Abstract
Background Cardiac magnetic resonance imaging (MRI) is an important diagnostic tool for congenital heart disease (CHD), as reflected by class 1 recommendations for the use of cardiac MRI by various consensus panels. However, little is known about the safety and clinical utility of cardiac MRI for these critically ill infants with CHD, whose further management cannot be directed by echocardiography. This study aimed to assess the safety, the potential hemodynamic side effects, and the clinical benefits of cardiac MRI for infants with complex CHD during their intensive care unit stay. Methods Infants referred from the pediatric cardiac intensive care unit (PCICU) to the authors’ cardiac MRI program in the past 2 years were retrospectively analyzed using the electronic chart system available at their institution. Data collected included age, diagnosis, inotropic support, urine output, diuretic medication, body temperature and lactate levels, length of MRI examination, adverse effects during and after the procedure, clinical implications of MRI, length of stay in the PCICU, and mean blood pressure and heart rate before, during, and after MRI. Results Among 592 patients in the past 2 years, 20 (3.4%) were referred for MRI testing during their stay in the PCICU. The mean age of the infants was 4.8 ± 3.2 months. Four of the patients were neonates, and eight were postoperative patients. Intracardiac malformations were present in 16 of the infants, vascular rings causing tracheal stenosis in 3 patients, and cardiomyopathy in 1 patient. The mean stay in the PCICU was 28 ± 43 days. Eight of the infants were ventilated, with a mean fraction of inspired oxygen (FiO2) of 0.30 ± 0.15. Four were receiving inotropic support. All the nonventilated children were intubated for the MRI and extubated in the MRI laboratory. The mean duration of the MRI (door-to-door time) was 110 ± 27 min. All except one patient were hemodynamically stable, and no increase in catecholamine support was necessary during or after the scans. A 10-month-old girl receiving inotropic support needed a single dose of epinephrine due to a short episode of bradycardia after a breathhold for a contrast agent MRI angiography. Mean body core temperature at arrival to the PCICU was 36.8 ± 0.7°C. The mean serum lactate level after the MRI was 1.2 ± 0.4 mmol/l. The mean blood pressure and heart rate before, during, and after MRI were unchanged. The mean diuresis on examination day was insignificantly lower (2.4%) than the day before with unchanged medication (5.09 ± 1.58 vs 5.53 ± 1.77 ml/kg/h). For 14 (70%) of the 20 patients, surgical or catheter interventional procedures were initiated based on novel MRI information. Conclusion Cardiac MRI can be performed safely with low risk and limited hemodynamic changes for infants during their stay in the PCICU. Cardiac MRI provides key information for invasive management decisions in this subset of patients.
Similar content being viewed by others
Magnetic resonance imaging (MRI) is an important diagnostic tool for congenital heart disease (CHD), as reflected by class 1 recommendations for the use of cardiac MRI by various consensus panels [3, 6, 12]. The use of cardiac MRI for infants before surgery or after cardiac surgery has been limited in the past due to the important role of echocardiography for this age group, the potential hazards during the transport of these sometimes critically ill children, and the challenging MRI environment, which carries several inherent risks [9, 14, 15].
Computed tomographic (CT) angiography, cardiac catheterization, and angiography are important and well-established alternatives to MRI. However, these diagnostic methods are invasive, causing significant exposure to ionizing radiation.
On the other hand, MRI provides a unique diagnostic capability for assessing all thoracic organs in neonates and infants with respiratory problems (e.g., patients with vascular rings and slings) [17]. Furthermore, functional cardiac MRI including flow measurements, volumetric analysis of ventricular size and function, and quantification of valvular incompetence is increasingly used, especially in complex cases [13].
Therefore, this study aimed to assess retrospectively the safety and any potential unwanted hemodynamic alteration during cardiac MRI in this setting. In addition, it sought to estimate the clinical impact of any novel MRI information on management decisions for this vulnerable patient group.
Materials and Methods
We retrospectively enrolled all infants from our pediatric cardiac intensive care unit (PCICU) referred to the CHD-MRI unit from January 2005 to December 2006. A total of 20 patients with pre- and postoperative congenital heart defects were identified (Table 1). All the patients were referred for further diagnostic evaluation by MRI because either transthoracic echocardiography (18 patients) or cardiac catheterization (2 patients) was unable to visualize the relevant cardiovascular morphology sufficiently. All the patients were in sinus rhythm.
Transport from the PCICU to the MRI laboratory, located on the same floor, was performed by the PCICU staff. Nonventilated infants were electively intubated in the MRI unit and anesthetized for MRI, then subsequently extubated in the MRI laboratory. Anesthesia was performed by experienced cardiac anesthetists with intravenous introduction and inhalation anesthesia using volatile anesthetics.
