Abstract
Purpose
The purpose of this study was to provide a critical systematic review of the role of magnetic resonance imaging (MRI) as a noninvasive method to assess periprosthetic joint infections (PJIs).
Methods
The electronic databases PubMed and EMBASE were searched, since their inception up to March 27, 2022. The included studies evaluated the reproducibility and accuracy of MRI features to diagnose PJIs. The article quality assessment was conducted by the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2).
Results
Among 1909 studies identified in the initial search, 8 studies were eligible for final systematic review. The included studies evaluated the reproducibility and accuracy of MRI features to diagnose PJIs. Seven of 8 studies showed good to excellent reliability, but only one article among them in which accuracy was evaluated had a low risk of bias. The intraclass correlation coefficient (ICC) and Cohen coefficient (κ) varied between 0.44 and 1.00. The accuracy varied between 63.9% and 94.4%. Potential MRI features, such as lamellated hyperintense synovitis, edema, fluid collection, or lymphadenopathy, might be valuable for diagnosing PJIs.
Conclusion
The quality of the evidence regarding the role of MRI for PJIs diagnosis was low. There is preliminary evidence that MRI has a noteworthy value of distinguishing suspected periprosthetic joint infection in patients with total knee arthroplasty or total hip arthroplasty, but the definition of specific MRI features related to PJIs diagnosis lacks consensus and standardization. Large-scale studies with robust quality were required to help make better clinical decisions in the future.
Similar content being viewed by others
Introduction
Total joint arthroplasty (TJA) has become the most common standard treatment for severe end-stage hip or knee disease, allowing joint pain relief, improvement of physical activity, and an increase in quality of life [1,2,3,4]. Although the postsurgical outcomes are usually excellent [5,6,7,8], the incidence of various complications will continue to increase over time, in large part due to the rise in the number of TJA over recent years and the increased life expectancy [9, 10]. Among these, periprosthetic joint infections (PJIs) is devastating because of prolonged hospitalization, repeated surgical interventions, or severe psychological and economic burden to patients [11, 12].
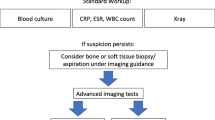
Determining the presence of PJIs remains a challenge of modern orthopedics as there is no gold standard diagnostic tool [13, 14]. In the last decade, the commonly used diagnostic criteria for PJIs were released by the European Bone and Joint Infection Society (EBJIS), Musculo-Skeletal Infection Society (MSIS) or two International Consensus Meetings on PJIs in 2013 (ICM 2013) and 2018 (ICM 2018) [15,16,17]. In general, the diagnostic approach in patients with suspected PJIs involves clinical findings, laboratory evaluation, radiology, biopsies with microbiological analysis, nuclear imaging, or intraoperative findings [18, 19]. There is no clear consensus about the choice of the most accurate imaging technique to detect suspected PJIs [20], especially in the case of a challenging diagnosis of an early or low-virulence infection.
Since the development of advanced metal artifact reducing techniques, magnetic resonance imaging (MRI) has been increasingly recognized as a noninvasive and valuable method in the evaluation of patients with septic arthritis [21] or hip and knee pain after arthroplasty [22,23,24,25]. However, there are two issues with the MRI diagnostic value of PJIs: (1) To date, there is no consensus on the diagnostic value of MRI for PJIs in total hip arthroplasty (THA) or total knee arthroplasty (TKA) patients [26,27,28,29,30,31,32,33]; and (2) There are no consistent criteria for the identification or definition of specific MRI features related to PJIs diagnosis. Consequently, it is necessary to systematically evaluate the diagnostic value of MRI features for PJIs.
This systematic review aimed to analyze the main value of MRI for PJIs diagnosis and summarize various helpful MRI appearances in identifying infected prostheses for THA or TKA patients.
Materials and methods
This systematic review strictly adheres to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [34]. Ethics committee approval was not needed to conduct a systematic review of the published literature.
