84].
No studies specifically assessed the role of blood cultures in diagnosing PJI. However, in consideration of the frequent haematogenous origin of PJI, it is recommended that blood cultures be performed in patients with suspected PJI who have fever.
5. Conventional radiography is the first imaging modality to perform in patients with suspicion of PJI for diagnosis and follow-up.
Level of evidence: 2.
Conventional radiography is regularly used to evaluate joint prostheses after implantation and follow-up, as these procedures are able to detect any potential abnormality involving both the implant and the surrounding bone. For this reason, conventional radiography should always be performed. Regarding PJI, conventional radiography often yields normal results or may detect nonspecific signs of soft tissue swelling. Serial plain radiography has been reported to have sensitivity of 14% and specificity of 70% in detecting implant-associated infections. Radiographic signs that may reveal PJI with high specificity are gas formation and active, immature periostitis. Radiographic signs with low specificity include soft tissue swelling, periprosthetic lucency, and component loosening. However, differentiation between septic and aseptic periprosthetic lucency and component loosening is almost impossible on conventional radiography. Also, these signs are visible only when almost 30% of the bone mass has been lost; thus, 50% of radiographs remain normal despite the presence of infection [85,86,87].
6. Ultrasound can detect complications around the prosthesis, but the capacity for detecting infection is controversial.
Level of evidence: 2.
Van Holsbeeck et al. reported 100% sensitivity and 74% specificity for infection when the a capsule-to-bone distance was >4 mm, while 100% specificity was observed when the capsule-to-bone distance was >3.2 mm and extracapsular fluid was found in the hip [88]. These findings were questioned by Weybright et al. [89], who reported that anterior distension of the hip capsule was not predictive of infection.
7. Imaging may be useful for guiding joint aspiration or periprosthetic tissue biopsy.
Level of evidence: 2.
One of the challenges of correct aspiration or biopsy in and around the implant is placing the needle exactly in the area of interest. Open aspiration and biopsy can be done in a surgical theatre, but this approach is highly invasive. Fluoroscopy can be used as a guide, but it does not correctly show soft tissues and fluids, and it uses ionizing radiation. US can be used to guide the needle in the joint space and in the soft tissue around the implant without the use of ionizing radiation. Eisler et al. reported 7% sensitivity and 66% specificity for ultrasound-guided capsular biopsy, while fluid aspiration was always falsely sterile [90]. Battaglia et al. demonstrated 69% sensitivity, 94% specificity, and 83% accuracy for ultrasound-guided periprosthetic joint aspiration [91]. CT-guided aspiration has been reported to have 70% sensitivity, 100% specificity, and 84% accuracy for diagnosis of infection [92].
8. Leukocyte count and differential in synovial fluid has high diagnostic accuracy in detecting PJI.
Level of evidence: 2.
Patients with abnormal CRP and/or ESR should undergo aspiration of the hip or knee. We recommend that aspiration fluid be tested for white blood cell count (WBC) and percentage of neutrophils. Our systematic review of the literature showed high sensitivity and specificity for both tests. Synovial white blood cell count had sensitivity of 36–100% and specificity of 80–99%. Differential count had sensitivity of 84–100% and specificity of 80–99%. A threshold for white blood cell count of >3000 cells/μl seems justified based on the studies found (the thresholds from various reports vary from 1700 cells/μl to 5000 cells/μl). Neutrophil percentage > 70% is highly suggestive of prosthetic joint infection (range 65–80%). Fourteen level 2 studies addressed the diagnostic efficacy of synovial fluid white blood cell count and differential [19, 21, 52, 58, 60,61,62,63, 71, 76, 77, 80, 93, 94]. Aspiration of synovial fluid for white blood cell count has advantages. It can be performed in the outpatient setting, and the results do not appear to be influenced by antimicrobial treatment [94].
9. Bacterial culture from joint aspiration has high diagnostic accuracy in detecting prosthetic joint infection.
Level of evidence: 2.
Given the limitations of the preoperative diagnostic work-up in identifying the presence or absence of infection, fluid and tissue cultures of the suspected infection site are often necessary. Twenty-three level 2 studies in our systematic review showed moderate to high sensitivity (43.5–100%) and high specificity (81.2–100%) for cultures [19, 57, 60, 65, 75, 78, 80, 92, 95,96,97,98,99,100,101,102,103,104,105,106,107,108]. The culture of multiple intraoperative tissue samples is important for the differentiation of contamination from infection. Accordingly, we recommend using five tissue samples for microbial culture for both aerobic and anaerobic culturing. Cultures can reliably confirm the etiology of joint infection in cases where two or more tissue samples show growth of the same micro-organism. The incubation time should be at least 7 days, although some studies even advise an incubation time of 2 weeks [65, 72]. Cultures may be false-negative due to prior use of an antimicrobial agent, low number of organisms, use of an inappropriate culture medium, infection by a fastidious organism, or prolonged transport time to the microbiology laboratory. Therefore, it is advisable to stop antibiotic treatment at least 2 weeks before sampling.
10. Measurement of the synovial biomarkers alpha-defensin, leukocyte esterase, interleukin-6, and C-reactive protein is useful in the detection of prosthetic joint infection.
Level of evidence: 2.
In the last decade, numerous studies have addressed the evaluation of new biomarkers in synovial fluid. These biomarkers show promising results. In our systematic review, alpha-defensin showed very high sensitivity and specificity (95.5–100% and 95–100%, respectively) in three level 2 studies and two level 3 studies [62, 68, 109,110,111]. Alpha-defensin is produced locally in the joint and does not appear to be influenced by antibiotic treatment before diagnostic evaluation. However, this test is expensive and not yet available in every hospital. Some low-grade bacteria such as Cutibacterium acnes (formerly Propionibacterium acnes) are less likely to be demonstrated with alpha-defensin measurement. Another synovial biomarker, leukocyte esterase, has also demonstrated diagnostic value, with sensitivity of 66–100% and specificity of 77–100% in five level 2 studies [112,113,114,115,116]. Leukocyte esterase is tested on a colorimetric reagent pad. It has the advantages of simplicity and of providing real-time results. Nevertheless, the reagent strip cannot be adequately read in the presence of blood or other debris. IL-6 has shown better diagnostic performance in synovial fluid than in serum. Six level 2 studies demonstrated sensitivity of 62.5–97% and specificity of 85.7–100% [57, 66, 76, 111, 117, 118]. IL-6 promotes osteoclast activation, consequently leading to prosthetic loosening. The costs are fairly high, and this test is not available in every hospital. CRP can be measured in serum and in synovial fluid. Synovial CRP showed diagnostic value, with sensitivity of 70–97.3% and specificity of 78.6–100%, in eight level 2 studies [62, 77, 79, 81, 111, 118,119,120]. Routine laboratory equipment that assays serum CRP can be used for testing synovial CRP. Non-elevated CRP in synovial fluid does not rule out PJI, as CRP is produced in the liver and not in the joints. Care must be taken to take physical examination and history into account, because CRP is a nonspecific marker of acute inflammation.
11. Biopsy of periprosthetic tissue for histology and cultures can be performed for preoperative diagnosis in cases where ESR and/or CRP are positive and aspiration is inconclusive or impossible to test (dry tap).
Level of evidence: 2.
Biopsy is not advised in all cases, as it is an invasive diagnostic modality. Five papers showed high diagnostic value (sensitivity 79.1–100%, specificity 90–100%); therefore, biopsy can be used to rule in and rule out infection [66, 67, 81, 121, 122]. Knees are more easily biopsied than hips, as in the hip, only the neck and head of the prosthesis and the inlay of the acetabular cup are easily accessible. Moreover, biopsy is associated with risk of infection and vascular or nerve injury. Using the blind technique could cause damage such as scratches to the articulating prosthetic surface. Culturing of biopsied periprosthetic tissue can identify the causative microorganism, and as a result, the correct antimicrobial treatment and adequate bone cement for the arthroplasty can be chosen.
12. Antibiotic therapy should be postponed or discontinued before pre- and intraoperative sampling.
Level of evidence: 4.
In clinical practice, the dictum that antibiotics should be withheld before obtaining microbiological cultures is well recognised. Some studies have confirmed the impact of previous antibiotic therapy on the probability of obtaining a microbiological diagnosis of PJI.
In a prospective trial in 79 patients with PJI, culture of samples obtained by sonication of the explanted prostheses were compared with conventional culture of periprosthetic tissue for the microbiological diagnosis of prosthetic joint infection. The sensitivity of the tissue cultures decreased (from 77% to 48% to 41%) as the antimicrobial-free interval before surgery decreased (from more than 14 days, to 4–14 days, and to 0–3 days, respectively) [20]. This was confirmed in another study, in which the sensitivity of periprosthetic tissue and synovial fluid culture increased from 54% to 73% when the patients who had received antimicrobial agents were excluded [93].
Another study found a statistically significant difference in the rate of positivity of biopsy specimen bacterial cultures between patients exposed and not exposed to previous antibiotic therapy [123].
Similarly, some studies reported higher sensitivity of synovial fluid culture in patients who did not take antibiotics before the procedure as compared with patients exposed to antibiotics [93, 124].
13. Antibiotic therapy should not be discontinued before white blood cell scintigraphy.
Level of evidence: 4.