Complete hemodynamic monitoring was performed during the scans including anesthetic vapor concentrations, end-tidal carbon dioxide analysis, invasive arterial and central venous pressures, noninvasive blood pressures, electrocardiography (ECG), and pulse oximetry. All examinations were performed on a standard 1.5-T whole-body MR scanner (Philips Intera; Best, The Netherlands) using a two-element phased-array head-neck or a five-element cardiac coil. Analysis was performed using our electronic patient documentation system in the PCICU that allows review of all hemodynamic data, respirator settings, and medications.
Data collected included age, diagnosis, length of stay in the PCICU, presence of indwelling catheters or drains, inotropic support, urine output, diuretic medication, body temperature, and lactate levels. Mean arterial blood pressures and heart rates were compared before, during, and after MRI. We documented the length of the MRI (door-to-door time) including the time needed for intubation in the MRI laboratory and positioning of the children for the scan as well as intra- or postprocedural complications.
Temperature and lactate levels were measured immediately after arrival back at the PCICU. Catecholamine dosage, diuresis, and the amount of diuretics were analyzed the day after the MRI examination. We also reviewed the subsequent clinical course of the patients for nosocomial infections and therapeutic implications derived from the MRI results.
Results
The study investigated 20 infants (13 boys and 7 girls) representing 3.4% of all patients (n = 592) studied in our CHD-MRI program over the last 2 years. The mean age was 4.8 ± 3.2 months (range, 6 days to 12 months; median, 4.9 months), and the mean weight was 5.8 ± 1.7 kg (range, 3.2–9.3 kg; median, 6 kg).
Of the 20 infants, 8 had undergone surgery for congenital heart defects. Intracardiac malformations were present in 16 of the infants and vascular rings causing tracheal stenosis in 3 patients. One 4-month-old boy was referred because of cardiomyopathy (Table 1). Of the 20 patients, 4 needed inotropic support at the time MRI was requested, and 8 were ventilated with a mean fraction of inspired oxygen (FiO2) of 0.3 ± 15 (range, 0.21–0.7).
Monitoring during transport from the PCICU to the MRI lab, a 5-min walking distance on the same floor, showed no significant differences in the vital parameters. The mean examination time in the MRI lab was 110 ± 27 min (range, 77–170 min; median, 104 min), including the time required to intubate the 12 nonventilated infants and position the patients on the MRI table, which was time consuming, especially for the 5 patients with arterial and central venous lines and the 2 patients with postoperative drains.
During the MRI scan procedures, all the patients except one were hemodynamically stabile, and no increase in intravenous catecholamine support was necessary. The mean blood pressure before MRI was 53 ± 7 mmHg (range, 38–65 mmHg; median, 55 mmHg). During the scans, the mean blood pressure was 52 ± 7 mmHg (range, 38–63 mmHg; median, 51 mmHg), and after arrival at the PCICU, it was 54 ± 6 mmHg (range, 37–65 mmHg; median, 55 mmHg). The heart rate changes before, during, and after the procedure were of no significance. The heart rate per minute was 139 ± 13 bpm (range, 120–180 bpm; median, 140 bpm) before the MRI, 125 ± 16 bpm (range, 100–170 bpm; median, 124 bpm) during the MRI, and 140 ± 13 bpm (range, 120–180 bpm; median, 140 bpm) after the MRI.
A 10-month-old girl (patient 9) with a double-outlet right ventricle, transposition of the great arteries, and chromosomal anomaly requiring a milrinone intravenous infusion needed a single dose (0.05 mg) of epinephrine due to a short episode of relative bradycardia (80 bpm) after one 15-s breathholding episode for a contrast agent–based angiography, which was the last scan in her examination. Here blood pressure, however, remained stable, and her bradycardia resolved with ventilation and epinephrine within 30 s.
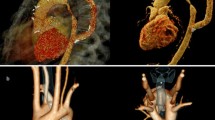
All other examinations were completed successfully with the ability to produce diagnostic images in all cases. An example of the image quality is given in Fig. 1 (patient 14).
Patient 14 with tracheal stenosis due to a double aortic arch with an atretic left anterior part. (a) Transverse turbo spin-echo images displaying the tracheal stenosis by the right aortic arch. (b) Three-dimensional volume–rendered reconstruction of the double aortic arch with the atretic left anterior arch. Note that each arch gives rise to the ipsilateral common carotid and subclavian artery
No indwelling catheters or drains were accidentally dislocated during transport or in the MRI laboratory. The mean body core temperature after return to the PCICU was 36.8 ± 0.7°C (range, 35.8–38.5°C; median, 36.9°C). The mean serum lactate level was 1.2 ± 0.4 mmol/l (range, 0.8–1.8 mmol/l; median, 1.2 mmol/l).
The mean diuresis on the examination day was insignificantly lower than the day before with unchanged medication (5.09 ± 1.58 vs 5.53 ± 1.77 ml/kg/h). The mean stay in the PCICU was 28 ± 43 days (range, 1–164 days; median, 8 days). No associated nosocomial infections were recorded up to 14 days after the MRI.