Search strategy
In March 27, 2022, a systematic literature search of the PubMed (Medline) and EMBASE (Elsevier) databases was conducted to identify the original studies that reported the imaging features of MRI for the diagnosis of PJIs. The detailed search terms were as follows: (Periprosthetic Infection OR Infected OR painful OR symptomatic) AND (THA OR TKA OR TJA OR TKR OR THR OR Knee Arthroplasty OR Hip Arthroplasty) AND (MRI OR MR OR MR Imaging OR magnetic resonance imaging) AND (Hip OR knee). The bibliographies of the included studies were also hand-screened to expand the search extent and to avoid missing relevant articles. Moreover, there were no search date limits in this study.
Inclusion and exclusion criteria
After inspection for duplicates, studies were included based on the following inclusion criteria: (1) original articles in a peer-reviewed journal; (2) human studies; (3) reports on the features of MRI for the diagnosis of PJIs after THA or TKA; and (4) original articles in English. Studies were excluded if any of following criteria were satisfied: (1) review articles; (2) meta-analyses; (3) letters to the editor; (4) replies; (5) comments; (6) conference abstracts; (7) editorials; (8) case reports; (9) non-English studies; and (10) studies involving only animals.
Study selection and data extraction
The eligible articles were independently selected by two reviewers according to title and abstract assessment. The final decision regarding inclusion was based on the full-text articles. If consensus was not reached in case of disagreement, a third reviewer was included.
The following study characteristics were extracted from the eligible studies: (1) authors; (2) year of publication; (3) study design; (4) number of subjects; (5) sex; (6) age; (7) prosthesis; (8) number of prostheses (total/infected/noninfected); (9) MRI setting; (10) duration from THA or TKA to MRI examination; and 11) study outcomes, including interrater and intrarater reliability (intraclass correlation coefficient (ICC) for continuous variables and Cohen coefficient (κ) for categorical variables with standard errors), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy. Data extraction was conducted independently by the two reviewers, and any disputes between them were resolved by a consensus meeting.
Methodologic quality appraisal and analysis
The included articles evaluated the reproducibility and accuracy of MRI features to diagnose PJIs. To assess the quality of these articles, the COnsensus-based Standards for the selection of health Measurement Instruments (COSMIN) tool and Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool were used.
The reproducibility of the included articles in this study can be evaluated by reliability assessment using COSMIN reliability box 6 [35]. Reliability box 6 contains 3 domains: design requirements, statistical methods and other flaws [35]. Each standard is answered by the four point rating system (inadequate, doubtful, adequate, or very good) [36], and the final rating is determined by the lowest score given for any of the standards in box 6 (the worst score counts method) [37]. Interrater or intrarater reproducibility can be calculated with κ or ICC. The κ statistic was interpreted as follows: almost perfect agreement (0.81-1), substantial agreement (0.61–0.80), moderate agreement (0.41–0.60), fair agreement (0.21–0.40), slight agreement (0.01–0.20), and no agreement (0) [38]. The definition of ICC values was as follows: excellent reliability (> 0.90), good reliability (0.75–0.90), moderate reliability (0.50–0.75), and poor reliability (< 0.50) [39].
The QUADAS-2 tool is recommended for use in rating bias and applicability of a majority of diagnostic accuracy studies [40]. The QUADAS-2 contains 4 domains: patient selection, index test, reference standard, and flow and timing. Each question can be assessed with “low risk of bias”, “high risk of bias”, or “unclear risk” [41]. Moreover, sensitivity, specificity, PPV, NPV and accuracy were also calculated for each MRI feature.
Results
Search results
A flowchart of study selection is shown in Fig. 1. The systematic search strategy identified 1909 articles from PubMed and EMBASE. After removing 236 duplicate articles, 1673 articles remained. Of these, 1664 were excluded after analyzing the information in the title and abstract, while the remaining 9 full-text articles were downloaded for a further assessment. One article was excluded because it included only one patient with PJIs [42]. No other potentially relevant studies were extracted from the bibliographies of these articles. Finally, 8 eligible articles, which included a total of 645 patients, were summarized and analyzed in this study [26,27,28,29,30,31,32,33].