The issue of whether on-going antibiotic treatment may interfere with the diagnostic accuracy of WBC scintigraphy has been widely disputed, yet there are no clinical comparative studies in patients with and without antibiotic treatment. Therefore, this information can only be extrapolated indirectly from studies that have included patients at diagnosis treated with antibiotics or from studies in patients during follow-up of therapy. Indeed, there are a number of studies of this kind in osteomyelitis (including peripheral bone osteomyelitis, prosthetic joint infection, and diabetic foot osteomyelitis) [125,126,127,128,129,130,131], soft tissue infections [132,133,134,135,136], inflammatory bowel diseases [137, 138], and cardiovascular infection [139, 140]. If taken together, approximately half of them conclude that antibiotic treatment reduces diagnostic accuracy [131, 135, 136, 138], and the other half report that it does not [125,126,127,128,129,130, 132, 137, 139]. This is based on the pooled sensitivity and specificity that seems to be reduced or unaffected with respect to patients at diagnosis without antibiotic therapy. Nevertheless, if we look only at only those papers in which the final diagnosis was made by histological evaluation of bone biopsy, we may conclude that WBC scintigraphy has the same diagnostic accuracy either before or during antibiotic treatment. This is particularly convincing for the diabetic foot infection [129, 130] and less convincing for prosthetic joint infections, mainly because of the results obtained by Chik et al. [131].
In summary, there is not sufficient evidence in the literature to reach a definitive conclusion on the impact of antibiotic treatment on the accuracy of WBC scintigraphy in PJI.
14. Computed tomography can be effectively used to diagnose PJI.
Level of evidence: 2.
Computed tomography has traditionally been used to evaluate orthopaedic implants. Striking artefacts caused by the interaction of the x-ray beam with the metallic hardware are now markedly reduced thanks to recent technical improvements. On CT, joint distension, fluid-filled bursae, and soft tissue collections are the main findings. Cyteval et al. reported that CT demonstrated 100% sensitivity, 87% specificity, and 89% accuracy when at least one soft tissue abnormality was used as an infection criterion, and 83% sensitivity, 96% specificity, and 94% accuracy when joint distention was used as infection criterion [141]. Absence of joint distension had 96% negative predictive value. Fluid collection in muscles and peri-muscular fat demonstrated 100% positive predictive value. Periosteal new bone has shown high specificity (100%) but low sensitivity (16%) for infection. Bone lucency around the implant is not a criterion for diagnosing infection, although in infected patients, CT may demonstrate a “more aggressive, ill-defined” lucency [142, 143]. Detection of a sinus tract may be difficult on CT.
15. The diagnostic accuracy for three-phase bone scintigraphy in patients with suspected infection within the first 2 years after hip or knee prosthesis placement is low.
Level of evidence: 2.
Three-phase bone scintigraphy is the most widely used screening modality for the diagnosis of PJI. However, it is common knowledge that the technique is highly sensitive but has low specificity for PJI, since any cause of increased bone formation (e.g. physiological bone remodelling or aseptic prosthetic loosening) shows increased periprosthetic activity on the bone scan. This physiological bone remodelling probably takes place in the first years after joint replacement surgery and is also dependent on the type of prosthesis and whether the prosthesis was cemented or uncemented.
The results of our search yielded 89 papers, of which 14 were included. After reading these papers thoroughly, we included only five papers that investigated the role of three phases in bone scan after joint replacement [144,145,146,147,148], four of which were reviews/overviews/expert opinions, and only one paper [144] reported the exact time between first surgery and bone scan (median duration 21 months in 39 patients after a unicompartmental knee replacement [UKR]). The authors found sensitivity of 50% and specificity of 71% for infection and concluded that there is no evidence to support the routine use of bone scan in clinical decision-making for patients with a painful UKR.
Experts agree that the diagnostic accuracy for three-phase bone scan in patients with suspected infections within the 5 years after hip or knee prosthesis placement is low. Van der Bruggen et al. [43] mention that in post-traumatic patients and after surgery, specificity is extremely low, around 35%. During this period, it is better to immediately perform another imaging technique, preferably white blood cell scintigraphy.
16. In the case of negative three-phase bone scintigraphy, a diagnosis of prosthetic joint infection can be excluded.
Level of evidence: 2.
Bone scintigraphy is widely used as first imaging modality when there is suspicion of a low-grade PJI. All three phases (perfusion, blood pool, and late phase depicting the osteoblastic activity) are necessary when an infection is suspected. Although a positive bone scan can be the result of any cause of increased osteoblast activity, a negative bone scan in all three phases means that there is no increased perfusion and no increased osteoblastic activity. It has been stated, therefore, that a negative three-phase bone scan rules out a diagnosis of PJI.
We conducted a literature search and 76 papers were retrieved, of which 15 were eventually included for thorough reading.
Only four research studies focused on the negative predictive value of the three-phase bone scan. Ikeuchi et al. [149] investigated the role of the bone scan in 15 patients after joint arthroplasty. They concluded that when the three-phase bone scan is negative, residual infection around the cement spacer is unlikely. Nagoya et al. [150] concluded that a negative three-phase bone scan suggests a low probability of periprosthetic infection and that one-stage revision could be considered in these cases. Volpe et al. [151] showed that a diagnostic algorithm using bone scan as a first screening modality had high diagnostic accuracy. Unfortunately, only seven patients had a negative bone scan, and timing between primary surgery and scans was not mentioned. Trevail et al. [152] investigated an imaging algorithm in 235 consecutive patients, of which only 17 were ultimately diagnosed with a proven infection. The authors also initially performed a bone scan. If the bone scan was negative, then infection was excluded and no WBC scan was performed. Using this algorithm, they found sensitivity of 80% and specificity of 99.5%. They did not mention, however, how many patients had a negative bone scan and in how many patients a WBC scan was performed.
Other included papers (overviews, reviews, and expert opinion) are in agreement that a study with normal findings (no increased perfusion or blood pool, no periprosthetic uptake in the late phase) can be considered strong evidence against the presence of an infection [146, 153,154,155,156].
17. In the case of a positive three-phase bone scan, the addition of white blood cell scintigraphy leads to high diagnostic accuracy for PJI.
Level of evidence: 2.
A positive three-phase bone scintigraphy can have several causes, including PJI, physiological bone remodelling, or aseptic loosening of the prosthesis. Therefore, other investigations must be performed to further differentiate between infection, reactive changes, and loosening. To determine whether WBC scintigraphy, when added to the diagnostic flowchart of a positive three-phase bone scintigraphy, leads to higher diagnostic accuracy, we conducted a PubMed search with the following terms: “(prosthetic OR prosthesis OR joint infection)) AND (bone scan OR MDP OR HDP OR bone scintigraphy)) AND (WBC scan OR WBC scintigraphy OR white blood cell scan OR white blood cell scintigraphy OR leukocyte scintigraphy)) AND diagnosis of infection”; 44 papers were retrieved, of which 19 were eventually included for thorough reading.
Only two research papers were found that specifically studied whether the addition of WBC scintigraphy after a positive bone scan leads to high diagnostic accuracy. Volpe et al. [149] showed that a diagnostic algorithm using the bone scan as first screening modality, and, when positive, the LeukoScan, achieved high diagnostic accuracy. Unfortunately, only seven patients had a negative bone scan, and timing between surgery and scans was not mentioned. Trevail et al. [152] also investigated an imaging algorithm in 235 consecutive patients, of which only 17 were ultimately diagnosed with a proven infection. The authors also performed an initial bone scan, which, if positive, was followed with a WBC scan. The use of this algorithm led to sensitivity of 80% and high specificity of 99.5%. Not mentioned, however, was how many patients had a negative bone scan and in how many patients a WBC scan was performed.
We also agree that another imaging modality is necessary in the case of a positive three-phase bone scan in patients with suspected PJI [3, 43, 157,158,159,160], and that WBC scintigraphy is the first nuclear imaging modality of choice in these cases because of its high diagnostic accuracy.
18. In the case of negative white blood cell scintigraphy, the probability of prosthetic joint infection is low.
Level of evidence: 2.
WBC scintigraphy has been described by many authors as highly sensitive and very specific for the diagnosis of PJI. However, there is still some concern whether low-grade chronic PJI with small amounts of bacteria on the biofilm can lead to false-negative WBC scan results.
We conducted a literature search to look at the diagnostic accuracy of WBC scintigraphy in patients with suspected PJI, and we retrieved 97 papers, of which 20 were eventually included for thorough reading and 12 after thorough reading.
The largest patient series included is from Kim et al. [161], who found NPV of 92% in 164 patients with suspected PJI (71 hip, 93 knee). Glaudemans et al. [154] used a time-decay dual-time-point imaging protocol and found NPV of 94% in 67 patients with suspected hip prosthesis infection, and NPV of 96% in 71 patients with suspected knee prosthesis infection. The same protocol was used by Erba et al. [162]. They report NPV of 93% in both hip and knee prostheses in 44 and 40 patients, respectively. Older studies used other protocols, including WBC labelled with 111In or anti-granulocyte imaging, or a combination of WBC/bone marrow (BM) scintigraphy.
Sousa et al. [163] report NPV NPV of 100% using sulesomab. Jung et al. [164] found NPV of 100%, but this was in only 11 patients and using a combined imaging protocol (WBC/BM). Simonsen et al. used both 99mTc- and 111In-labelled WBC, and found 94% true-negative results [165]. Only Basu et al. found lower NPV (85% in patients with suspected hip prosthesis infection), but they used an incorrect acquisition protocol with only one imaging time point between 18 and 24 h after re-injection [166]. In conclusion, expert opinions and most research studies indicate high negative predictive value for WBC scintigraphy, which is even higher when performed with the correct acquisition protocol and interpretation criteria.
19. 18 F-FDG-PET in patients with suspected prosthetic joint infection has high sensitivity but lower specificity than white blood cell scintigraphy or anti-granulocyte antibody scintigraphy.
Level of evidence: 2.
A PubMed search based on the above-listed MeSH terms revealed 15 papers, of which five (three original research articles and two systematic reviews) were selected for thorough reading. In addition, four papers on the diagnostic performance of WBC scintigraphy in prosthetic joint infections were added.
There are few articles directly comparing the diagnostic performance of FDG-PET and WBC scintigraphy. The study by Love et al. [34] reported significantly higher accuracy for combined bone marrow and WBC scintigraphy than for FDG-PET, independent of the interpretation criteria used for FDG-PET. Vanquickenborne et al. [167] reported similar sensitivity between WBC scintigraphy and FDG-PET (88%), but higher specificity for WBC scan compared with FDG-PET (100% vs. 78%). The study by Pill et al. [168] reported sensitivity and specificity of 95% and 93%, respectively, for FDG-PET, while the use of combined 99mTc-sulfur colloid- and 111In-labelled WBC demonstrated sensitivity of 50% and specificity of 95%.