For 14 (70%) of the 20 patients, operative or catheter-interventional procedures were initiated after the MRI result. One 3-month-old baby was listed for heart transplantation (Table 2), and only one additional diagnostic direct heart catheterization (patient 20) was performed after the MRI. Four patients (patients 3, 9, 11, and 13) died due to their congenital heart disease during the study period.
Discussion
Cardiac MRI has become a cornerstone for diagnostic imaging in congenital heart disease. Anatomic delineation of all thoracic organs and functional assessment of blood flow and myocardial cardiac function are possible for all age groups [2, 5, 16]. One major advantage of cardiac MRI is the lack of radiation, which is especially important for children. One major disadvantage of cardiac MRI is that it is slow, which is especially important in the imaging of critically ill patients.
Infants requiring intensive care are particularly vulnerable because of their impaired cardiac or respiratory function during transport to imaging sites with its potential additional hazards [19]. One recent study delineated a low overall rate of adverse events during cardiovascular magnetic resonance for congenital heart disease, with the highest rate of adverse events for patients from the intensive care unit [4].
The current study demonstrated that cardiac MRI for the infant in the intensive care unit, in an adequate setting, has no delayed hemodynamic effects, as indicated by the evaluated parameters including serum lactate, diuresis, and the amount of diuretics up to 24 h after the MRI. Although this approach may reflect our institutional approach, to some extent, the significant clinical value of cardiovascular MRI for sick infants with CHD is increasingly recognized by other investigators [1, 10].
Cardiac MRI appeared to have no significant unwanted hemodynamic effects, except for one infant, a 10-month-old girl receiving inotropic support who required a single dose of epinephrine after a breathhold scan of 15 s resulting in relative bradycardia, which resolved within 30 s. This patient’s blood pressure remained stable throughout the procedure and the bradycardia event. This episode emphasizes the importance of complete hemodynamic monitoring during cardiac MRI for sick children and the close cooperation required between the anesthetist and radiologist, especially during breathhold scans.
Transport of a critically ill infant may involve significant risks. Therefore, hemodynamic stability should be optimized, and monitoring during transport is crucial [20]. In our study, transport from the PCICU to the MRI and back was within a 5-min walking distance on the same floor. The transport was carried out by one experienced pediatric cardiologist, an intensivist, and one or two nurses from the PCICU. Because many congenital heart defects cause an imbalance between systemic and pulmonary perfusion, special care was taken not to hyperventilate patients during transport.
No complications occurred during transport in our study, underscoring the importance of exact preparation for such transports. In all cases, the patient was assessed on the PCICU ward the day before MRI by the pediatric cardiologist responsible for our congenital cardiac MRI program.
Complete hemodynamic monitoring during the examinations including end-tidal carbon dioxide analysis, invasive arterial and central venous pressures, noninvasive blood pressures, ECG, and pulse oximetry allowed the treating physicians to adapt anesthesia continuously to the hemodynamic changes. Heart rate, blood pressure, and ventilation during anesthesia did not differ from those of the previous hemodynamic situation.
Joint meticulous planning and tailoring of the examination to the patient’s hemodynamic and respiratory status is known to be very important, especially with small children [11]. At our institution, this is facilitated by performance of the scans by pediatric cardiologists in close collaboration with our radiologists.
All examinations could be completed successfully with good image quality during a mean examination time of 110 ± 27 min from the patient’s arrival, including intubation, positioning, imaging, and return to the PCICU. This corresponds to the reported time needed for infant cardiac imaging by other institutions [16]. Duration of these tests is significant due to anesthetic management during the examination on the one hand and due to technical aspects of infant cardiac imaging on the other hand, in which higher heart rates and smaller vascular structures must be adapted to time-consuming navigator techniques or multiple signal averages [8].
No nosocomial infections, especially ventilator-associated pneumonia, were recognized up to 14 days after the examinations. Although the number of patients in this study was small, our strategy of elective ventilation for MRI appeared to be a wise approach.
For 14 of the 20 infants, operative or catheter interventional procedures were initiated after the MRI result during the same hospital stay. One 3-month-old baby was listed for heart transplantation. Details for MRI indications, new findings by MRI, and clinical consequences are presented in Table 2.
The noninvasive nature of MRI and its great clinical impact on management decisions render cardiac MRI particularly attractive for patients with impaired hemodynamics for whom direct cardiac catheterization poses additional risks such as arrhythmias, infections, and contrast agent load [17]. Alternatively, cardiac CT certainly is an important method, particularly for delineating extracardiac vessel malformations and airway problems. Its great advantage is its unique speed, with acquisition times of a few seconds. Obviously, this is most important with imaging procedures for unstable patients. However, CT is limited largely to morphologic assessment because no hemodynamic data can realistically be expected from CT with small children. Moreover, the increase in radiation sensitivity up to 10-fold for smaller children is particularly relevant for infants with complex CHD, for whom repeated X-ray-based procedures may be used [18].
