Abstract
Background
Magnetic resonance cholangiopancreatography (MRCP) could aid in the diagnosis of biliary atresia, a hepatic pathology with thin, irregular or interrupted biliary ducts. There is little published evidence of MRCP appearances in normal neonates and young infants.
Objective
To assess the use of MR cholangiopancreatography in visualizing the biliary tree in neonates and infants younger than 3 months with no hepatobiliary disorder, and to assess this visibility in relationship to the child’s age, weight, and sedation and fasting states.
Materials and methods
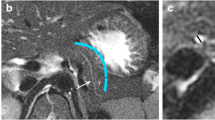
Between December 2008 and October 2010 our department performed MRI of the brain, orbits and face on 16 full-term neonates and infants. Each child was younger than 3 months (90 days) and without any hepatobiliary disorders. The children were scanned with a respiratory-gated 0.54 × 0.51 × 0.4-mm3 3-D MRCP sequence. We used a reading grid to assess subjectively the visibility of the extrahepatic bile ducts along with extrahepatic bile duct confluence. The visibility of the extrahepatic bile duct confluence was assessed against age, weight, and sedation and fasting states.
Results
The extrahepatic bile duct confluence was seen in 10 children out of 16 (62.5%). In the neonate sub-group (corrected age younger than 30 days), the MRCP was technically workable and the extrahepatic bile duct confluence was seen in four cases out of eight (50%). This visualization was up to 75% in the subgroup older than 30 days. However, statistically there was no significant difference in visibility of the extrahepatic bile duct confluence in relationship to age, weight or MRCP performance conditions (feeding, fasting or sedation).
Conclusion
The complete normal biliary system (extrahepatic bile duct confluence included) is not consistently visualized in infants younger than 3 months old on non-enhanced MRCP. Thus the use of MRCP to exclude a diagnosis of biliary atresia is compromised at optimal time of surgery.


Similar content being viewed by others
References
Hartley JL, Davenport M, Kelly DA (2009) Biliary atresia. Lancet 374:1704–1713
Benchimol EI, Walsh CM, Ling SC (2009) Early diagnosis of neonatal cholestatic jaundice: test at 2 weeks. Can Fam Physician 55:1184–1192
Moyer V, Freese DK, Whitington PF et al (2004) Guideline for the evaluation of cholestatic jaundice in infants: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 39:115–128
Petersen C, Davenport M (2013) Aetiology of biliary atresia: what is actually known? Orphanet J Rare Dis 8:128
Lykavieris P, Chardot C, Sokhn M et al (2005) Outcome in adulthood of biliary atresia: a study of 63 patients who survived for over 20 years with their native liver. Hepatology 41:366–371
Serinet M-O, Wildhaber BE, Broué P et al (2009) Impact of age at Kasai operation on its results in late childhood and adolescence: a rational basis for biliary atresia screening. Pediatrics 123:1280–1286
Chan YL, Yeung CK, Lam WW et al (1998) Magnetic resonance cholangiography – feasibility and application in the paediatric population. Pediatr Radiol 28:307–311
Guibaud L, Lachaud A, Touraine R et al (1998) MR cholangiography in neonates and infants: feasibility and preliminary applications. AJR Am J Roentgenol 170:27–31
Jaw TS, Kuo YT, Liu GC et al (1999) MR cholangiography in the evaluation of neonatal cholestasis. Radiology 212:249–256
Peng SS, Li YW, Chang MH et al (1998) Magnetic resonance cholangiography for evaluation of cholestatic jaundice in neonates and infants. J Formos Med Assoc 97:698–703
Miyazaki T, Yamashita Y, Tang Y et al (1998) Single-shot MR cholangiopancreatography of neonates, infants, and young children. AJR Am J Roentgenol 170:33–37