Reinartz et al. [32], in a systematic review, reported higher sensitivity but lower specificity for FDG-PET compared with WBC scintigraphy. In addition, the accuracy for FDG-PET was found to be slightly higher in hip prosthesis than in knee prosthesis. In another review article, Gemmel et al. reported pooled sensitivity and specificity of 84% for FDG-PET in PJI, with higher accuracy for hip than knee prosthesis [31]. The joint EANM/SNMMI guidelines for the use of FDG in inflammation and infection (expert opinion) reported overall sensitivity of 95% for FDG-PET and specificity of 98% for knee and hip PJI [160].
In all mentioned systematic reviews, the range for both sensitivity (28–91%) and specificity (34–97%) in the individual studies was quite large. This is largely attributable to the differences in study design and interpretation criteria (visual interpretation using pattern recognition), emphasizing the need for standardized reconstruction and interpretation criteria.
Although there are not many published papers that directly compare FDG-PET and WBC scintigraphy in prosthetic joint infections, several different interpretation criteria for FDG-PET have been tested, and all papers confirm the lower specificity of FDG-PET compared with WBC scintigraphy. Large prospective studies comparing the diagnostic performance of WBC scintigraphy and FDG-PET for prosthetic joint infections are anticipated.
20. Anti-granulocyte scintigraphy is a good alternative to white blood cell scintigraphy, with similar sensitivity and specificity (mentions human anti-mouse antibodies [HAMA], differences between Fab and IgG, repeatability, which one to use in function of pretest probability, etc.).
Level of evidence: 2.
An extensive PICO was performed using a combination of different terms, but no papers were found that directly compared the diagnostic accuracy of labelled white blood cells with anti-granulocyte antibodies for patients with suspicion of prosthetic joint infections. A direct comparison between 99mTc-besilesomab- and 99mTc-labelled white blood cells in peripheral osteomyelitis, including patients with PJI, was published by Richter et al. [169], with comparable results for the two imaging approaches [163, 170].
Two meta-analyses on the diagnostic performance of anti-granulocyte antibodies in prosthetic joint infections were performed by Pakos et al. [171] and Xing et al. [172], and revealed overall sensitivity of 83% and specificity of 79–80%. These results are comparable to radiolabelled white blood cells, with slightly lower specificity for antibodies. Considering the results of these meta-analyses, the use of anti-granulocyte antibodies can be regarded as a valid alternative in patients with suspicion of prosthetic joint infections.
21. Hybrid SPECT/CT imaging can improve localization of infection (and diagnostic accuracy).
Level of evidence: 2.
Since the introduction of hybrid imaging technologies in clinical practice, the diagnostic accuracy of conventional nuclear exams has drastically improved due to the complementary molecular/functional and morphological information. Even though current recommendations for interpreting white blood cell scintigraphy are based solely on planar images at consecutive time points, adding SPECT/CT in the case of a positive result would theoretically further increase the diagnostic accuracy. It is well established for other pathologies that adding SPECT/CT to planar images results in higher diagnostic accuracy because of better resolution and morphological information.
A PubMed search yielded 50 papers, of which five papers (three original research articles [161, 173, 174] and two systematic reviews [31, 175]) were included. Two small studies [173, 174] showed increased specificity for SPECT/CT compared with SPECT alone and demonstrated contributory value in up to 38%. The largest study, by Kim et al., also demonstrated improved diagnostic accuracy with the addition of SPECT/CT [161].
Despite limited published data on white blood cell SPECT/CT in patients with suspicion of prosthetic joint infections, the incremental value of SPECT/CT over planar imaging is obvious. Adding SPECT/CT increases diagnostic accuracy by better distinguishing bone infection from soft tissue infections through improved assessment of the extent of the infection. Therefore, SPECT/CT should be recommended in the case of a positive planar white blood cell scan.
22. Semiquantitative analysis of WBC accumulation over time in WBC scan increases diagnostic accuracy for PJI.
Level of evidence: 3.
Based on the assumption that radiolabelled WBC, once injected into the patient, will migrate over time to an infected area and will progressively accumulate there due to the presence of chemotactic factors, nuclear medicine physicians have thought to quantify the presence of WBC in suspected lesions at 3–4 h after injection and again at 20–24 h. This quantitation is expressed as a ratio between radioactivity in the suspected region (target) and radioactivity in a background area. If this target-to-background (T/B) ratio increases over time (i.e. T/B20h > T/B4h), there is active WBC accumulation, which is interpreted as an infection. By contrast, if the ratio decreases over time (i.e. T/B20h < T/B4h), there is only transient WBC accumulation in the lesion, and it is interpreted as a sterile inflammatory process. Only two works have systematically investigated these assumptions, however, in retrospective studies, using the histological/microbiological information or long-term clinical follow-up of patients as gold standard [154, 176]. Both studies demonstrated a clear improvement in diagnostic accuracy for the semiquantitative method over simple qualitative image evaluation, particularly if the calculation of the T/B ratio was performed in both delayed images (3-4 h) and late images (20-24 h), and if the contralateral tissue was used as background instead of the ipsilateral bone marrow or ipsilateral iliac bone (often not available in the case of knee prosthesis). Glaudemans et al. showed that the T/B should show an increase of at least 10% to be considered a reliable indicator of granulocyte accumulation over time [154].
Other studies have applied a similar semiquantitative method, not only for prosthesis infection but also for soft tissue infection [161], post-traumatic osteomyelitis [176], and diabetic foot infection [35], or even with other radiopharmaceuticals such as FDG [34, 35, 177]. All studies were in agreement on the usefulness of semiquantitative evaluation of WBC accumulation in infected lesions over time. In particular, Van Acker et al. [178] emphasized that when only a qualitative approach is used, there is no benefit regardless of whether the analysis is done with or without a grading. It is worth mentioning that a study by Glaudemans et al. in a large number of patients demonstrated that semiquantitative analysis of the T/B ratio was particularly useful in those cases with a doubtful qualitative interpretation [154].
23. Combining WBC scan with bone marrow scan increases diagnostic accuracy for PJI detection.
Level of evidence: 2.
The use of combined WBC scintigraphy (using either 99mTc-HMPAO-WBC or 111In-oxine-WBC) and bone marrow scintigraphy (with radiolabelled colloids) has been studied by many authors. This technique allows us to reduce the number of false-positive cases at WBC scintigraphy due to WBC accumulation in areas of expanded/displaced bone marrow by providing a map of bone marrow activity. It is particularly useful in cases of suspected PJI and in patients with a doubtful qualitative or semiquantitative analysis of WBC scintigraphy.
With few exceptions, the cumulative results obtained from papers describing this combined technique are remarkably consistent, with reported diagnostic accuracy ranging from 83% to 98% for both 111In-oxine-WBC and 99mTc-HMPAO-WBC and for both hip and knee prosthesis infections [31, 34, 155, 165, 179,180,181,182,183]. Pill et al. in 2006 [168] and Joseph et al. in 2001 [184] reported low sensitivity (50% and 46%, respectively) but very high specificity (95% and 100%, respectively). The reason for the low sensitivity in these studies was that most of the examined infections were subacute or chronic, and/or microbiological data were often lacking. Given these few exceptions, it appears that combined in vitro labelled leucocyte/bone marrow scintigraphy (LS/BMS) has overall diagnostic accuracy of >90% and is the imaging modality of choice for diagnosing PJI.
Most importantly, the acquisition protocol and the interpretation criteria for WBC scintigraphy differed dramatically in the reported studies, thus emphasizing the importance of the combined LS/BMS technique.
Today, standardized acquisition and interpretation criteria are being disseminated and utilised across Europe, thus further reducing inter-observer variability and increasing the diagnostic accuracy and reproducibility of WBS scintigraphy. This will certainly help to reduce the number of doubtful cases in which to apply additional BMS scintigraphy.
24. MRI is wholly feasible in patients with suspected PJI.
Level of evidence: 2.
The presence of a joint prosthesis does not represent a contraindication to MRI. Traditionally, joint implants were considered potentially limiting to the outcome of an MR examination, due to a high quantity of susceptibility artefacts that could be generated by the metal itself. More recently, the advent of prostheses made with less ferromagnetic alloy materials and the technological advancements in MR sequences (metal artefact reduction sequences [MARS], slice encoding for metal artefact correction [SEMAC], and multi-acquisition with variable-resonance image combination [MAVRIC]) have made MRI wholly feasible in patients with joint implants, with artefacts largely confined to the area of the implant itself [185,186,187]. The diagnostic performance of MRI in PJI is addressed in statement 25.
25. MRI demonstrates high diagnostic performance in detecting clinically suspected PJI, with no ionizing radiation.
Level of evidence: 2.
Despite the widespread use of this protocol in clinical practice, most papers on MRI and joint prosthesis were focused on the technical feasibility of this examination. Only three papers specifically aimed to evaluate prosthesis infection. In the knee, Plodowski et al. found 86–92% sensitivity and 85–87% specificity for infection, while Li et al. found 65–78% sensitivity and 98–99% specificity. In the hip, He et al. found 94% sensitivity and 97% specificity. Like ultrasound, MRI is an imaging modality that does not use ionizing radiation. This fact should be given particular consideration, especially in these patients, who typically need repeated examinations [44,45,46,47].
Conclusions and final recommendations
The proposed flowchart is shown in Fig. 1. Regarding the advanced diagnostic tests, there are too few well-designed papers (with a high level of evidence) that directly compare radiological and nuclear medicine techniques. When choosing an advanced diagnostic test, further stratification should be performed based on the pretest probability of infection and local availability and experience. Overall, considering the diagnostic performance of all modalities, both WBC scan (with or without bone marrow scan) or anti-granulocyte scintigraphy (preferably with IgG) and non-contrast MRI can be performed as an initial investigation (Fig. 2).