Characteristics of included studies
The detailed study characteristics are summarized in Table 1. The included studies were published in 2013 (1/8) [33], 2014 (1/8) [31], 2016 (2/8) [30, 32], 2020 (3/8) [27,28,29] and 2021 (1/8) [26]. The study design was retrospective in 87.5% (7/8) of studies [26,27,28,29,30, 32, 33] and prospective in 12.5% (1/8) [31]. The number of subjects ranged from 30 to 140 patients. Six studies detected the diagnostic role of MRI for THA patients [26,27,28,29,30,31] and the remaining two studies focused on the MRI features of TKA patients [32, 33]. Altogether, a total of 645 patients, 206 (31.94%) with and 439 (68.06%) without PJIs, were assessed in 481 (74.57%) hip prostheses and 164 (25.43%) knee prostheses. MRI was performed by 1.5 T scanners in all eight studies.
Study quality appraisal and analysis
For reproducibility assessment (Table 2), seven studies were scored adequate to very good by the COSMIN reliability box [26,27,28,29,30, 32, 33], and only one study was scored inadequate [31]. Nevertheless, approximately 12.5% of the included articles did not analyze interrater reliability, and 50% of the included studies did not provide intrarater reliability assessment.
For accuracy assessment (Figs. 2 and 3), the methodological quality of seven studies had a high risk of bias [27,28,29,30,31,32,33], and only one study had a low risk of bias [26]. Because only one retrospective study scored a low risk of bias [26], the accuracy of the included articles showed more concerns regarding patient selection. Generally, the retrospective study design property will increase susceptibility to selection bias. In addition, the majority of included studies provide necessary information in regard to index test, reference standard, or flow and timing [26,27,28,29, 32, 33].
MRI findings and PJIs
As shown in Tables 2 and 3, MRI features demonstrated high diagnostic performance in evaluating suspected PJIs, but the individual MRI signs of PJIs around the prosthesis varied or were inconsistent among all included studies. The important MRI findings of PJIs are summarized as follows:
Synovitis is common in patients with hip or knee prostheses, and the lamellated hyperintense synovitis (LHS) is the most suggestive MRI sign of PJIs in THA [26, 28, 31] or TKA [32, 33] patients. Reasonable reliability results were found regarding LHS, with an interrater reliability of (K, 0.76–0.907) and interrater reliability of (K, 0.44–0.89) [26, 28, 32, 33]. The sensitivity and specificity for diagnosing PJIs by LHS on MRI varied between 26.3% and 86% for sensitivity and between 84% and 98.8% for specificity. The diagnostic accuracy of LHS ranged from 74.8 to 94.4% [26, 28, 32, 33].
Edema, including bone edema [26, 31], extracapsular edema [26, 31], capsule edema [27], intramuscular edema [27], and adjacent soft tissue edema [29,30,31] had a high correlation with the clinical diagnosis of PJIs. Interrater reliability was almost perfect for bone edema (K = 0.927) [26], extracapsular edema (K, 0.905–0.923) [26], capsule edema (K = 0.88) [27], intramuscular edema (K = 0.73–0.88) [27], and adjacent soft tissue edema (K = 0.955) [29]. The sensitivity of edema on MRI for PJI was 68.4 − 100%, and the specificity for diagnosing PJIs by edema on MRI was 73.1 − 95%. The diagnostic accuracy of edema ranged from 79.8 to 93% [26, 27, 29,30,31].
The MRI appearance of extracapsular collection (or fluid collection) [26, 27, 31] was suggestive of an infected arthroplasty implant. Interrater reliability was almost perfect (K, 0.905–0.923) or substantial (K = 0.68) for extracapsular collection. These articles reported the sensitivity and specificity values of 28–58% and 77.8–98%, respectively [26, 27]. The diagnostic accuracy of extracapsular collection ranged from 68.9 to 85% [26, 27].