Therefore, all efforts should be made to minimize the cumulative risk for the development of radiation-induced cancer [7, 18]. For this reason, cardiovascular MRI is considered the method of choice by many institutions when transthoracic echocardiography is inconclusive and the patient is stable enough to undergo a longer investigation under general anesthesia.
Conclusion
We reviewed the infant patients from our PCICU undergoing cardiac MRI for hemodynamic consequences and intraprocedural complications, as well as the subsequent clinical value of the investigations. No acute or delayed hemodynamic adverse effects and no significant intraprocedural complications occurred. For 70% of our patients, surgical or catheter-based interventional procedures were initiated on the basis of the novel MRI information. This indicates that in an adequate setting, cardiovascular MRI is safe and has important management implications even for this highly vulnerable patient group.
References
Brown DW, Gauvreau K, Powell AJ et al (2007) Cardiac magnetic resonance versus routine cardiac catheterization before bidirectional Glenn anastomosis in infants with functional single ventricle. Circulation 116:2718–2725
Chung T (2000) Assessment of cardiovascular anatomy in patients with congential heart disease by magnetic resonance imaging. Pediatr Cardiol 21:18–26
Constantine G, Shan K, Flamm SD et al (2004) Role of MRI in clinical cardiology. Lancet 363:2162–2171
Dorfman AL, Odegard KC, Powell AJ et al (2007) Risk factors for adverse events during cardiovascular magnetic resonance in congenital heart disease. J Cardiovasc Magn Reson 9:793–798
Fogel MA (2000) Assessment of cardiac function by magnetic resonance imaging. Pediatr Cardiol 21:59–69
Hendel RC, Patel MR, Kramer CM et al (2006) ACCF/ACR/SCCT/SCMR/ASN-/NASCI/SCAI/SIR appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging. J Am Coll Cardiol 48:1475–1497
Huda W (2007) Radiation doses and risks in chest computed tomography examinations. Proc Am Thorac Soc 4:316–320
Kellenberger CJ, Yoo S-J, Valsangiacomo-Büchel ER (2007) Cardiovascular MR imaging in neonates and infants with congenital heart disease. RadioGraphics 27:5–18
Malviya S, Voepel-Lewis T, Eldevik OP et al (2000) Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaest 84:743–748
Muthurangu V, Taylor AM, Hedge SR et al (2005) Cardiac magnetic resonance imaging after stage I Norwood operation for hypoplastic left heart syndrome. Circulation 112:3256–3263
Odegard KC, Dinardo JA, Tsai-Goodman B et al (2004) Anaesthesia considerations for cardiac MRI in infants and small children. Pediatr Anesth 14:471–476
Pennell DJ, Sechtem UP, Higgins CB et al (2004) Clinical indications for cardiovascular magnetic resonance: consensus panel report. Eur Heart J 25:1940–1965
Samyn MM (2004) A review of the complementary information available with cardiac magnetic resonance imaging and multislice computed tomography (CT) during the study of congenital heart disease. Int J Cardiovasc Imaging 20:569–557
Smith I, Fleming S, Cernaianu A (1990) Mishaps during transport from the intensive care unit. Crit Care Med 18:278–281
Tobin JR, Spurrier EA, Wetzel RC (1992) Anaesthesia for critically ill children during magnetic resonance imaging. Br J Anaesth 69:482–486
Tsai-Goodman B, Geva T, Odegard KC et al (2004) Clinical role, accuracy, and technical aspects of cardiovascular magnetic resonance imaging in infants. Am J Cardiol 94:69–74
Vitiello R, McCrindle BW, Nykanen D et al (1998) Complications associated with pediatric cardiac catheterization. J Am Coll Cardiol 32:1433–1440
Vock P (2002) CT radiation exposure in children: consequences of the American discussion for Europe. Radiologe 42:697–702
Wallen E, Venkataraman ST, Grosso MJ (1995) Intrahospital transport of critically ill children. Crit Care Med 23:1588–1595
Weg JG, Haas CF (1998) Safe intrahospital transport of critically ill ventilator-dependent patients. Chest 96:631–635
Acknowledgments
S. Sarikouch was supported in part by the Competence Network for Congenital Heart Defects funded by the Federal Ministry of Education and Research (BMBF), grant FKZ 01G10210.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarikouch, S., Schaeffler, R., Körperich, H. et al. Cardiovascular Magnetic Resonance Imaging for Intensive Care Infants: Safe and Effective?. Pediatr Cardiol 30, 146–152 (2009). https://doi.org/10.1007/s00246-008-9295-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9295-z