The suggested initial diagnostic steps to undertake in the case of suspicion of a PJI, based on published evidence. Some tests can be repeated (i.e. blood cultures, bone biopsies, or soft tissue biopsies). Serological tests (CRP, WBC count with differential, and ESR) should be performed over time, since the overall increasing or decreasing trend is more important than a single value. The choice of an advanced diagnostic test depends on availability, costs, radiation burden, and operator experience (see Tables 1 and 2). Synovial biomarkers and cultures can be better performed after sonication of tissue samples. They have high accuracy for infection but need to be integrated with advanced imaging modalities to study the bone and soft tissue status and the extent and severity of the infection
The suggested path to undertake when nuclear medicine procedures are considered for suspicion of a PJI, based on published evidence and expert opinion. Initial stratification is based on time after implant (more or less than 2 years). This is particularly true for hip and shoulder prostheses, but knee prosthesis may require up to 5 years post-implant to reduce physiological inflammation. Some differences may also depend on the type of prosthesis (cemented or not), with cemented prostheses having a shorter post-implant time for physiological inflammatory reaction. 1FDG-PET has higher sensitivity than specificity, mainly because of false-positive inflammatory uptake in the case of aseptic loosening and/or recent surgery. This is why it is better to exclude an infective process in chronic painful joints. Nevertheless, despite the lack of standardized image interpretation criteria available, FDG-PET has also been proposed in early acute phases of infections. 2WBC scan has higher sensitivity and specificity than AGA scan, FDG-PET, and MRI, and is preferred when available and indicated for the patient. The methodology for these nuclear medicine scans is extremely important (usually by acquiring three sets of images corrected for isotope decay), and we refer to the procedural guidelines published by the EANM Committee on Infection/Inflammation. It can be combined with bone marrow scintigraphy to further increase specificity
Evidence-based diagnostic flow charts
Based on the above-mentioned statements and evidence from the published literature, we have developed a diagnostic flow chart, shown in Fig. 1, correlated with Tables 1 and 2.
In some cases, the flow was integrated by consensus opinion amongst the experts, since not all steps are always clearly deducible from the literature or from level 1–2 articles. The flow chart does not take into consideration socioeconomic factors or the availability of diagnostic methods. It also presumes that all exams are optimally performed (possibly following procedural guidelines published by each European or national society, when available) and by expert professionals.
Change history
09 February 2019
The authors regret to inform the readers that one of the author’s name in the original publication of this article was spelled incorrectly as Victor Casar-Pullicino. The correct spelling is Victor N. Cassar-Pullicino and is now presented correctly in this article.
Abbreviations
- PJI:
-
Prosthetic joint infection
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- WBC:
-
White blood cells
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- PICO:
-
Population/problem – Intervention/indicator – Comparator – Outcome
- CT:
-
Computed tomography
- EANM:
-
European Association of Nuclear Medicine
- ESR:
-
European Society of Radiology
- EBJIS:
-
European Bone and Joint Infection Society
- ESCMID:
-
European Society of Clinical Microbiology and Infectious Diseases
- OCEBM:
-
Oxford Centre for Evidence-based Medicine
- MRI:
-
Magnetic resonance imaging
- FDG:
-
Fluor-deoxy-glucose
- Tc:
-
Technetium
- PET:
-
Positron emission tomography
- AGA:
-
Anti-granulocyte antibodies
- mAbs:
-
Monoclonal antibodies
- SPECT:
-
Single-photon emission computed tomography
- US:
-
Ultrasound
- HDP:
-
Hydroxymethylene diphosphonate
- MDP:
-
Methylene diphosphonate
- HMPAO:
-
Hexamethylpropyleneamine oxime
- T/B:
-
Target-to-background ratio
- Oxine:
-
8-hydroxyquinoline
- MARS:
-
Metal artefact reduction sequences
- MAVRIC:
-
Multi-acquisition variable-resonance image combination
- SEMAC:
-
Slice encoding for metal artefact correction
References
Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–97.
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplast. 2012;27:61–5.
Glaudemans AW, Galli F, Pacilio M, Signore A. Leukocyte and bacteria imaging in prosthetic joint infection. Eur Cell Mater. 2013;25:61–77.
Cataldo MA, Petrosillo N, Cipriani M, Cauda R, Tacconelli E. Prosthetic joint infection: recent developments in diagnosis and management. J Inf Secur. 2010;61:443–8.
Trampuz A, Zimmerli W. Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly. 2005;135(17–18):243–51.
Berbari EF, Hanssen AD, Duffy MC, Steckelberg JM, Ilstrup DM, Harmsen WS, et al. Risk factors for prosthetic joint infection: case-control study. Clin Infect Dis. 1998;27(5):1247–54.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645–54.
Moran E, Masters S, Berendt AR, McLardy-Smith P, Byren I, Atkins BL. Guiding empirical antibiotic therapy in orthopaedics: the microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Inf Secur. 2007;55(1):1–7.
Hsieh PH, Lee MS, Hsu KY, Chang YH, Shih HN, Ueng SW. Gram-negative prosthetic joint infections: risk factors and outcome of treatment. Clin Infect Dis. 2009;49(7):1036–43.
Legout L, Senneville E, Stern R, Yazdanpanah Y, Savage C, Roussel-Delvalez M, et al. Treatment of bone and joint infections caused by gram-negative bacilli with a cefepime-fluoroquinolone combination. Clin Microbiol Infect. 2006;12(10):1030–3.
Sia IG, Berbari EF, Karchmer AW. Prosthetic joint infections. Infect Dis Clin N Am. 2005;19(4):885–914.
Berbari EF, Marculescu C, Sia I, Lahr BD, Hanssen AD, Steckelberg JM, et al. Culture-negative prosthetic joint infection. Clin Infect Dis. 2007;45(9):1113–9.
Marculescu CE, Berbari EF, Cockerill FR 3rd, Osmon DR. Fungi, mycobacteria, zoonotic and other organisms in prosthetic joint infection. Clin Orthop Relat Res. 2006;451:64–72.
Jutte P, Lazzeri E, Sconfienza LM, Cassar-Pullicino V, Trampuz A, Petrosillo N, et al. Diagnostic flowcharts in osteomyelitis, spondylodiscitis and prosthetic joint infection. Q J Nucl Med Mol Imaging. 2014;58:2–19.
Howick J, Chalmers I, Glasziou P, GreenhalghT, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H. The 2011 Oxford CEBM levels of evidence (introductory document). Oxford Centre for Evidence-Based Medicine. 2011.
OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. www.cebm.net/index.aspx?0=5653. website. 2016.
Trampuz A, Steckelberg JM, Osmon DR, Cockerill FR, Hanssen AD, Patel R. Advances in the laboratory diagnosis of prosthetic joint infection. Rev Med Microbiol. 2003;14:1–14.
Pandey R, Berendt AR, Athanasou NA. Histological and microbiological findings in non-infected and infected revision arthroplasty tissues. The OSIRIS collaborative study group. Oxford Skeletal Infection Research and Intervention Service. Arch Orthop Trauma Surg. 2000;120(10):570–4.
Spangehl MJ, Masri BA, O’Connell JX, Duncan CP. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg. 1999;81(5):672–83.
Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, et al. Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med. 2007;357(7):654–63.
Trampuz A, Zimmerli W. Diagnosis and treatment of implant-associated septic arthritis and osteomyelitis. Curr Infect Dis Rep. 2008;10(5):394–403.
Klauser AS, Tagliafico A, Allen GM, Boutry N, Campbell R, Grainger A, et al. Clinical indications for musculoskeletal ultrasound: a Delphi-based consensus paper of the European Society of Musculoskeletal Radiology. Eur Radiol. 2012;22(5):1140–8.
Lee YH, Lim D, Kim E, Kim S, Song H-T, Suh J-S. Usefulness of slice encoding for metal artifact correction (SEMAC) for reducing metallic artifacts in 3-T MRI. Magn Reson Imaging. 2013;31(5):703–6.
Li AE, Sneag D, Greditzer HG 4th, Johnson CC, Miller TT, Potter HG. Total knee arthroplasty: diagnostic accuracy of patterns of synovitis at MR imaging. Radiology. 2016;27:152828.
Plodkowski AJ, Hayter CL, Miller TT, Nguyen JT, Potter HG. Lamellated hyperintense synovitis: potential MR imaging sign of an infected knee arthroplasty. Radiology. 2013;266(1):256–60. https://doi.org/10.1148/radiol.12120042.
Van den Wyngaert T, Strobel K, Kampen WU, Kuwert T, van der Bruggen W, Mohan HK, et al. The EANM practice guidelines for bone scintigraphy. Eur J Nucl Med Mol Imaging. 2016;43(9):1723–38. https://doi.org/10.1007/s00259-016-3415-4.
De Vries EF, Roca M, Jamar F, Israel O, Signore A. Guidelines for the labelling of leucocytes with (99m)Tc-HMPAO. Inflammation/infection Taskgroup of the European association of Nuclear Medicine. Eur J Nucl Med Mol Imaging. 2010;37:842.
Roca M, EFJ DV, Jamar F, Israel O, Signore A. Guidelines for the labelling of leucocytes with 111In-oxine. Eur J Nuclear Med Molec Imag. 2010;37(4):835–41 Erratum to: (2010) European Journal of Nuclear Medicine and Molecular Imaging, 37 (6), p. 1236.
Gratz S, Reize P, Kemke B, Kampen WU, Luster M, Höffken H. Targeting osteomyelitis with complete [99mTc]besilesomab and fragmented [99mTc]sulesomab antibodies: kinetic evaluations. Q J Nucl Med Mol Imaging. 2016;60(4):413–23.