A correlation was found between reactive lymphadenopathy (or nodal indices) on MRI and PJIs [26, 27, 29]. Results demonstrated excellent reliability for lymphadenopathy (ICC = 0.98, K, 0.844–0.99) [26, 29]. The sensitivity and specificity of the diagnoses varied between 78.9 − 93% and 47 − 87.7% [26, 29]. The diagnostic accuracy of lymphadenopathy ranged from 70 to 93.1% [26, 29].
Details of other MRI signs of PJIs are shown in Tables 2 and 3.
Discussion
The present study aimed to systematically review the role of MRI in the assessment of infected joint prostheses for THA or TKA patients. The main findings suggest that MRI is capable of identifying suspected periprosthetic joint infection, but the definition of specific MRI features related to PJIs diagnosis lacks consensus and standardization.
All included articles were published in the last 8 years, with a rapid rise in published articles per year over time, especially in 2020–2021. The publication trend indicated that MRI assessment of PJIs is currently a research focus. MRI of metallic joint arthroplasty implants needs modified and advanced MRI pulse sequences to eliminate vast metal artifacts between the implant components and the surrounding soft tissues [23, 24]. High performance of 1.5 T MRI system is suited for achieving this function of substantial reductions in artifacts around metallic implants [23]. Hence, MRI is increasingly recognized as a noninvasive and valuable tool in the assessment of patients with problematic arthroplasty [19, 20, 43].
When inconsistent laboratory tests or nonspecific clinical symptoms are found, distinguishing between aseptic and septic implant failure remains imperfect and challenging [13, 14]. The clinical manifestation of PJIs includes the chronic, acute, low-grade, and high-grade implant infections. To date, there is no consistent diagnostic standard for PJIs in clinical practice [18, 19]. Among the aforementioned criteria, none recommend MRI as a diagnostic test for PJIs. In addition, there is another problem that conclusions of different studies on the diagnostic value of MRI for PJIs are not exactly the same. For example, Albano et al. considered conventional MRI features to have limited accuracy detecting total hip arthroplasty (THA) patients with PJIs [26], but other studies indicated the assessment of MRI findings facilitated the diagnosis of PJIs in THA or total knee arthroplasty (TKA) patients [27,28,29,30,31,32,33]. Possible considerations included the following: (1) very little evidence has been released on the diagnostic value of MRI for PJIs, and standardized specific MRI diagnostic features for PJIs are inconsistent and multifarious [19]. Due to the complicated anatomical structure of the hip joint, the extraction of typical MRI features on PJIs is difficult. (2) Some problems in the retrospective studies might result in serious bias risks. Most relevant articles that have been published are retrospective [26,27,28,29,30, 32, 33]. Because the retrospective nature of the study, it might lead to high selection bias and the possibility that the diagnostic value was falsely calculated. For example, the control group in some studies did not manifest characteristics of PJIs, but a possible low-virulence infection could not be excluded in a timely manner. (3) A periprosthetic mechanical stress reaction in MRI cannot be distinguished well from PJIs; in other words, a single positive MRI feature cannot be exclusive for implant infections [44]. (4) MRI is not extensively utilized to diagnose PJIs in clinical practice because of limitations such as high cost, long acquisition time, complex image postprocessing, and operator dependence.
Although MRI itself has the above inevitable limitations, the intrinsic multiparametric nature of MRI is conducive to achieving qualitative grading of bone destruction, synovitis, soft tissue edema, fluid collection, periosteal reaction, or lymphadenopathy, without ionizing radiation [25]. In this study, some MRI features, such as lamellated hyperintense synovitis, edema, fluid collection, or lymphadenopathy, were valuable diagnostic imaging findings. Diagnostic properties were found in terms of sensitivity, specificity, PPV and NPV (26.3 − 100%, 47 − 98%, 46 − 94.7% and 73.8 − 98%) with satisfactory accuracy (63.9 − 94.4%) and adequate reliability. Standardization is challenging, but a unique metric for the evaluation of PJIs as well as a standardized MRI protocol should be strenuously achieved, allowing MRI criteria of PJIs to be used in some suspected infections of patients who are difficult to diagnose.