Norton KI, Glass RB, Kogan D et al (2002) MR cholangiography in the evaluation of neonatal cholestasis: initial results. Radiology 222:687–691
Metreweli C, So NMC, Chu WCW et al (2004) Magnetic resonance cholangiography in children. Br J Radiol 77:1059–1064
Sodickson A, Mortele KJ, Barish MA et al (2006) Three-dimensional fast-recovery fast spin-echo MRCP: comparison with two-dimensional single-shot fast spin-echo techniques. Radiology 238:549–559
Morita S, Ueno E, Masukawa A et al (2009) Comparison of SPACE and 3D TSE MRCP at 1.5 T focusing on difference in echo spacing. Magn Reson Med Sci 8:101–105
Humphrey TM, Stringer MD (2007) Biliary atresia: US diagnosis. Radiology 244:845–851
Kim MJ, Park YN, Han SJ et al (2000) Biliary atresia in neonates and infants: triangular area of high signal intensity in the porta hepatis at T2-weighted MR cholangiography with US and histopathologic correlation. Radiology 215:395–401
Edwards AD, Arthurs OJ (2011) Paediatric MRI under sedation: is it necessary? What is the evidence for the alternatives? Pediatr Radiol 41:1353–1364
Arthurs OJ, Edwards A, Austin T et al (2012) The challenges of neonatal magnetic resonance imaging. Pediatr Radiol 42:1183–1194
Bracken J, Heaslip I, Ryan S (2012) Chloral hydrate sedation in radiology: retrospective audit of reduced dose. Pediatr Radiol 42:349–354
Park WH, Choi SO, Lee HJ (1999) The ultrasonographic ‘triangular cord’ coupled with gallbladder images in the diagnostic prediction of biliary atresia from infantile intrahepatic cholestasis. J Pediatr Surg 34:1706–1710
Lee H-J, Lee S-M, Park W-H et al (2003) Objective criteria of triangular cord sign in biliary atresia on US scans. Radiology 229:395–400
Yang J-G, Ma D-Q, Peng Y et al (2009) Comparison of different diagnostic methods for differentiating biliary atresia from idiopathic neonatal hepatitis. Clin Imaging 33:439–446
Esmaili J, Izadyar S, Karegar I et al (2007) Biliary atresia in infants with prolonged cholestatic jaundice: diagnostic accuracy of hepatobiliary scintigraphy. Abdom Imaging 32:243–247
Sevilla A, Howman-Giles R, Saleh H et al (2007) Hepatobiliary scintigraphy with SPECT in infancy. Clin Nucl Med 32:16–23
Nwomeh BC, Caniano DA, Hogan M (2007) Definitive exclusion of biliary atresia in infants with cholestatic jaundice: the role of percutaneous cholecysto-cholangiography. Pediatr Surg Int 23:845–849
Meyers RL, Book LS, O’Gorman MA et al (2004) Percutaneous cholecysto-cholangiography in the diagnosis of obstructive jaundice in infants. J Pediatr Surg 39:16–18
Ohnuma N, Takahashi T, Tanabe M et al (1997) The role of ERCP in biliary atresia. Gastrointest Endosc 45:365–370
Ohnuma N, Takahashi H, Tanabe M et al (1997) Endoscopic retrograde cholangiopancreatography (ERCP) in biliary tract disease of infants less than one year old. Tohoku J Exp Med 181:67–74
Poddar U, Thapa BR, Bhasin DK et al (2001) Endoscopic retrograde cholangiopancreatography in the management of pancreaticobiliary disorders in children. J Gastroenterol Hepatol 16:927–931
Petersen C, Meier PN, Schneider A, et al. (2009) Endoscopic retrograde cholangiopancreaticography prior to explorative laparotomy avoids unnecessary surgery in patients suspected for biliary atresia. J Hepatol 51:1055–1060
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siles, P., Aschero, A., Gorincour, G. et al. A prospective pilot study: Can the biliary tree be visualized in children younger than 3 months on Magnetic Resonance Cholangiopancreatography?. Pediatr Radiol 44, 1077–1084 (2014). https://doi.org/10.1007/s00247-014-2953-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-014-2953-9