Jin H, Yuan L, Li C, Kan Y, Hao R, Yang J. Diagnostic performance of FDG PET or PET/CT in prosthetic infection after arthroplasty: a meta-analysis. Q J Nucl Med Mol Imaging. 2014;58:85–93.
Gemmel F, Van den Wyngaert H, Love C, Welling MM, Gemmel P, Palestro CJ. Prosthetic joint infections: radionuclide state-of-the-art imaging. Eur J Nucl Med Mol Imaging. 2012;39(5):892–909.
Reinartz P. FDG-PET in patients with painful hip and knee arthroplasty: technical breakthrough or just more of the same. Q J Nucl Med Mol Imaging. 2009;53(1):41–50.
Chacko TK, Zhuang H, Stevenson K, Moussavian B, Alavi A. The importance of the location of fluorodeoxyglucose uptake in periprosthetic infection in painful hip prostheses. Nucl Med Commun. 2002;23(9):851–5.
Love C, Marwin SE, Tomas MB, Krauss ES, Tronco GG, Bhargava KK, et al. Diagnosing infection in the failed joint replacement: a comparison of coincidence detection 18F-FDG and 111In-labeled leukocyte/99mTc-sulfur colloid marrow imaging. J Nucl Med. 2004;45(11):1864–71.
Familiari D, Glaudemans AW, Vitale V, Prosperi D, Bagni O, Lenza A, et al. Can sequential 18F-FDG PET/CT replace WBC imaging in the diabetic foot? J Nucl Med. 2011;52(7):1012–9.
Stumpe KD, Nötzli HP, Zanetti M, Kamel EM, Hany TF, Görres GW, et al. FDG PET for differentiation of infection and aseptic loosening in total hip replacements: comparison with conventional radiography and three-phase bone scintigraphy. Radiology. 2004;231(2):333–41.
Wenter V, Müller JP, Albert NL, Lehner S, Fendler WP, Bartenstein P, et al. The diagnostic value of [(18)F]FDG PET for the detection of chronic osteomyelitis and implant-associated infection. Eur J Nucl Med Mol Imaging. 2016;43(4):749–61.
Thang SP, Tong AK, Lam WW, Ng DC. SPECT/CT in musculoskeletal infections. Semin Musculoskelet Radiol. 2014;18(2):194–202.
Tam HH, Bhaludin B, Rahman F, Weller A, Ejindu V, Parthipun A. SPECT-CT in total hip arthroplasty. Clin Radiol. 2014;69(1):82–95.
Mariani G, Bruselli L, Kuwert T, Kim EE, Flotats A, Israel O, et al. A review on the clinical uses of SPECT/CT. Eur J Nucl Med Mol Imaging. 2010;37(10):1959–85.
Scharf S. SPECT/CT imaging in general orthopedic practice. Semin Nucl Med. 2009;39(5):293–307.
Israel O, Keidar Z. PET/CT imaging in infectious conditions. Ann N Y Acad Sci. 2011;1228:150–66.
van der Bruggen W, Bleeker-Rovers CP, Boerman OC, Gotthardt M, Oyen WJ. PET and SPECT in osteomyelitis and prosthetic bone and joint infections: a systematic review. Semin Nucl Med. 2010;40(1):3–15.
Aliprandi A, Sconfienza LM, Randelli P, Bandirali M, Tritella S, Di Leo G, et al. Magnetic resonance imaging of the knee after medial unicompartmental arthroplasty. Eur J Radiol. 2011;80(3):e416–21.
White LM, Kim JK, Mehta M, Merchant N, Schweitzer ME, Morrison WB, et al. Complications of total hip arthroplasty: MR imaging-initial experience. Radiology. 2000;215(1):254–62.
Hayter CL, Koff MF, Shah P, Koch KM, Miller TT, Potter HG. MRI after arthroplasty: comparison of MAVRIC and conventional fast spin-echo techniques. AJR Am J Roentgenol. 2011;197(3):W405–11.
He C, Lu Y, Jiang M, Feng J, Wang Y, Liu Z. Clinical value of optimized magnetic resonance imaging for evaluation of patients with painful hip arthroplasty. Chin Med J. 2014;127(22):3876–80.
Gille J, Ince A, González O, Katzer A, Loehr JF. Single-stage revision of peri-prosthetic infection following total elbow replacement. J Bone Joint Surg Br. 2006;88(10):1341–6.
Achermann Y, Stasch P, Preiss S, Lucke K, Vogt M. Characteristics and treatment outcomes of 69 cases with early prosthetic joint infections of the hip and knee. Infection. 2014;42(3):511–9.
Garcia RM, Hardy BT, Kraay MJ, Goldberg VM. Revision total knee arthroplasty for aseptic and septic causes in patients with rheumatoid arthritis. Clin Orthop Relat Res. 2010;468(1):82–9.
Magnuson JE, Brown ML, Hauser MF, Berquist TH, Fitzgerald RH Jr, Klee GG. In-111-labeled leukocyte scintigraphy in suspected orthopedic prosthesis infection: comparison with other imaging modalities. Radiology. 1988;168(1):235–9.
Virolainen P, Lahteenmaki H, Hiltunen A, Sipola E, Meurman O, Nelimarkka O. The reliability of diagnosis of infection during revision arthroplasties. Scand J Surg. 2002;91(2):178–81.
Teller RE, Christie MJ, Martin W, Nance EP, Haas DW. Sequential indium labeled leukocyte and bone scans to diagnose prosthetic joint infection. Clin Orthop Relat Res. 2000;373:241–7.
Bailey DL, Pichler BJ, Gückel B, et al. Combined PET/MRI: from status quo to status go. Summary report of the fifth international workshop on PET/MR imaging; February 15-19, 2016; Tübingen, Germany. Mol Imaging Biol. 2016;18(5):637–50.
Omar M, Ettinger M, Reichling M, et al. Synovial C-reactive protein as a marker for chronic periprosthetic infection in total hip arthroplasty. Bone Joint J. 2015;97-B(2):173–6.
Alijanipour P, Bakhshi H, Parvizi J. Diagnosis of periprosthetic joint infection: the threshold for serologic markers. Clin Orthop Relat Res. 2013;471(10):3186–95.
Ghanem E, Ketonis C, Restrepo C, Joshi A, Barrack R, Parvizi J. Periprosthetic infection: where do we stand with regard to Gram stain? Acta Orthop. 2009;80(1):37–40.
Ali S, Christie A, Chapel A. The pattern of procalcitonin in primary total hip and knee arthroplasty and its implication in periprosthetic infection. J Clin Med Res. 2009;1(2):90–4.
Berbari E, Mabry T, Tsaras G, et al. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2010;92(11):2102–9.
Bergin PF, Doppelt JD, Hamilton WG, et al. Detection of periprosthetic infections with use of ribosomal RNA-based polymerase chain reaction. J Bone Joint Surg Am. 2010;92:654–63.
Zmistowsky B, Restrepo C, Huang R, Hozack WJ, Parvizi J. Periprosthetic joint infection diagnosis: a complete understanding of white blood cell count and differential. J Arthroplast. 2012;27(9):1589–93.
Cipriano CA, Brown NM, Michael AM, Moric M, Sporer SM, Della Valle CJ. Serum and synovial fluid analysis for diagnosing chronic periprosthetic infection in patients with inflammatory arthritis. J Bone Joint Surg Am. 2012;94(7):594–600.
Della Valle GJ, Sporer SM, Jacobs JJ, Berger RA, Rosenberg AG, Paprosky WG. Preoperative testing for sepsis before revision total knee arthroplasty. J Arthroplast. 2007;22(6 suppl 2):90–3.
Elgeidi A, Elganainy AE, Abou Elkhier N, Rakha S. Interleukin-6 and other inflammatory markers in diagnosis of periprosthetic joint infection. Int Orthop. 2014;38(12):2591–5.
Ettinger M, Calliess T, Kielstein JT, et al. Circulating biomarkers for discrimination between aseptic joint failure, low-grade infection and high grade septic failure. Clin Infect Dis. 2015;61(3):332–41.
Fink B, Makowiak C, Fuerst M, Berger I, Schäfer P, Frommelt L. The value of synovial biopsy, joint aspiration and C-reactive protein in the diagnosis of late peri-prosthetic infection of total knee replacements. J Bone Joint Surg Br. 2008;90(7):874–8.
Fink B, Gebhard A, Fuerst M, Berger I, Schäfer P. High diagnostic value of synovial biopsy in periprosthetic joint infection of the hip. Clin Orthop Relat Res. 2013;471(3):956–64.
Gallo J, Kolar M, Dendis M, et al. Culture and PCR analysis of joint fluid in the diagnosis of prosthetic joint infection. New Microbiol. 2008;31(1):97–104.
Bernard L, Lübbeke A, Stern R, et al. Value of preoperative investigations in diagnosing prosthetic joint infection: retrospective cohort study and literature review. Scand J Infect Dis. 2004;36(6–7):410–6.
Glehr M, Friesenbichler J, Hofmann G, et al. Novel biomarkers to detect infection in revision hip and knee arthroplasties. Clin Orthop Relat Res. 2013;471(8):2621–8.
Greidanus NV, Masri BA, Garbuz DS, et al. Use of erythrocyte sedimentation rate and C-reactive protein level to diagnose infection before revision total knee arthroplasty: a prospective evaluation. J Bone Joint Surg Am. 2007;89(7):1409–16.
Hoell S, Borgers L, Gosheger G, et al. Interleukin-6 in two-stage revision arthroplasty: what is the threshold value to exclude persistent infection before re-implantation? Bone Joint J. 2015;97-B(1):71–5.
Gollwitzer H, Dombrowski Y, Prodinger PM, et al. Antimicrobial peptides and proinflammatory cytokines in periprosthetic joint infection. J Bone Joint Surg Am. 2013;95(7):644–51.
Ghanem E, Parvizi J, Burnett SJ, et al. Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. J Bone Joint Surg Am. 2008;90(8):1637–43.