Some inherent limitations included the following: (1) Collecting large-scale populations with PJIs in clinical practice is difficult, and only 206 patients with PJIs were included in this study. (2) The included studies showed statistical homogeneity and a high risk of bias, so it is improbable to perform a meta-analysis and categorize standardized MRI features for PJIs; (3) Due to the design limitations of the included studies, the diagnostic value of MRI for different types of PJIs was not clear. (4) Most included articles were retrospective designs which might result in serious variation and bias risk. Some larger prospective studies should be conducted to evaluate standardized MRI features for PJIs diagnosis in the future.
In conclusion, there is preliminary evidence that MRI has a noteworthy value of distinguishing suspected PJIs in patients with TKA or THA, but the definition of specific MRI features related to PJIs diagnosis lacks consensus and standardization. Large-scale studies with robust quality were required to help make better clinical decisions in the future.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–36. https://doi.org/10.1001/2012.jama.11153.
Ventura A, Macchi V, Borgo E, Legnani C. Shift to low-impact sports and recreational activities following total knee replacement. Int J Artif Organs. 2022;45:952–6. https://doi.org/10.1177/03913988221119524.
Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–97. https://doi.org/10.2106/JBJS.N.01141.
Courpied JP, Caton JH. Total hip arthroplasty, state of the art for the 21st century. Int Orthop. 2011;35:149–50. https://doi.org/10.1007/s00264-011-1207-9.
Shan L, Shan B, Graham D, Saxena A. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthr Cartil. 2014;22:389–406. https://doi.org/10.1016/j.joca.2013.12.006.
Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following unicompartmental or bicompartmental knee arthroplasty. A meta-analysis. J Arthroplasty. 1995;10:141–50. https://doi.org/10.1016/s0883-5403(05)80120-2.
Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am. 2005;87:598–603. https://doi.org/10.2106/JBJS.C.00591.
González-Sáenz-de-Tejada M, Quintana JM, Arenaza JC, Azcarate-Garitano JR, Esnaola-Guisasola PM, García-Sánchez I, Baguer-Antonio A, Bilbao-González A. Long-term health related quality of life in total knee arthroplasty. BMC Musculoskelet Disord. 2023;24:327. https://doi.org/10.1186/s12891-023-06399-6.
Qvistgaard M, Nåtman J, Lovebo J, Almerud-Österberg S, Rolfson O. Risk factors for reoperation due to periprosthetic joint infection after elective total hip arthroplasty: a study of 35,056 patients using linked data of the swedish hip Arthroplasty Registry (SHAR) and swedish Perioperative Registry (SPOR). BMC Musculoskelet Disord. 2022;23:275. https://doi.org/10.1186/s12891-022-05209-9.
Grammatico-Guillon L, Rusch E, Astagneau P. Surveillance of prosthetic joint infections: international overview and new insights for hospital databases. J Hosp Infect. 2015;89:90–8. https://doi.org/10.1016/j.jhin.2013.09.016.
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27:61–65e61. https://doi.org/10.1016/j.arth.2012.02.022.
Kapadia BH, McElroy MJ, Issa K, Johnson AJ, Bozic KJ, Mont MA. The economic impact of periprosthetic infections following total knee arthroplasty at a specialized tertiary-care center. J Arthroplasty. 2014;29:929–32. https://doi.org/10.1016/j.arth.2013.09.017.
Pellegrini A, Legnani C, Meani E. A new perspective on current prosthetic joint infection classifications: introducing topography as a key factor affecting treatment strategy. Arch Orthop Trauma Surg. 2019;139:317–22. https://doi.org/10.1007/s00402-018-3058-y.