Atkins BL, Athanasou N, Deeks JJ, et al. Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. J Clin Microbiol. 1998;36(10):2932–9.
Nilsdotter-Augustinsson A, Briheim G, Herder A, Ljunghusen O, Wahlström O, Öhman L. Inflammatory response in 85 patients with loosened hip prostheses: a prospective study comparing inflammatory markers in patients with aseptic and septic prosthetic loosening. Acta Orthop. 2007;78(5):629–39.
Bottner F, Wegner A, Winkelmann W, Becker K, Erren M, Götze C. Interleukin-6, procalcitonin and TNF-a: markers of peri-prosthetic infection following total joint replacement. J Bone Joint Surg Br. 2007;89(1):94–9.
Di Cesare PE, Chang E, Preston CF, Liu CJ. Serum interleukin-6 as a marker of periprosthetic infection following total hip and knee arthroplasty. J Bone Joint Surg Am. 2005;87(9):1921–7.
Parvizi J, Jacovides C, Adeli B, Jung KA, Hozack WJ, Mark B. Coventry award: synovial C-reactive protein: a prospective evaluation of a molecular marker for periprosthetic knee joint infection. Clin Orthop Relat Res. 2012;470(1):54–60.
Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am. 2008;90(9):1869–75.
Tetreault MW, Wetters NG, Moric M, Gross CE, Della Valle CJ. Is synovial C-reactive protein a useful marker for periprosthetic joint infection? Clin Orthop Relat Res. 2014;472(12):3997–4003.
Mason JG, Fehring TK, Odum SM, Griffin WL, Nussman DS. The value of white blood cell counts before revision total knee arthroplasty. J Arthroplast. 2003;18(8):1038–43.
Shanmugasundaram S, Ricciardi BF, Briggs TW, Sussmann PS and Bostrom MP. Evaluation and management of periprosthetic joint infection - an international, multicenter study. HSS J. 2014;10(1):36–44.
Murdoch DR, Roberts SA, Fowler VG Jr, et al. Infection of orthopedic prostheses after Staphylococcus aureus bacteremia. Clin Infect Dis. 2001;32(4):647e649.
Lyons CW, Berquist TH, Lyons JC, Rand JA, Brown ML. Evaluation of radiographic findings in painful hip arthroplasties. Clin Orthop Relat Res. 1985;195:239–51.
Tigges S, Stiles RG, Roberson JR. Appearance of septic hip prostheses on plain radiographs. AJR Am J Roentgenol. 1994;163(2):377–80.
Math KR, Zaidi SF, Petchprapa C, Harwin SF. Imaging of total knee arthroplasty. Semin Musculoskelet Radiol. 2006;10(1):47–63 Review.
Van Holsbeeck MT, Eyler WR, Sherman LS, Lombardi TJ, Mezger E, Verner JJ, et al. Detection of infection in loosened hip prostheses: efficacy of sonography. AJR Am J Roentgenol. 1994;163:381–4.
Weybright PN, Jacobson JA, Murry KH, Lin J, Fessell DP, Jamadar DA, et al. Limited effectiveness of sonography in revealing hip joint effusion: preliminary results in 21 adult patients with native and postoperative hips. AJR Am J Roentgenol. 2003;181:215–8.
Eisler T, Svensson O, Engström CF, Reinholt FP, Lundberg C, Wejkner B, et al. Ultrasound for diagnosis of infection in revision total hip arthroplasty. J Arthroplast. 2001;16(8):1010–7.
Battaglia M, Vannini F, Guaraldi F, Rossi G, Biondi F, Sudanese A. Validity of preoperative ultrasound-guided aspiration in the revision of hip prosthesis. Ultrasound Med Biol. 2011;37(12):1977–83.
Tomas X, Bori G, Garcia S, Garcia-Diez AI, Pomes J, Soriano A, et al. Accuracy of CT-guided joint aspiration in patients with suspected infection status post-total hip arthroplasty. Skelet Radiol. 2011;40(1):57–64.
Trampuz A, Piper KE, Hanssen AD, et al. Sonication of explanted prosthetic components in bags for diagnosis of prosthetic joint infection is associated with risk of contamination. J Clin Microbiol. 2006;44(2):628–31.
Vasoo S, Cunningham SA, Greenwood-Quaintance KE, et al. Evaluation of the film array blood culture ID panel on biofilms dislodged from explanted arthroplasties for prosthetic joint infection diagnosis. J Clin Microbiol. 2015;53(8):2790–2.
Hindle P, Davidson E, Biant LC. Septic arthritis of the knee: the use and effect of antibiotics prior to diagnostic aspiration. Ann R Coll Surg Engl. 2012;94(5):351–5.
Cazanave C, Greenwood-Quaintance KE, Hanssen AD, et al. Rapid molecular microbiologic diagnosis of prosthetic joint infection. J Clin Microbiol. 2013;51(7):2280–7.
Esteban J, Gomez-Barrena E, Cordero J, Martín-de-Hijas NZ, Kinnari TJ, Fernandez-Roblas R. Evaluation of quantitative analysis of cultures from sonicated retrieved orthopedic implants in diagnosis of orthopedic infection. J Clin Microbiol. 2008;46(2):488–92.
Cheung A, Lachiewicz PF, Renner JB. The role of aspiration and contrast-enhanced arthrography in evaluating the uncemented hip arthroplasty. AJR Am J Roentgenol. 1997;168(5):1305–9.
Howard CB, Einhorn M, Dagan R, Yagupski P, Porat S. Fine-needle bone biopsy to diagnose osteomyelitis. J Bone Joint Surg Br. 1994;76(2):311–4.
Bonhoeffer J, Haeberle B, Schaad UB, Heininger U. Diagnosis of acute haematogenous osteomyelitis and septic arthritis, 20 years experience at the University Children’s Hospital Basel. Swiss Med Wkly. 2001;131(39–40):575–81.
Barrack RL, Harris WH. The value of aspiration of the hip joint before revision total hip arthroplasty. J Bone Joint Surg Am. 1993;75(1):66–76.
Portillo ME, Salvadó M, Sorli L, et al. Multiplex PCR of sonication fluid accurately differentiates between prosthetic joint infection and aseptic failure. J Inf Secur. 2012;65(6):541–8.
Janz V, Wassilew GI, Kribus M, Trampuz A, Perka C. Improved identification of polymicrobial infection in total knee arthroplasty through sonicate fluid cultures. Arch Orthop Trauma Surg. 2015;135(10):1453–7.
Minassian AM, Newham R, Kalimeris E, Bejon P, Atkins BL, Bowler ICJW. Use of an automated blood culture system (BD BACTEC) for the diagnosis of prosthetic joint infections: easy and fast. BMC Infect Dis. 2014;14:233.
Frangiamore SJ, Gajewski ND, Saleh A, Farias-Kovac M, Barsoum WK, Higuera CA. Alfa-defensin accuracy to diagnose periprosthetic joint infection - best available test? J Arthroplast. 2016;31(2):456–60.
Frangiamore SJ, Saleh A, Grosso MJ, et al. α-Defensin as a predictor of periprosthetic shoulder infection. J Shoulder Elb Surg. 2015;24(7):1021–7.
Cipriano C, Maiti A, Hale G, Jiranek W. The host response: toll-like receptor expression in periprosthetic tissues as a biomarker for deep joint infection. J Bone Joint Surg Am. 2014;96(20):1692–8.
Liu JZ, Saleh A, Klika AK, Barsoum WK, Higuera CA. Serum inflammatory markers for periprosthetic knee infection in obese versus non-obese patients. J Arthroplast. 2014;29(10):1880–3.
Bingham J, Clarke H, Spangehl M, Schwartz A, Beauchamp C, Goldberg B. The alpha defensin-1 biomarker assay can be used to evaluate the potentially infected total joint arthroplasty. Clin Orthop Relat Res. 2014;472(12):4006–9.
Lenski M, Scherer MA. Synovial IL-6 as inflammatory marker in periprosthetic joint infections. J Arthroplast. 2014;29(6):1105–9.
Jacovides CL, Parvizi J, Adeli B, Jung KA. Molecular markers for diagnosis of periprosthetic joint infection. J Arthroplast. 2011;26(6 suppl):99–103.
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J. Combined measurement of synovial fluid alpha-defensin and C-reactive protein levels: highly accurate for diagnosing periprosthetic joint infection. J Bone Joint Surg Am. 2014;96(17):1439–45.
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J. Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res. 2014;472(11):3254–62.
Ali F, Wilkinson JM, Cooper JR, et al. Accuracy of joint aspiration for the preoperative diagnosis of infection in total hip arthroplasty. J Arthroplast. 2006;21(2):221–6.
Achermann Y, Vogt M, Leunig M, Wüst J, Trampuz J. Improved diagnosis of periprosthetic joint infection by multiplex PCR of sonication fluid from removed implants. J Clin Microbiol. 2010;48(4):1208–14.
Wetters NG, Berend KR, Lombardi AV, Morris MJ, Tucker TL, Della Valla CJ. Leukocyte esterase reagent strips for the rapid diagnosis of periprosthetic joint infection. J Arthroplast. 2012;27(8 suppl):8–11.
Mikkelsen DB, Pedersen C, Højbjerg T, Schønheyder HC. Culture of multiple peroperative biopsies and diagnosis of infected knee arthroplasties. APMIS. 2006;114(6):449–52.
Esteban J, Alonso-Rodriguez N, del Prado G, et al. PCR-hybridization after sonication improves diagnosis of implant-related infection. Acta Orthop. 2012;83(3):299–304.
Gomez E, Cazanave C, Cunningham SA, et al. Prosthetic joint infection diagnosis using broad-range PCR of biofilms dislodged from knee and hip arthroplasty surfaces using sonication. J Clin Microbiol. 2012;50(11):3501–8.
Tunney MM, Patrick S, Curran MD, et al. Detection of prosthetic hip infection at revision arthroplasty by immunofluorescence microscopy and PCR amplification of the bacterial 16S rRNA gene. J Clin Microbiol. 1999;37(10):3281–90.
Rak M, Barlic-Maganja D, Kavcic M, Trebse R, Cor A. Comparison of molecular and culture method in diagnosis of prosthetic joint infection. FEMS Microbiol Lett. 2013;343(1):42–8.
Morawietz L, Tiddens O, Mueller M, et al. Twenty-three neutrophil granulocytes in 10 high-power fields is the best histopathological threshold to differentiate between aseptic and septic endoprosthesis loosening. Histopathology. 2009;54(7):847–53.
Spangehl MJ, Masterson E, Masri BA, O’Connell JX, Duncan CP. The role of intraoperative gram stain in the diagnosis of infections during revision total hip arthroplasty. J Arthroplast. 1999;14(8):952–6.
Barrack RL, Jennings RW, Wolfe MW, Bertot AJ. The Coventry award. The value of preoperative aspiration before total knee revision. Clin Orthop Relat Res. 1997;345:8–16.
Datz FL, Thorne DA. Effect of antibiotic therapy on the sensitivity of indium-111-labeled leukocyte scans. J Nucl Med. 1986;27(12):1849–53.
McCarthy K, Velchik MG, Alavi A, Mandell GA, Esterhai JL, Goll S. Indium-111-labeled white blood cells in the detection of osteomyelitis complicated by a pre-existing condition. J Nucl Med. 1988;29(6):1015–21.
Kolindou A, Liu Y, Ozker K, Krasnow AZ, Isitman AT, Hellman RS, et al. In-111 WBC imaging of osteomyelitis in patients with underlying bone scan abnormalities. Clin Nucl Med. 1996;21(3):183–91.
Van der Wall H, Lunz D, Stanton F, Bruce W. Prognostic value of 99m Tc leukocyte scintigraphy in diabetic pedal osteomyelitis. Foot Ankle Int. 2001;22(9):720–4.
Vesco L, Boulahdour H, Hamissa S, Kretz S, Montazel JL, Perlemuter L, et al. The value of combined radionuclide and magnetic resonance imaging in the diagnosis and conservative management of minimal or localized osteomyelitis of the foot in diabetic patients. Metabolism. 1999;48(7):922–7.
Newman LG, Waller J, Palestro CJ, Schwartz M, Klein MJ, Hermann G, et al. Unsuspected osteomyelitis in diabetic foot ulcers. Diagnosis and monitoring by leukocyte scanning with indium 111 oxyquinoline. JAMA. 1991;266(9):1246–51.
Chik KK, Magee MA, Bruce WJ, Higgs RJ, Thomas MG, Allman KC, et al. Tc-99m stannous colloid-labeled leukocyte scintigraphy in the evaluation of the painful arthroplasty. Clin Nucl Med. 1996;21(11):838–43.
Schmidt KG, Rasmussen JW, Wedebye IM, Frederiksen PB. Analysis of factors that may affect the speed of accumulation of 111In-labelled granulocytes at sites of inflammation. Nucl Med Commun. 1988;9(2):97–103.
Kim DG, Lee JI, Lee DS, Lee MC, Choi KS, Han DH. 99mTc-HMPAO labeled leukocyte SPECT in intracranial lesions. Surg Neurol. 1995;44(4):338–45.
Kristinsson JK, Sigurdsson H, Sigfusson A, Gudmundsson S, Agnarsson BA. Detection of orbital implant infection with technetium 99m-labeled leukocytes. Ophthal Plast Reconstr Surg. 1997;13:256–8.
Ascher NL, Forstrom L, Simmons RL. Radiolabeled autologous leukocyte scanning in abscess detection. World J Surg. 1980;4:395–402.
Knochel JQ, Koehler PR, Lee TG, Welch DM, et al. Diagnosis of abdominal abscesses with computed tomography, ultrasound, and indium-111leukocyte scans. Radiology. 1980;137:425–32.
Laitinen R, Tahtinen J, Lantto T, Vorne M. Tc-99m labeled leukocytes in imaging of patients with suspected acute abdominal inflammation. Clin Nucl Med. 1990;15:597–602.
Challa S, Lyons KP, Broekelschen P, Milne N. Relative sensitivity of Tc-99mWBC versus in-111 WBC in a patient with Crohn disease and steroid use. Clin Nucl Med. 1997;22:700–3.
Chung CJ, Hicklin OA, Payan JM, Gordon L. Indium-111-labeled leukocyte scan in detection of synthetic vascular graft infection: the effect of antibiotic treatment. J Nucl Med. 1991;32:13–5.
Ramackers JM, Kotzki PO, Couret I, Messner-Pellenc P, Davy JM, Rossi M. The use of technetium-99m hexamethylpropylene amine oxime labelled granulocytes with single-photon emission tomography imaging in the detection and follow-up of recurrence of infective endocarditis complicating transvenous endocardial pacemaker. Eur J Nucl Med. 1995;22:1351–4.
Cyteval C, Hamm V, Sarrabère MP, Lopez FM, Maury P, Taourel P. Painful infection at the site of hip prosthesis: CT imaging. Radiology. 2002;224(2):477–83.
Cahir JG, Toms AP, Marshall TJ, Wimhurst J, Nolan J. CT and MRI of hip arthroplasty. Clin Radiol. 2007;62(12):1163–71 discussion 1172–1173.
Roth TD, Maertz NA, Parr JA, Buckwalter KA, Choplin RH. CT of the hip prosthesis: appearance of components, fixation, and complications. Radiographics. 2012;32(4):1089–107.
Wong MY, Beadsmoore C, Toms A, Smith T, Donell S. Does 99mTc-MDP bone scintigraphy add to the investigation of patients with symptomatic unicompartmental knee replacement? Knee. 2012;19(5):592–6.
Yue B, Tang T. The use of nuclear imaging for the diagnosis of periprosthetic infection after knee and hip arthroplasties. Nucl Med Commun. 2015;36(4):305–11.
Love C, Marwin SE, Palestro CJ. Nuclear medicine and the infected joint replacement. Semin Nucl Med. 2009;39(1):66–78.
Nagoya S, Kaya M, Sasaki M, Tateda K, Yamashita T. Diagnosis of peri-prosthetic infection at the hip using triple-phase bone scintigraphy. J Bone Joint Surg Br. 2008;90(2):140–4.
Temmerman OP, Raijmakers PG, Deville WL, Berkhof J, Hooft L, Heyligers IC. The use of plain radiography, subtraction arthrography, nuclear arthrography, and bone scintigraphy in the diagnosis of a loose acetabular component of a total hip prosthesis: a systematic review. J Arthroplast. 2007;22(6):818–27.
Ikeuchi M, Okanoue Y, Izumi M, Fukuda G, Aso K, Sugimura N, et al. Diagnostic value of triple-phase bone scintigraphy for the diagnosis of infection around antibiotic-impregnated cement spacers. Springerplus. 2013;2:401. https://doi.org/10.1186/2193-1801-2-401.
Nagoya S, Kaya M, Sasaki M, Tateda K, Yamashita T. Diagnosis of peri-prosthetic infection at the hip using triple-phase bone scintigraphy. J Bone Joint Surg Br. 2008 Feb;90(2):140–4.
Volpe L, Indelli PF, Latella L, Poli P, Yakupoglu J, Marcucci M. Periprosthetic joint infections: a clinical practice algorithm. Joints. 2015 Feb 13;2(4):169–74.
Trevail C, Ravindranath-Reddy P, Sulkin T, Bartlett G. An evaluation of the role of nuclear medicine imaging in the diagnosis of periprosthetic infections of the hip. Clin Radiol. 2016 Mar;71(3):211–9.
Ouyang Z, Li H, Liu X, Zhai Z, Li X. Prosthesis infection: diagnosis after total joint arthroplasty with three-phase bone scintigraphy. Ann Nucl Med. 2014;28(10):994–1003.
Glaudemans AW, de Vries EF, Vermeulen LE, Slart RH, Dierckx RA, Signore A. A large retrospective single-centre study to define the best image acquisition protocols and interpretation criteria for white blood cell scintigraphy with99mTc-HMPAO-labelled leucocytes in musculoskeletal infections. Eur J Nucl Med Mol Imaging. 2013;40(11):1760–9.
Lima AL, Oliveira PR, Carvalho VC, Saconi ES, Cabrita HB, Rodrigues MB. Periprosthetic joint infections. Interdiscip Perspect Infect Dis. 2013;2013:542796.
Temmerman OP, Raijmakers PG, Berkhof J, David EF, Pijpers R, Molenaar MA, et al. Diagnostic accuracy and interobserver variability of plain radiography, subtraction arthrography, nuclear arthrography, and bone scintigraphy in the assessment of aseptic femoral component loosening. Arch Orthop Trauma Surg. 2006;126(5):316–23.
Signore A, Glaudemans AW, Galli F, Rouzet F. Imaging infection and inflammation. Biomed Res Int. 2015;2015:615150.
Palestro CJ. Nuclear medicine and the failed joint replacement: past, present, and future. World J Radiol. 2014;6(7):446–58.
Jutte P, Lazzeri E, Sconfienza LM, Cassar-Pullicino V, Trampuz A, Petrosillo N, et al. Diagnostic flowcharts in osteomyelitis, spondylodiscitis and prosthetic joint infection. Q J Nucl Med Mol Imaging. 2014;58(1):2–19.
Jamar F, Buscombe J, Chiti A, Christian PE, Delbeke D, Donohoe KJ, et al. EANM/SNMMI guideline for 18F-FDG use in inflammation and infection. J Nucl Med. 2013;54(4):647–58.
Kim HO, Na SJ, Oh SJ, Jung BS, Lee SH, Chang JS, et al. Usefulness of adding SPECT/CT to 99mTc-hexamethylpropylene amine oxime (HMPAO)-labeled leukocyte imaging for diagnosing prosthetic joint infections. J Comput Assist Tomogr. 2014;38(2):313–9.