Romanò CL, Petrosillo N, Argento G, Sconfienza LM, Treglia G, Alavi A, Glaudemans AWJM, Gheysens O, Maes A, Lauri C, Palestro CJ, Signore A. The role of imaging techniques to define a peri-prosthetic hip and knee joint infection: Multidisciplinary Consensus statements. J Clin Med. 2020;9:2548. https://doi.org/10.3390/jcm9082548.
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG. New definition for periprosthetic joint infection: from the workgroup of the Musculoskeletal infection society. Clin Orthop Relat Res. 2011;469:2992–4. https://doi.org/10.1007/s11999-011-2102-9.
Parvizi J, Gehrke T. Definition of periprosthetic joint infection. J Arthroplasty. 2014;29:1331. https://doi.org/10.1016/j.arth.2014.03.009.
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N. The 2018 definition of Periprosthetic hip and knee infection: an evidence-based and validated Criteria. J Arthroplasty. 2018;33:1309–1314e1302. https://doi.org/10.1016/j.arth.2018.02.078.
Pellegrini A, Suardi V, Legnani C. Classification and management options for prosthetic joint infection. Ann Joint. 2022;7:3. https://doi.org/10.21037/aoj-20-86.
Signore A, Sconfienza LM, Borens O, Glaudemans AWJM, Cassar-Pullicino V, Trampuz A, Winkler H, Gheysens O, Vanhoenacker FMHM, Petrosillo N, Jutte PC. Consensus document for the diagnosis of prosthetic joint infections: a joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur J Nucl Med Mol Imaging. 2019;46:971–88. https://doi.org/10.1007/s00259-019-4263-9.
Arvieux C, Common H. New diagnostic tools for prosthetic joint infection. Orthop Traumatol Surg Res. 2019;105:23–s30. https://doi.org/10.1016/j.otsr.2018.04.029.
Karchevsky M, Schweitzer ME, Morrison WB, Parellada JA. MRI findings of septic arthritis and associated osteomyelitis in adults. AJR Am J Roentgenol. 2004;182:119–22. https://doi.org/10.2214/ajr.182.1.1820119.
Hayter CL, Gold SL, Koff MF, Perino G, Nawabi DH, Miller TT, Potter HG. MRI findings in painful metal-on-metal hip arthroplasty. AJR Am J Roentgenol. 2012;199:884–93. https://doi.org/10.2214/AJR.11.8203.
Fritz J, Lurie B, Miller TT, Potter HG. MR imaging of hip arthroplasty implants. Radiographics. 2014;34:E106–132. https://doi.org/10.1148/rg.344140010.
Fritz J, Lurie B, Potter HG. MR imaging of knee arthroplasty implants. Radiographics. 2015;35:1483–501. https://doi.org/10.1148/rg.2015140216.
Talbot BS, Weinberg EP. MR imaging with metal-suppression sequences for evaluation of total joint arthroplasty. Radiographics. 2016;36:209–25. https://doi.org/10.1148/rg.2016150075.
Albano D, Messina C, Zagra L, Andreata M, De Vecchi E, Gitto S, Sconfienza LM. Failed total hip arthroplasty: diagnostic performance of conventional MRI features and Locoregional Lymphadenopathy to identify infected implants. J Magn Reson Imaging. 2021;53:201–10. https://doi.org/10.1002/jmri.27314.
Galley J, Sutter R, Stern C, Filli L, Rahm S, Pfirrmann CWA. Diagnosis of Periprosthetic Hip Joint infection using MRI with metal artifact reduction at 1.5 T. Radiology. 2020;296:98–108. https://doi.org/10.1148/radiol.2020191901.
Gao Z, Jin Y, Chen X, Dai Z, Qiang S, Guan S, Li Q, Huang J, Zheng J. Diagnostic value of MRI lamellated Hyperintense Synovitis in Periprosthetic infection of hip. Orthop surg. 2020;12:1941–6. https://doi.org/10.1111/os.12789.