Erba PA, Glaudemans AW, Veltman NC, Sollini M, Pacilio M, Galli F, et al. Image acquisition and interpretation criteria for 99mTc-HMPAO-labelled white blood cell scintigraphy: results of a multicentre study. Eur J Nucl Med Mol Imaging. 2014;41(4):615–23.
Sousa R, Massada M, Pereira A, Fontes F, Amorim I, Oliveira A. Diagnostic accuracy of combined 99mTc-sulesomab and 99mTc-nanocolloid bone marrow imaging in detecting prosthetic joint infection. Nucl Med Commun. 2011;32(9):834–9.
Jung KP, Park JS, Lee AY, Choi SJ, Lee SM, Bae SK. The clinical usefulness of (99m)Tc HMPAO leukocyte/(99m)Tc phytate bone marrow scintigraphy for diagnosis of prosthetic knee infection: a preliminary study. Nucl Med Mol Imaging. 2012;46(4):247–53.
Simonsen L, Buhl A, Oersnes T, Duus B. White blood cell scintigraphy for differentiation of infection and aseptic loosening: a retrospective study of 76 painful hip prostheses. Acta Orthop. 2007;78(5):640–7.
Basu S, Kwee TC, Saboury B, Garino JP, Nelson CL, Zhuang H, Parsons M, Chen W, Kumar R, Salavati A, Werner TJ, Alavi A. FDG PET for diagnosing infection in hip and knee prostheses: prospective study in 221 prostheses and subgroup comparison with combined (111)In-labeled leukocyte/(99m)Tc-sulfur colloid bone marrow imaging in 88 prostheses.
Vanquickenborne B, Maes A, Nuyts J, Van Acker F, Stuyck J, Mulier M, et al. The value of (18)FDG-PET for the detection of infected hip prosthesis. Eur J Nucl Med Mol Imaging. 2003;30(5):705–15.
Pill SG, Parvizi J, Tang PH, Garino JP, Nelson C, Zhuang H, et al. Comparison of fluorodeoxyglucose positron emission tomography and(111)indium-white blood cell imaging in the diagnosis of periprosthetic infection of the hip. J Arthroplast. 2006;21(6 Suppl 2):91–7.
Richter WS, Ivancevic V, Meller J, Lang O, Le Guludec D, Szilvazi I, et al. 99mTc-besilesomab (Scintimun) in peripheral osteomyelitis: comparison with 99mTc-labelled white blood cells. Eur J Nucl Med Mol Imaging. 2011;38(5):899–910.
Palestro CJ. Radionuclide imaging of osteomyelitis. Semin Nucl Med. 2015;45(1):32–46.
Pakos EE, Trikalinos TA, Fotopoulos AD, Ioannidis JP. Prosthesis infection: diagnosis after total joint arthroplasty with antigranulocyte scintigraphy with 99mTc-labeled monoclonal antibodies—a meta-analysis. Radiology. 2007;242(1):101–8.
Xing D, Ma X, Ma J, Wang J, Chen Y, Yang Y. Use of anti-granulocyte scintigraphy with 99mTc-labeled monoclonal antibodies for the diagnosis of periprosthetic infection in patients after total joint arthroplasty: a diagnostic meta-analysis. PLoS One. 2013;8(7):e69857.
Filippi L, Schillaci O. Usefulness of hybrid SPECT/CT in 99mTc-HMPAO-labeled leukocyte scintigraphy for bone and joint infections. J Nucl Med, 47. 2006;(12):1908–13.
Graute V, Feist M, Lehner S, Haug A, Müller PE, Bartenstein P, et al. Detection of low-grade prosthetic joint infections using 99mTc-antigranulocyte SPECT/CT: initial clinical results. Eur J Nucl Med Mol Imaging. 2010;37(9):1751–9.
Schillaci O. Hybrid imaging systems in the diagnosis of osteomyelitis and prosthetic joint infection. Q J Nucl Med Mol Imaging. 2009;53(1):95–104 Review.
Pelosi E, Baiocco C, Pennone M, Migliaretti G, Varetto T, Maiello A, et al. 99mTc-HMPAO-leukocyte scintigraphy in patients with symptomatic total hip or knee arthroplasty: improved diagnostic accuracy by means of semiquantitative evaluation. J Nucl Med. 2004;45(3):438–44.
Papós M, Barát F, Nárai G, Dillmann J, Láng J, Csernay L. Tc-99m HMPAO leukocyte and Tc-99m nanocolloid scintigraphy in posttraumatic bone infection. Clin Nucl Med. 1998;23(7):423–8.
Van Acker F, Nuyts J, Maes A, Vanquickenborne B, Stuyck J, Bellemans J, et al. FDG-PET, 99mtc-HMPAO white blood cell SPET and bone scintigraphy in the evaluation of painful total knee arthroplasties. Eur J Nucl Med. 2001;28(10):1496–504.
Mulamba L, Ferrant A, Leners N, de Nayer P, Rombouts JJ, Vincent A. Indium-111 leucocyte scanning in the evaluation of painful hip arthroplasty. Acta Orthop Scand. 1983;54(5):695–7.
Palestro CJ, Kim CK, Swyer AJ, Capozzi JD, Solomon RW, Goldsmith SJ. Total-hip arthroplasty: periprosthetic indium-111-labeled leukocyte activity and complementary technetium-99m-sulfur colloid imaging in suspected infection. J Nucl Med. 1990;31(12):1950–5.
Palestro CJ, Love C, Tronco GG, Tomas MB, Rini JN. Combined labeled leukocyte and technetium 99m sulfur colloid bone marrow imaging for diagnosing musculoskeletal infection. Radiographics. 2006;26(3):859–70 Review.
Palestro CJ, Swyer AJ, Kim CK, Goldsmith SJ. Infected knee prosthesis: diagnosis with in-111 leukocyte, Tc-99m sulfur colloid, and Tc-99m MDP imaging. Radiology. 1991;179(3):645–8.
El Espera I, Blondet C, Moullart V, Saïdi L, Havet E, Mertl P, et al. The usefulness of 99mTc sulfur colloid bone marrow scintigraphy combined with 111In leucocyte scintigraphy in prosthetic joint infection. Nucl Med Commun. 2004;25(2):171–5.
Joseph TN, Mujtaba M, Chen AL, Maurer SL, Zuckerman JD, Maldjian C, et al. Efficacy of combined technetium-99m sulfur colloid/indium-111 leukocyte scans to detect infected total hip and knee arthroplasties. J Arthroplast. 2001;16(6):753–8.
Talbot BS, Weinberg EP. MR imaging with metal-suppression sequences for evaluation of total joint arthroplasty. Radiographics. 2016;36(1):209–25.
Sneag DB, Bogner EA, Potter HG. Magnetic resonance imaging evaluation of the painful total knee arthroplasty. Semin Musculoskelet Radiol. 2015;19(1):40–8.
Aliprandi A, Sconfienza LM, Randelli F, Bandirali M, Di Leo G, Sardanelli F. Magnetic resonance imaging of painful total hip replacement: detection and characterisation of periprosthetic fluid collection and interobserver reproducibility. Radiol Med. 2012;117(1):85–95.
Acknowledgements
Alberto Signore, Andor WJM Glaudemans, and Olivier Gheysens are representatives of the European Association of Nuclear Medicine (EANM); Luca Maria Sconfienza, Victor Cassar-Pullicino, and Filip MHM Vanhoenacker are representatives of the European Society of Radiology (ESR); Olivier Borens, Heinz Winkler, and Paul C. Jutte are representatives of the European Bone and Joint Infection Society (EBJIS); Andrej Trampuz and Nicola Petrosillo are representatives of the European Society of Clinical Microbiology and Infectious Diseases (ESCMID).
We wish to thank the many people who contributed to these guidelines by actively working on them or just contributing with useful discussion: first of all, the members of the EANM Committee on Infection and Inflammation (Elena Lazzeri, Riddhika Chakravarrty, Chiara Lauri, Vera Artico, Andrè Diaz, Samantha Terry, Paola Erba, and John Buscombe) and the important advice we received from other committees, and in particular the Bone & Joint Committee, the Radiopharmacy Committee, and the Technologist Committee of EANM.
We also thank the boards of ESR, EBJIS, and ESCMID for supporting this work and the dissemination of our results in international congresses. We thank Claudia Löwik for performing a literature search and retrieving articles.
Each practice guideline, representing a policy statement, has undergone a thorough consensus process in which it has been subjected to extensive review. EANM/ESR/EBJIS and ESCMID recognize that the safe and effective use of diagnostic imaging requires specific training, skills, and techniques, as described in each document.
This guideline was brought to the attention of all other EANM committees and to the national societies of nuclear medicine. The comments and suggestions from the Oncology Committee, the Radiation Protection Committee, and the Translational-Molecular Imaging Committee, and from the Czech Republic, Italian, Latvian, Russian, German, and Polish national societies are highly appreciated and have been considered for this Guideline.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. For this type of study, formal consent is not required.
Disclaimer
The European Association of Nuclear Medicine (EANM) has written and approved guidelines to promote the use of nuclear medicine procedures of high quality. The guidelines should not be deemed inclusive of all proper procedures and exclusive of other procedures reasonably directed to obtaining the same results.
The facilities in a specialized practice setting may be different from those in a more general setting. Resources available to care for patients, legislation, and local regulations may vary greatly from one European country or one medical facility to another. For these reasons, these guidelines cannot be rigidly applied.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised as the author name Victor Casar-Pullicino should have been Victor Cassar-Pullicino.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Signore, A., Sconfienza, L.M., Borens, O. et al. Consensus document for the diagnosis of prosthetic joint infections: a joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur J Nucl Med Mol Imaging 46, 971–988 (2019). https://doi.org/10.1007/s00259-019-4263-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-4263-9