Schwaiger BJ, Gassert FT, Suren C, Gersing AS, Haller B, Pfeiffer D, Dangelmaier-Dawirs J, Roski F, von Eisenhart-Rothe R, Prodinger PM, Woertler K. Diagnostic accuracy of MRI with metal artifact reduction for the detection of periprosthetic joint infection and aseptic loosening of total hip arthroplasty. Eur J Radiol. 2020;131:109253. https://doi.org/10.1016/j.ejrad.2020.109253.
Jiang MH, He C, Feng JM, Li ZH, Chen Z, Yan FH, Lu Y. Magnetic resonance imaging parameter optimizations for diagnosis of periprosthetic infection and tumor recurrence in artificial joint replacement patients. Sci Rep. 2016;6:36995. https://doi.org/10.1038/srep36995.
He C, Lu Y, Jiang M, Feng J, Wang Y, Liu Z. Clinical value of optimized magnetic resonance imaging for evaluation of patients with painful hip arthroplasty. Chin Med J (Engl). 2014;127:3876–80.
Li AE, Sneag DB, Greditzer HGt, Johnson CC, Miller TT, Potter HG. Total knee arthroplasty: diagnostic accuracy of patterns of Synovitis at MR Imaging. Radiology. 2016;281:499–506. https://doi.org/10.1148/radiol.2016152828.
Plodkowski AJ, Hayter CL, Miller TT, Nguyen JT, Potter HG. Lamellated hyperintense synovitis: potential MR imaging sign of an infected knee arthroplasty. Radiology. 2013;266:256–60. https://doi.org/10.1148/radiol.12120042.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29:372:n71. https://doi.org/10.1136/bmj.n71.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, Terwee CB. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–57. https://doi.org/10.1007/s11136-018-1798-3.
Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, Terwee CB. COSMIN Risk of Bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1171–9. https://doi.org/10.1007/s11136-017-1765-4.
Terwee CB, Mokkink LB, Knol DL, Ostelo RW, Bouter LM, de Vet HC. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res. 2012;21:651–7. https://doi.org/10.1007/s11136-011-9960-1.
Kundel HL, Polansky M. Measurement of observer agreement. Radiology. 2003;228:303–8. https://doi.org/10.1148/radiol.2282011860.
Koo TK, Li MY. A Guideline of selecting and reporting Intraclass correlation coefficients for Reliability Research. J Chiropr Med. 2016;15:155–63. https://doi.org/10.1016/j.jcm.2016.02.012.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
White LM, Kim JK, Mehta M, Merchant N, Schweitzer ME, Morrison WB, Hutchison CR, Gross AE. Complications of total hip arthroplasty: MR imaging-initial experience. Radiology. 2000;215:254–62. https://doi.org/10.1148/radiology.215.1.r00ap11254.
Schröder FF, Post CE, Wagenaar FBM, Verdonschot N. Huis In’t veld R. MRI as Diagnostic modality for analyzing the problematic knee arthroplasty: a systematic review. J Magn Reson Imaging. 2020;51:446–58. https://doi.org/10.1002/jmri.26874.
Zanetti M. The expanding role of MRI in the evaluation of Periprosthetic Hip Joint infection. Radiology. 2020;296:109–10. https://doi.org/10.1148/radiol.2020201419.
Acknowledgements
None.
Funding
This study was supported by the Natural Science Foundation of Gansu Province for Distinguished Young Scholars (22JR5RA943).
Author information
Authors and Affiliations
Contributions
CS and GB were responsible for the conception and design, data synthesis and analysis, interpretation of data and drafting the manuscript. CS and LJ screened the literature and assessed risk of bias independently. ZX contributed to conception and design, and reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shufen, C., Jinmin, L., Xiaohui, Z. et al. Diagnostic value of magnetic resonance imaging for patients with periprosthetic joint infection: a systematic review. BMC Musculoskelet Disord 24, 801 (2023). https://doi.org/10.1186/s12891-023-06926-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06926-5